Treatment
Treatment for children with malignancies includes chemotherapy, radiotherapy, surgery, stem cell/bone marrow rescue and transplantation, and novel therapies such as gene therapy. Children may receive one or a combination of these treatments dependent on their underlying diagnosis.
Chemotherapy
Chemotherapy is the most common treatment for paediatric malignancies. Cancer is a disease of uncontrolled cell growth. Chemotherapy is a drug which has anti-cancer or cytotoxic (cell-killing) properties and can be given intravenously or orally dependent on the diagnosis and treatment protocol. Chemotherapy kills or damages cells at different stages in the cell cycle, with different chemotherapy effective at different stages. In order to fully understand chemotherapy it is essential to have an understanding of the cell cycle, cell replication and division of the healthy cell and readers are advised to refer to an anatomy and physiology textbook of their choice (Selwood et al. 2009). The side-effects (which may be fatal) are related to the inability of chemotherapy to distinguish between healthy cells and malignant cells, therefore having a systemic effect on the whole body, with damaging effects on all cells in the bone marrow (platelets, red blood cells and white cells).
Radiotherapy
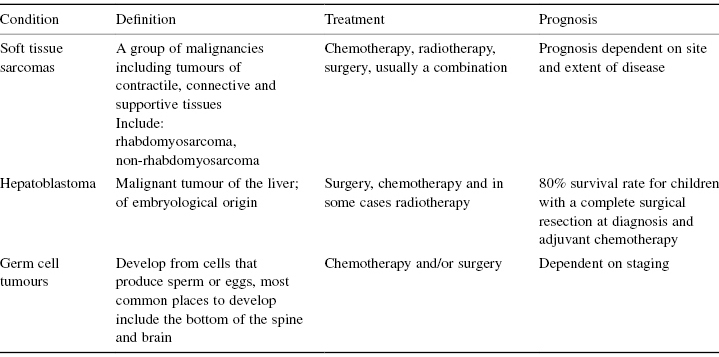
Radiotherapy is often used as a treatment for paediatric malignancies, and can be used individually or with chemotherapy or surgery, dependent on the child’s diagnosis and treatment protocol (Hopkins 2008). Radiotherapy is commonly used in the treatment of Ewing’s sarcoma, rhabdomyosarcoma, Hodgkin’s disease, neuroblastoma, Wilms’ tumour and leukaemia with central nervous system involvement (see Table 11.1); however it can also be used for children receiving palliative care to control the symptoms of progressive disease (Hopkins 2008). Radiotherapy works using high-energy rays which kill malignant cells by causing internal damage to the cells’ components or molecules (Cancer Research UK 2007). The side-effects are dependent on the area of the body receiving radiotherapy and can be divided into long-term and short-term side-effects. Healthy tissues react differently to radiotherapy dependent on the proliferation rate of the tissue, for example skin, bone marrow and hair follicles proliferate quickly and therefore effects can be seen quickly; organs such as the brain and kidneys proliferate at a slower pace, therefore cellular damage occurs at a later stage (Hopkins and Scott 2008).
Surgery
Surgical treatment of malignancy has changed over the years in paediatric oncology from often being an isolated treatment to now playing an integral part of the overall management of a child with cancer alongside other modes of treatment such as chemotherapy and/or radiotherapy (Hollis et al. 2008). Surgery is commonly used in conjunction with other treatments for osteosarcoma, neuroblastoma, Ewing’s sarcoma, hepatoblastoma, Wilms tumour and brain tumours. Children with malignant brain tumours often require surgery initially when they are diagnosed; however other solid tumours such as osteosarcoma and Ewing’s sarcoma receive initial chemotherapy in an attempt to reduce the tumour prior to surgery. This also allows assessment to the response of chemotherapy from the histology of the removed tumour (Selwood et al. 2009). Children requiring surgery are usually cared for on a general surgical ward, have a planned intensive care bed and in unusual cases may require an emergency intensive care bed due to the complications of surgery. As a general rule children having surgery are in relatively good condition as bone marrow recovery is often essential prior to surgery, therefore children require the skills of general surgical and intensive care nurses as opposed to the skills of an oncology nurse.
Novel Therapies
Novel therapies are emerging in the treatment of paediatric malignancies. These include molecular-targeted therapies, gene therapy and tumour vaccines. Molecular-targeted therapies are the therapy which really seems to be increasing within paediatric oncology and works by inhibiting growth of malignant cells without damaging surrounding healthy cells, which is very encouraging (Selwood et al. 2009).
