Chapter 16 Care of Preoperative Patients
Safe and Effective Care Environment
1. Differentiate among the various types and purposes of surgery.
2. Examine individual patient factors for potential threats to safety, especially for older adults.
3. Use appropriate patient identifiers when providing instruction, administering drugs, marking surgical sites, and performing any procedure.
4. Verify that the patient has given informed consent for the surgical procedure and that the presurgical checklist is complete and accurate.
5. Identify patient conditions or issues that need to be communicated to other members of the surgical and postoperative teams.
6. Use effective communication when teaching patients and family members about what to expect during the surgical experience.
7. Act as a patient advocate with regard to patients’ rights, informed consent, and advance directives.
8. Identify learning needs for the patient preparing for surgery.
9. Use knowledge of physiology and behavioral principles to describe an accurate and complete preoperative assessment.
10. Evaluate personal factors that increase the patient’s risk for complications during and immediately after surgery.
11. Evaluate laboratory values for changes that may affect the patient’s response to drugs, anesthesia, and surgery.
12. Explain the purposes and techniques commonly used for patient preoperative preparation.
13. Apply antiembolic stockings, sequential compression boots, or other devices to reduce or prevent vascular complications.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
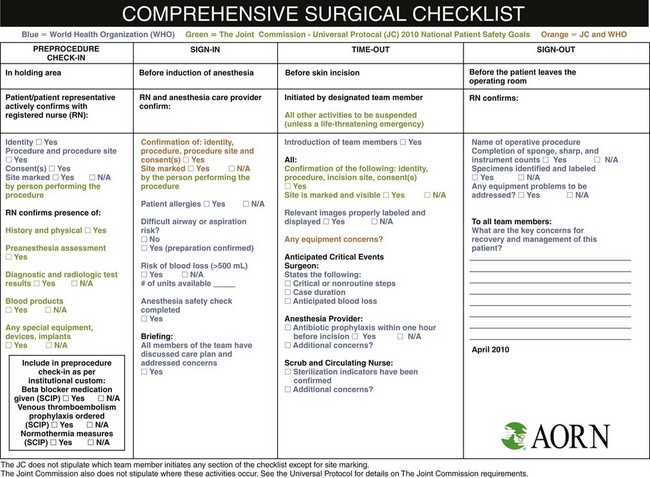
Patient safety throughout the perioperative period is the number-one priority for all personnel. Fig. 16-1 shows an overview of the preoperative activities for patient safety recommended by the World Health Organization (WHO), The Joint Commission (TJC), and the Association of periOperative Registered Nurses (AORN).
Because surgery is invasive and involves exposure to various anesthetic agents and drugs, as well as positioning and other environmental hazards, complications are common. Some complications are predictable and are considered preventable. As a result, TJC has partnered with other groups and agencies and developed a plan for the reduction and eventual elimination of preventable surgical complications known as the Surgical Care Improvement Project (SCIP). Implementation of these core measures is now mandatory for patient safety. The current plan focuses on prevention of infection, prevention of serious cardiac events, and prevention of venous thromboembolism (VTE). Ten specific core measures have been identified as actions required for prevention of these complications in patients identified to be at risk. Table 16-1 provides an overview of these core measure areas. (The numbers associated with the core measures are not always chronological, indicating that some areas are still in development.) The preoperative areas of responsibility for these core measures and their prevention strategies are highlighted in the appropriate areas of this chapter. In addition, some core measures are discussed in patient care chapters most associated with the complication.