Bone Marrow and Stem Cell Transplantation
Bone marrow and stem cell transplantation is associated with high levels of morbidity for many reasons. Bone marrow or stem cell transplantation involves bone marrow or stem cells from a donor being transplanted by intravenous infusion. Before the recipient receives the transplanted cells they are given high doses of chemotherapy with or without total body irradiation in an attempt to wipe out the immune system and associated disease completely (Selwood et al. 2009). An allogeneic transplant involves receiving a transplant from another source, either a relative or an unrelated donor, dependent on the suitability of the match (Bennett-Rees and Hopkins 2008a; Selwood et al. 2009), and usually occurs in children with high-risk leukaemia, relapsed leukaemia or children with particular haematological conditions (Selwood 2008a).
Autologous transplantation involves cells being harvested from the patient and then reinfused following high doses of myeloablative chemotherapy (Bennett-Rees and Hopkins 2008a). This procedure is often referred to as a stem cell/bone marrow rescue and is predominantly used for children with solid tumours, commonly children with stage 4 neuroblastoma (Selwood 2008a).
The side-effects of a bone marrow/stem cell transplant are severe and life-threatening, due to the nature of high-dose chemotherapy and the prolonged period of neutropenia (Selwood 2008a). Nursing care focuses on prevention of infection, through barrier nursing, mouth care, dietary restrictions, skin care and infection screening (Bennett-Rees and Hopkins 2008c). Stem cell transplantation is associated with high mortality rates, with multiple infectious and non-infectious causes, often requiring support of an ICU (Pene et al. 2006). Children are at high risk of infection due to the prolonged period of neutropenia, veno-occlusive disease as a result of conditioning chemotherapy and other side-effects related to oncological treatments mentioned in this chapter. An allogeneic transplant is often further complicated by the presence of graft-versus-host disease (GVHD) (Pene et al. 2006). GVHD involves the donor’s T-cells attacking the recipient’s tissues and can be fatal. GVHD can be acute or chronic and can involve many systems in the body including skin, gastrointestinal tract and liver (Bennett-Rees and Hopkins 2008b). GVHD can have a positive effect due to its ability to recognise and eliminate any malignant cells seen; this is known as graft versus leukaemia (Bennett-Rees and Hopkins 2008b). GVHD is common during transplantation and may require further immunosuppressive therapy such as steroids, which in turn increase the risk of mortality (Pene et al. 2006). Although mortality remains high for patients following a bone marrow/stem cell transplant, improvements in supportive care in the ICU have significantly improved the survival of haemato-oncology patients (Naeem et al. 2006).
So, the question remains, are oncology children different from other children who are looked after in the ICU? Immunosuppression is often the most significant difference. Children with cancer who are admitted to the ICU, with the exception of children who have had planned surgery, are often neutropenic and severely immunocompromised following chemotherapy or bone marrow/stem cell harvest. It is important, however, to be aware that although children post-surgery may not be neutropenic at that time, if they have had fairly recent chemotherapy they may still have a degree of immunosuppression.
It is important to remember when looking after a child who is receiving or who has received chemotherapy that as well as the immune system being damaged, the physiological response to infection is not as effective and the physical barriers may be damaged. This damage (e.g. to the skin, gastrointestinal tract, etc.) is often due to side-effects of chemotherapy such as mucositis. The normal responses to infection are not always present as a result of chemotherapy and/or steroids, for example a child may have a serious life-threatening infection without a fever.
Historically, patients with cancer admitted to the ICU were associated with a very high mortality rate. Over recent years, however, there is limited evidence to support such a statement (Farquhar-Smith and Wigmore 2008), particularly in the paediatric population. It has been suggested that the cancer diagnosis itself is not the risk factor in survival, but the acute disturbance in the physiological processes that has a detrimental effect on overall outcome (Farquhar-Smith and Wigmore 2008). Differing risk factors are suggested as being risk factors in oncology patients on the ICU, one of which is mechanical ventilation, which is strongly linked with mortality (Soares et al. 2005). It has been suggested that there is a link between survival of oncology children on the ICU and the use of inotropes, with the amount of inotropes having a negative effect on overall survival (Keengwe et al. 1999). It has also been documented that gram-negative infections, in particular Pseudomonas and Klebsiella, are linked with high levels of ICU admission and death (Adamski et al. 2008). The major differences in caring for children with a malignancy on the ICU are often related to the treatment the child has received in the past or are currently receiving and the potential side-effects. Side-effects, such as prolonged neutropenia and severe weight loss, have a huge impact on the body’s ability to recover from illness and side-effects. Gaining an understanding of chemotherapy and its side-effects will enable the reader to have an awareness of the anticipated problems and predicted side-effects of children with a malignancy.