TABLE 16-1 SURGICAL CARE IMPROVEMENT PROJECT CORE MEASURE OVERVIEW
| CORE MEASURE IDENTIFICATION | MEASUREMENT NAME/DESCRIPTION |
|---|---|
| SCIP Infection-1 (SCIP Inf-1) | Prophylactic Antibiotic Received Within One Hour Prior to Surgical Incision |
| The purpose is to use short-duration antibiotics to establish bactericidal blood and tissue levels by the time the surgical incision is made. | |
| SCIP Infection-2 (SCIP Inf-2) | Prophylactic Antibiotic Selection for Surgical Patients |
| The purpose is to ensure that prophylactic antibiotics are used for patients who are at increased risk for surgical site infections. The guidelines for risk and for the exact antibiotic to be used are specific to each type of surgical procedure and follow evidence-based published recommendations. | |
| SCIP Infection-3 (SCIP Inf-3) | Prophylactic Antibiotics Discontinued Within 24 Hours After Surgery End Time |
| The purpose is to ensure that prophylactic antibiotic therapy provides benefit without risk. Prolonged prophylactic antibiotic therapy has not been shown to increase benefit and is known to increase the risk for C. difficile infection and the development of microorganisms that are resistant to antimicrobial drugs. | |
| SCIP Infection-4 (SCIP Inf-4) | Cardiac Surgery Patients with Controlled 6 AM Postoperative Blood Glucose (Applies to cardiac surgery patients only) |
| The purpose is to avoid hyperglycemia (which is defined as blood glucose levels above 200 mg/dL and is associated with increased complications and mortality) in cardiac surgery patients, especially patients undergoing coronary artery bypass graft surgery and patients with diabetes who are having cardiac surgery. | |
| SCIP Infection-6 (SCIP Inf-6) | Surgery Patients with Appropriate Hair Removal |
| The purpose is to avoid hair removal procedures, specifically shaving, that cause skin abrasions and increase the risk for surgical site infections. If hair must be removed from the surgical site, removal is performed with electric clippers or chemical depilatories. | |
| SCIP Infection-9 (SCIP Inf-9) | Urinary Catheter Removed on Postoperative Day 1 (POD 1) or Postoperative Day 2 (POD 2) with Day of Surgery Being Day Zero |
| The purpose is to avoid urinary catheter–associated urinary tract infections, which increase with longer duration indwelling catheters. It is unacceptable to have an indwelling urinary catheter in place longer than 48 hours after surgery unless there is a documented specific and medically validated reason for it. | |
| SCIP Infection-10 (SCIP Inf-10) | Surgery Patients with Perioperative Temperature Management |
| The purpose is to prevent prolonged hypothermia, which is associated with impaired wound healing, serious cardiac complications, altered drug metabolism, coagulation problems, and a higher incidence of surgical site infections. Temperature must be measured within 15 minutes from the end of anesthesia administration. Intentional hypothermia must be documented. | |
| SCIP CARD-2 | Surgery Patients on Beta-Blocker Therapy Prior to Arrival Who Received a Beta-Blocker During the Perioperative Period |
| The purpose is to ensure that patients with specific medical conditions receive beta-blocker therapy before surgery and continue the therapy in the immediate postoperative period. This evidence-based action has resulted in a significant reduction in coronary events, cardiovascular mortality, and overall mortality. | |
| SCIP Venous thromboembolism-1 (SCIP VTE-1) | Surgery Patients with Recommended Venous Thromboembolism Prophylaxis Ordered |
| The purpose is to reduce the complications from postoperative venous thromboembolism (VTE). Surgery is a major risk factor responsible for VTE formation and subsequent pulmonary embolism. Although VTE prophylaxis is effective, it is underused. Specific preoperative and postoperative VTE prophylaxis strategies are recommended on the basis of patient risk, type and duration of surgery, and extent of expected postoperative immobilization. | |
| SCIP Venous thromboembolism-2 (SCIP VTE-2) | Surgery Patients Who Received Appropriate Venous Thromboembolism Prophylaxis Within 24 Hours Prior to Surgery to 24 Hours After Surgery |
| The purpose is to reduce the complications from postoperative venous thromboembolism (VTE), particularly among patients undergoing the types of surgeries in which the risk is highest. |
Information compiled from The Joint Commission. (2010). National Patient Safety Goals. Retrieved October 2010 from http://www.jointcommission.org/patientsafety/nationalpatientsafetygoals/.
Overview
The preoperative period begins when the patient is scheduled for surgery and ends at the time of transfer to the surgical suite. As a nurse, you will function as an educator, an advocate, and a promoter of health. The surgical environment demands the use of knowledge, judgment, and skills based on the principles of nursing science. Perioperative nursing places special emphasis on safety, advocacy, and patient education, although ensuring a “culture of safety” is the responsibility of all health care team members (Scherer & Fitzpatrick, 2008).
Categories and Purposes of Surgery
Surgical procedures are categorized by the purpose, body location, extent, and degree of urgency. Table 16-2 explains the categories and gives examples of surgical procedures.
TABLE 16-2 SELECTED CATEGORIES OF SURGICAL PROCEDURES
| CATEGORY | DESCRIPTION | CONDITION OR SURGICAL PROCEDURE |
|---|---|---|
| Reasons for Surgery | ||
| Diagnostic | Performed to determine the origin and cause of a disorder or the cell type for cancer | |
| Curative | Performed to resolve a health problem by repairing or removing the cause | |
| Restorative | Performed to improve a patient’s functional ability | |
| Palliative | Performed to relieve symptoms of a disease process, but does not cure | |
| Cosmetic | Performed primarily to alter or enhance personal appearance | |
| Urgency of Surgery | ||
| Elective | Planned for correction of a nonacute problem | |
| Urgent | Requires prompt intervention; may be life threatening if treatment is delayed more than 24 to 48 hr | |
| Emergent | Requires immediate intervention because of life-threatening consequences | |
| Degree of Risk of Surgery | ||
| Minor | Procedure without significant risk; often done with local anesthesia | |
| Major | Procedure of greater risk; usually longer and more extensive than a minor procedure | |
| Extent of Surgery | ||
| Simple | Only the most overtly affected areas involved in the surgery | |
| Radical | Extensive surgery beyond the area obviously involved; is directed at finding a root cause | |
| Minimally invasive surgery (MIS) | Surgery performed in a body cavity or body area through one or more endoscopes; can correct problems, remove organs, take tissue for biopsy, re-route blood vessels and drainage systems; is a fast-growing and ever-changing type of surgery | |
Surgical Settings
The term inpatient refers to a patient who is admitted to a hospital. The patient may be admitted the day before or, more often, the day of surgery (often termed same-day admission [SDA]), or the patient may already be an inpatient when surgery is needed. The terms outpatient and ambulatory refer to a patient who goes to the surgical area the day of the surgery and returns home on the same day (i.e., same-day surgery [SDS]). Hospital-based ambulatory surgical centers, freestanding surgical centers, physicians’ offices, and ambulatory care centers are common. More than half of all surgical procedures in North America are performed in ambulatory centers (CDC, 2008).
Patient-Centered Collaborative Care
Assessment
History
• Use of tobacco, alcohol, or illicit substances, including marijuana
• Use of complementary or alternative practices, such as herbal therapies, folk remedies, or acupuncture
• Prior surgical procedures and how these were tolerated
• Prior experience with anesthesia, pain control, and management of nausea or vomiting
• Autologous or directed blood donations
• Allergies, including sensitivity to latex products
• Knowledge about and understanding of events during the perioperative period
When taking a history, screen the patient for problems that increase the risk for complications during and after surgery. Some problems that increase the surgical risk or increase the risk for complications after surgery are listed in Table 16-3.
TABLE 16-3 SELECTED FACTORS THAT INCREASE SURGICAL RISK OR INCREASE THE RISK FOR POSTOPERATIVE COMPLICATIONS
| Age |
| Medications |
| Medical History |
| Prior Surgical Experiences |
| Health History |
| Family History |
| Type of Surgical Procedure Planned |
Older patients are at increased risk for complications (Doerflinger, 2009). The normal aging process decreases immune system functioning and delays wound healing. The frequency of chronic illness increases in older patients. In addition, reductions of muscle mass and body water increase the risk for dehydration. See Chart 16-1 for other changes in older adults that may alter the operative response or risk.