Literature also suggests that the earlier children are admitted to an ICU the better the survival outcome in critically ill cancer patients (Thiery et al. 2005). Children with a malignancy are looked after in specialised paediatric oncology units, from where children are often moved to ICU late on, due to the specialist care they receive on the oncology unit and as it is often a risk to move such children, particular children post-bone marrow or stem cell transplant, being nursed in strict isolation.
It is important to consider that the care of the oncology patient within an ICU environment has the added dimension of the complex ethical issues faced by medical and nursing staff (Collins and Mozdzierz 1996). Nursing staff may struggle with often divergent views and different clinical perspectives, particularly relating to perception of treatment effectiveness and prognosis between intensivists, oncologists and occasionally other specialists (Kaplow 2001).
Conditions Related to the Disease Process
In this section we discuss conditions specifically related to the disease process, at diagnosis, relating to disease progression or as a direct result of initial treatment.
Superior Vena Cava Syndrome
The superior vena cava is a major blood vessel, which drains venous blood from the head, neck, upper extremities and upper thorax, back to the heart (Kallab 2005). Superior vena cava syndrome is an obstruction of venous blood flow though the SVC (Selwood et al. 2009). The majority of cases of SVC syndrome are seen in patients with a malignant disease; in fact up to 90% of cases involve patients with a malignancy (Creel et al. 2008). The frequency of SVC syndrome in the paediatric population is unknown due to the lack of published data; however it is known that cases of the syndrome are caused by central venous catheter thrombosis and more commonly as a direct result of a tumour compressing the SVC (Creel et al. 2008). Tumour compression of the SVC can occur at diagnosis or relapse/disease progression and can be caused by many tumours including T-cell leukaemia (Hon et al. 2005), non-Hodgkin’s lymphoma, Hodgkin’s lymphoma, chest tumours and any malignant process causing a mediastinal mass (Selwood et al. 2009).
Signs and symptoms are directly related to the increased venous pressure in the upper part of the body (Wilson et al. 2007), resulting in oedema in the upper extremities and face, engorgement of the face, subconjunctival haemorrhage and protruding eyes (Beeson 2007). Oedema leads to compromise of the pharynx or larynx, resulting in a cough, dyspnoea, stridor and dysphagia, with cerebral oedema leading to confusion, headaches and, in some cases, coma (Wilson et al. 2007). Haemodynamic compromise can also occur due to decreased venous return (Wilson et al. 2007). Onset can be insidious but can happen very quickly leading to acute respiratory distress (Selwood et al. 2009), with the most common symptom development being over a two-week period (Wilson et al. 2007).
Diagnosis
Diagnosis can be established through imaging such as chest X-ray or CT scan, however a diagnosis is often established through clinical examination and an accurate history-taking (Haut 2005; Kallab 2005).
Management
Management of SVC syndrome has a two-pronged approach, involving treatment of the malignant condition and managing and relieving the symptoms of the obstruction itself (Wilson et al. 2007). Diagnosing the underlying aetiology of the tumour is essential to ensure appropriate treatment is commenced as quickly as possible (Kennebeck 2005). Adjunctive therapy such as steroids and diuretics are commonly used in relieving the symptoms (Beeson 2007). Steroids are also very effective in reducing tumour burden in patients with non-Hodgkin’s lymphoma, and thereby reducing the obstruction (Wilson et al. 2007). The nursing care of a child with SVC syndrome is a challenge (Hon et al. 2005), with children often requiring immediate intubation and ventilation when the syndrome is suspected (Haut 2005). Psychological care is essential in caring for children with SVC syndrome, as the child and family are dealing with an acute, life-threatening episode and trying to deal with the prospect of ongoing cancer treatment, with limited knowledge (Selwood et al. 2009).
Spinal Cord Compression
Spinal cord compression in children is a medical emergency and a serious complication of a malignant process (Haas 2003). Children with spinal cord compression may be looked after in the intensive care environment and are associated with considerable mortality and morbidity (Joseph and Tayar 2005; Osowski 2002). Spinal cord compression in the paediatric population is usually associated with a variety of malignant diseases at diagnosis, including lymphoma, Ewing’s sarcoma, osteosarcoma, leukaemia, neuroblastoma, posterior fossa brain tumours and with metastatic disease (Haut 2005; Selwood 2008b). However, it can also cause problems in the palliative stage of a malignant disease.