Chart 16-1 Nursing Focus on the Older Adult
Changes of Aging as Surgical Risk Factors
| PHYSIOLOGIC CHANGE | NURSING INTERVENTIONS | RATIONALES |
|---|---|---|
| Cardiovascular System | ||
| Decreased cardiac output | Determine normal activity levels, and note when the patient tires. | Knowing limits helps prevent fatigue. |
| Increased blood pressure | ||
| Decreased peripheral circulation | Monitor vital signs, peripheral pulses, and capillary refill. | Having baseline data helps detect deviations. |
| Respiratory System | ||
| Reduced vital capacity | Teach coughing and deep-breathing exercises. | Pulmonary exercises help prevent pulmonary complications. |
| Loss of lung elasticity | ||
| Decreased oxygenation of blood | Monitor respirations and breathing effort. | Having baseline data helps detect deviations. |
| Renal/Urinary System | ||
| Decreased blood flow to kidneys Reduced ability to excrete waste Decline in glomerular filtration rate Nocturia common | Monitor intake and output. Assess overall hydration. Monitor electrolyte status. | Ongoing assessment helps detect fluid and electrolyte imbalances and decreased renal function. |
| Assist frequently with toileting needs, especially at night. | Frequent toileting helps prevent incontinence and falls. | |
| Neurologic System | ||
| Sensory deficits Slower reaction time Decreased ability to adjust to changes in the surroundings | Orient the patient to the surroundings. Allow extra time for teaching the patient. Provide for the patient’s safety. | An individualized preoperative teaching plan is developed based on the patient’s orientation and any neurologic deficits. |
| Safety measures help prevent falls and injury. | ||
| Musculoskeletal System | ||
| Increased incidence of deformities related to osteoporosis or arthritis | Assess the patient’s mobility. Teach turning and positioning. Encourage ambulation. | Interventions help prevent complications of immobility. |
| Place on falls precautions, if indicated. | Safety measures help prevent injury. | |
| Skin | ||
| Dry with less subcutaneous fat makes the skin at greater risk for damage; slower skin healing increases risk for infection | Assess the patient’s skin before surgery for lesions, bruises, and areas of decreased circulation. | Having baseline data helps detect changes and evaluate interventions. |
| Pad bony prominences. | Padding can protect at-risk areas. | |
| Use pressure-avoiding or pressure-reducing overlays. | Overlays can prevent pressure ulcer formation by redistributing body weight. | |
| Avoid applying tape to skin. | Tape removal damages thin skin. | |
| Teach the patient to change position at least every 2 hours. | Changing position frequently helps prevent reduced blood flow to an area and changes external pressure patterns. | |
Drugs and substance use may affect patient responses to surgery. The use of tobacco increases the risk for pulmonary complications because of changes it causes to the lungs and chest cavity. Excessive alcohol and illicit substance use can alter the patient’s responses to anesthesia and pain medication. Withdrawal of alcohol before surgery may lead to delirium tremens. Prescription and over-the-counter drugs may also affect how the patient reacts to the operative experience. Adverse effects can occur with the use of some herbs, such as those listed in Table 16-4.