Spinal cord compression is a compression of the intrathecal sac caused by a mass in the epidural space (Quinn and DeAngelis 2000). Malignant invasion of the spinal cord can occur at any point along the 26 vertebrae (Flounders and Ott 2003) and can cause irreversible neurological damage if not treated promptly (Selwood 2008b), therefore imaging is crucial in order to diagnose the condition and ensure speedy and appropriate treatment.
Signs and Symptoms
Signs and symptoms are related to the location of tumour and the extent of spinal cord compression (Marrs 2006). Back and neck pain is an early complaint (Slocombe and Boynes 2005), and pain may progress from a discomfort into weakness in limbs, autonomic dysfunction, loss of sensation and occasionally paralysis (Osowski 2002; Selwood 2008b).
Diagnosis
Diagnosis of spinal cord compression involves a thorough physical examination, including a neurological examination, an accurate history and an MRI scan (Kwok et al. 2006).
Management
Options for the treatment of children with spinal cord compression include decompression surgery, radiotherapy and chemotherapy. Dexamethasone is commonly used to reduce swelling and inflammation and therefore giving temporary pressure relief (Haas 2003). Spinal cord compression is one of the few situations in which chemotherapy is administered as an emergency (Selwood 2008b). Radiotherapy is commonly given for spinal cord compression in the palliative stages of care.
As with superior vena cava syndrome it is important when nursing these children to give consideration to psychological care and education, as these children and their families may have to deal with an acute oncological event, as well as the prospect of further treatment and the possibility of long-term neurological problems (Selwood 2008b). Nursing management focuses on assessing ongoing neurological function and pain relief (Flounders and Ott 2003), as well as preventing and treating associated complications such as sensory-motor deficits and immobility (Wilkes 1999).
Tumour Lysis Syndrome
Children who are most at risk of tumour lysis syndrome (TLS) usually have bulky disease with a large tumour burden (e.g. B-cell or T-cell lymphomas) or have a high white cell count leukaemia. It is sometimes seen in children with solid tumours. TLS can occur before treatment is commenced but is most common 12–72 hours after the initiation of treatment (Rheingold and Lange 2006). TLS consists of several metabolic abnormalities that results from the rapid death of tumour cells and can be fatal. There is a resulting increase in the breakdown products of uric acid, phosphate and potassium, and the symptoms will relate to these changes.
Prevention and early recognition of any problems are vital. An awareness of the children likely to encounter this problem is important with relevant medical personnel involved fully aware of the situation. Aggressive hydration, without added potassium, at 3 l/m2 of the body surface area should be started before treatment is commenced and during initial chemotherapy. A renal ultrasound performed before treatment is commenced will also establish whether there are any abnormalities that may compromise renal function. Frequent observation of the renal function should be undertaken for early recognition of abnormalities followed by prompt treatment, which may be needed 4–6 hourly. An accurate fluid balance, twice daily weights and 4-hourly blood pressures also help assess and highlight any potential problems promptly. Although rare, leukapheresis has been performed to reduce really high white cell counts before treatment is commenced (Porcu et al. 2000).
There are two medications that are used to help promote the breakdown of uric acid: allopurinol and recombinant urate oxidase. Allopurinol is administered orally and works by inhibiting the enzyme xanthine oxidase which is necessary for the production of uric acid. It does not reduce any uric acid that is already present (Jeha 2001). Recombinant urate oxidase is administered intravenously and works by catalysing the conversion of uric acid into allatonin, which is more easily excreted in the urine with less potential for precipitation (Jeha 2001). Any blood samples of children who are on recombinant urate oxidase need to be put on ice immediately because if they are transported at room temperature the uric acid in the sample degrades and the results will give a false low (Lim et al. 2003). Allopurinol is used routinely in all children who have a risk of TLS, whereas recombinant urate acid tends to be used in children who present with a large tumour burden or high white cell count or with a uric acid that is increasing throughout treatment.
Even if these steps are taken, some children will end up with metabolic abnormalities that will need treatment. Some will develop renal failure that will require haemodialysis to help reduce the plasma uric acid, high levels of potassium and high phosphate. Hyperkalaemia will need to be corrected by decreasing potassium intake, facilitating the shift of extracellular potassium and excretion. Correction of the hyperphosphataemia should increase the low calcium that occurs when phosphate is high. Successful management of the child with TLS relates to recognition of those at risk, prevention and early recognition of any abnormalities. Most of these children will be diagnosed and treated in the oncology unit, but some may present straight to intensive care for management.
Other Issues Where Children Who Require Specialist Input May Present in ITU
There are many malignancies which may present in an ICU, in particular malignancies that present with a mediastinal mass, such as lymphoma. Often such children require intubation and ventilation and may require procedures such as chest drains. Treatment is a two-way approach: treating the current symptoms and establishing a diagnosis so effective treatment of the malignancy can commence.
Side-Effects of Chemotherapy
Chemotherapy affects the malignant cells but can also damage any rapidly dividing cells in the body. This can lead to significant side-effects which can range from mild to life-threatening. Some of the side-effects that may be seen in the intensive care environment are discussed here. It should be noted that these children can have multiple side-effects and this should be considered when nursing them.
Bone Marrow Suppression
The majority of chemotherapy agents cause some form of bone marrow suppression leading to three main problems seen in the oncology patient: anaemia, thrombocytopenia and neutropenia. These are commonly seen 7–14 days post-chemotherapy.
Anaemia
This is a deficiency of red blood cells or haemoglobin (Hb) leading to a decrease in the oxygen-carrying capacity of the blood (Hastings et al. 2006). It can lead to breathlessness, pallor, headaches, loss of appetite, dizziness, fatigue and irritability. Transfusion is usually performed when the child is symptomatic of anaemia or may be considered when the Hb falls below 7–8 g/dl. However, there is no consensus on the level that the Hb can fall to before transfusion is indicated; this will depend on local practice.
Thrombocytopenia
This is a result of a fall in the circulating platelets resulting in bleeding, purpura or petechiae (Selwood 2008a). Often the management of thrombocytopenia is conservative, although this will vary with local practice. Platelets are usually transfused when a patient is symptomatic or about to undergo an invasive procedure although they may be given if the platelet count is less than 10 × 109 l. Pre-procedure (e.g. a lumbar puncture), platelets may be transfused to ensure there are enough platelets circulating. If a child has a fever, infection or enlarged liver, their effectiveness may be decreased and more platelet transfusions may be required (British Committee for Standards in Haematology 2003).
There is a risk with administering blood products, including adverse reactions and the potential for infection, and these will need to be considered as with any patients. Cytomegalovirus (CMV) carries a significant risk of morbidity and mortality in the immunocompromised patient. This has been reduced since the induction of leukodepleted blood products although most oncology patients will still receive CMV-negative blood products. Irradiated blood products are required for patients immediately pre- and post-stem cell transplantation, patients with Hodgkin’s disease and patients who have received treatment with a purine analogue (e.g. fludarabine). Irradiation destroys the ability of transfused lymphocytes to respond to host foreign antigens thereby preventing graft versus host disease in these patients (BCSH Blood Transfusion Task Force 1996).
Neutropenia
The definition of neutropenia differs between hospitals but is commonly referred to as an absolute neutrophil count of <0.5 × 109 l (normal 2.5–7.5 × 109 l). This is a common complication of cytotoxic chemotherapy and can occur 7–10 days post-treatment and usually recovers by 21 days. There is a significant risk of morbidity and mortality associated with the risk of life-threatening infections and it also leads to delays in chemotherapy. Children should attend for assessment if they have a temperature of 38.5°C or two recordings of 38°C 1 hour apart as temperatures are often the only symptom that there is an infective process taking place. All other inflammatory processes are altered in the immunocompromised child and may not show any signs of infection. On arrival the child should be treated as an oncological emergency and should commence broad spectrum antibiotics within 30–60 minutes once a full assessment has taken place otherwise there is an increased risk of mortality or morbidity (Pizzo 1999).
Immunocompromised children are at risk from both gram-negative and gram-positive sepsis. Gram-negative sepsis (Escherichia coli, Pseudomonas aeruginosa and Klebsiella) used to be the most common organisms seen. Now gram-positive sepsis is more common, mainly caused by the endogenous flora of the patient (e.g. coagulase-negative staphylococci and streptococci) (Oren et al. 2001).
There is a risk of fungal infections in the immunocompromised child and this can also be life-threatening. Children with prolonged neutropenia are at greater risk of invasive fungal infections (Lehrnbecher et al. 1999) and breaches of mucosa which coexist with neutropenia allow a portal for infection into the body. Prolonged use of antibiotics and steroids is an additional risk factor. Antifungal treatment is often given to children who are recognised to be at risk at prophylactic doses. These are then increased to treatment dose as the child presents with an infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