TABLE 16-4 POTENTIAL EFFECTS OF HERBS
| HERB | POTENTIAL EFFECT |
|---|---|
| Black cohosh | Bradycardia, hypotension, joint pains |
| Bloodroot | Bradycardia, dysrhythmia, dizziness, impaired vision, intense thirst |
| Boneset | Liver toxicity, mental changes, respiratory problems |
| Coltsfoot | Fever, liver toxicity |
| Dandelion | Interactions with diuretics, increased concentration of lithium or potassium |
| Ephedra | Headache, dizziness, insomnia, tachycardia, hypertension, anxiety, irritability, dry mouth |
| Feverfew | Interference with blood-clotting mechanisms |
| Garlic | Hypotension, blood-clotting inhibition, potentiation of diabetes drugs |
| Ginseng | Headache, anxiety, insomnia, hypertension, tachycardia, asthma attacks, postmenopausal bleeding |
| Goldenseal | Vasoconstriction |
| Hawthorn | Hypotension |
| Kava | Damage to the eyes, skin, liver, and spinal cord from long-term use |
| Licorice | Hyperkalemia, hypernatremia |
| Lobelia | Hearing and vision problems |
| Motherwort | Increased anticoagulation |
| Nettle | Hypokalemia |
| Senna | Potentiation of digoxin |
| St. John’s wort | Antidepressant, photosensitivity |
| Valerian root | Mild sedative or tranquilizer effect, hepatotoxicity |
Medical history is important to obtain because many chronic illnesses increase surgical risks and need to be considered when planning care (Woolger, 2008). For example, a patient with systemic lupus erythematosus may need additional drugs to offset the stress of the surgery. A patient with diabetes may need a more extensive bowel preparation because of decreased intestinal motility. An infection may need to be treated before surgery.
Ask the patient specifically about cardiac disease because complications from anesthesia occur more often in patients with cardiac problems (Morse, 2009; Johnson, 2011). A patient with a history of rheumatic heart disease may be prescribed antibiotics before surgery. Cardiac problems that increase surgical risks include coronary artery disease, angina, myocardial infarction (MI) within 6 months before surgery, heart failure, hypertension, and dysrhythmias. These problems impair the patient’s ability to withstand hemodynamic changes and alter the response to anesthesia. The risk for an MI during surgery is higher in patients who have heart problems. Patients with cardiac disease may require perioperative therapy with beta-blocking drugs, as recommended by core measures for SCIP CARD-2 (see Table 16-1).
Pulmonary complications during or after surgery are more likely to occur in older patients, those with chronic respiratory problems, and smokers because of smoking- or age-related lung changes (Doerflinger, 2009). Increased chest rigidity and loss of lung elasticity reduce anesthetic excretion. Smoking increases the blood level of carboxyhemoglobin (carbon monoxide on oxygen-binding sites of the hemoglobin molecule), which decreases oxygen delivery to organs. Action of cilia in pulmonary mucous membranes decreases, which leads to retained secretions and predisposes the patient to infection (pneumonia) and atelectasis (collapse of alveoli). Atelectasis reduces gas exchange and causes intolerance of anesthesia. It is also a common problem after general anesthesia.
Previous surgical procedures and anesthesia affect the patient’s readiness for surgery. Previous experiences, especially with complications, may increase anxiety about the scheduled surgery. Ask about the patient’s experience with anesthesia and all allergies. These data provide information about tolerance of and possible fears about the use of anesthesia. The family medical history and problems with anesthetics may indicate possible reactions to anesthesia, such as malignant hyperthermia (see Chapter 17).
Discharge planning is started before surgery. Assess the patient’s home environment, self-care capabilities, and support systems and anticipate postoperative needs before surgery. All patients, regardless of how minor the procedure or how often they have had surgery, should have discharge planning. Older patients and dependent adults may need transportation referrals to and from the physician’s office or the surgical setting. A home care nurse may be needed to monitor recovery and to provide instructions. All patients with few support systems may need follow-up care at home. Some patients need a planned direct admission to a rehabilitation hospital or center for physical therapy after surgery, especially joint replacement surgery (Lucas, 2008). Shortened hospital stays require adequate discharge planning to achieve the desired outcomes after surgery.
Physiological Integrity
A. Check the client’s international normalized ratio (INR).
B. Call the laboratory to ensure that the blood is physically at the operating facility.
C. Ensure that the client has given consent to receive blood if a transfusion is necessary.
D. Inform the client that an autologous transfusion does not eliminate the risk for development of bloodborne diseases.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree