M. Linda Workman
Care of Patients with Shock
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
10 Compare the risk factors, causes, and manifestations of different types of shock.
11 Identify the manifestations associated with shock progression.
12 Use laboratory data and clinical manifestations to determine the effectiveness of therapy for shock.
13 Describe the actions, side effects, and nursing implications of drug therapy for shock.
14 Coordinate the nursing care for the patient experiencing any stage of hypovolemic shock.
16 Prioritize the nursing care for the patient with sepsis or septic shock.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
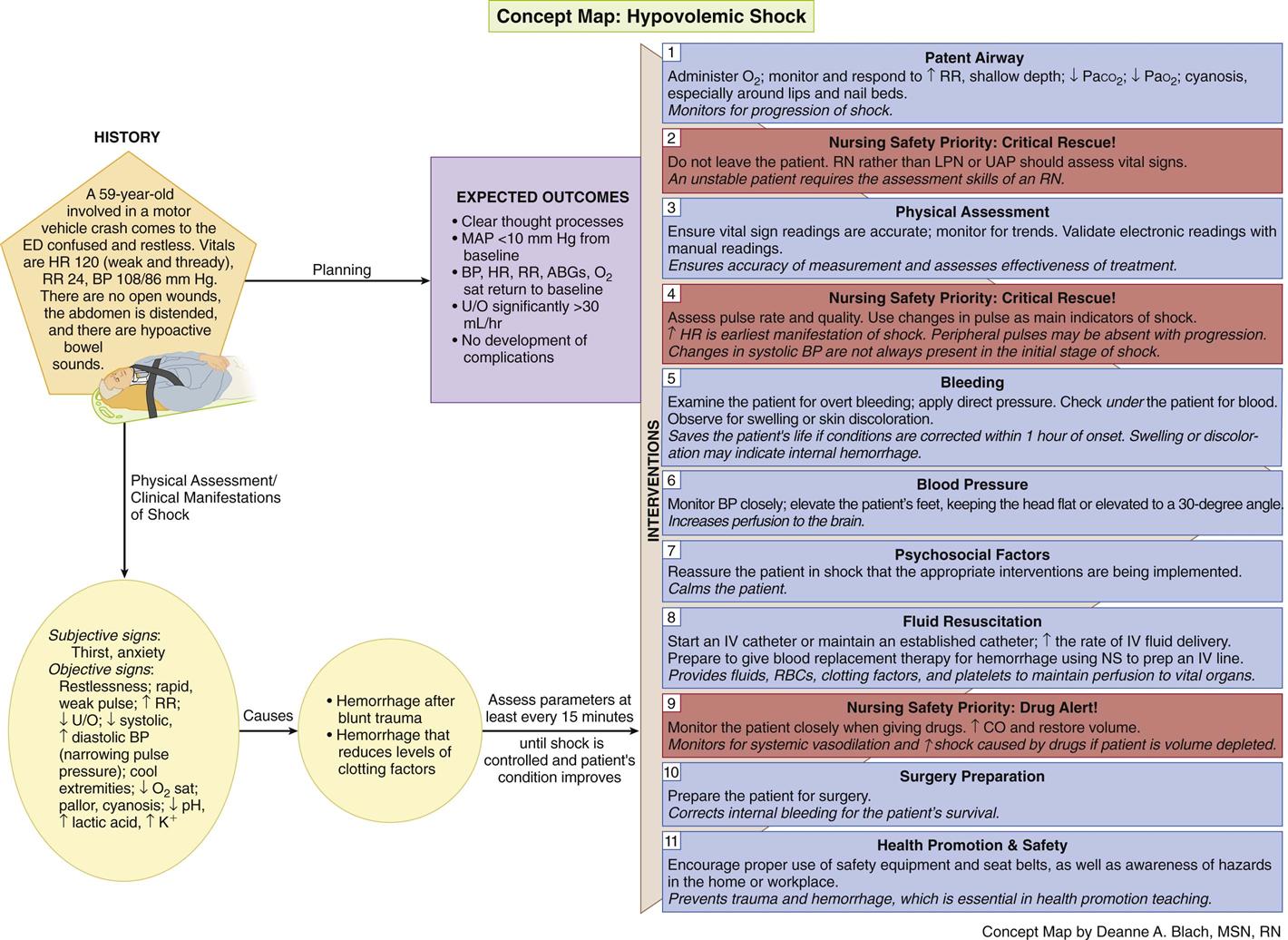
Concept Map: Hypovolemic Shock
Key Points
Review Questions for the NCLEX® Examination
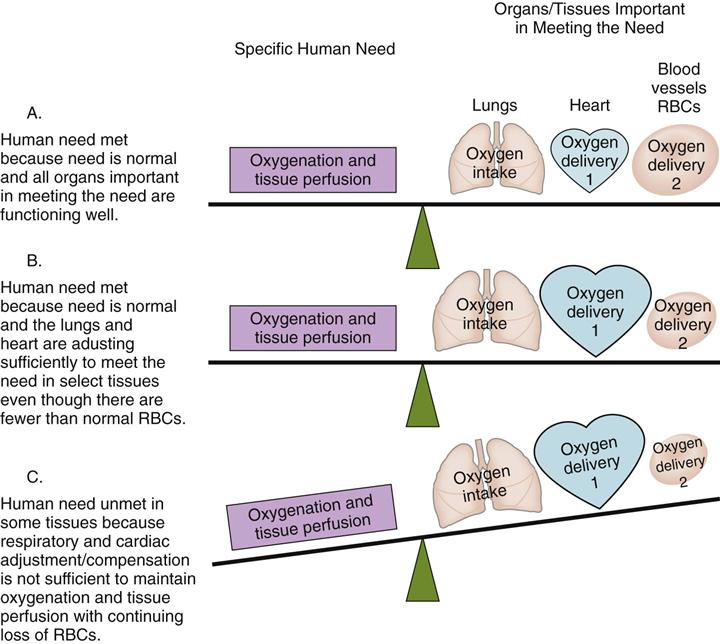
Overview
A continuous supply of oxygen is needed by all organs, tissues, and cells to function properly. The lungs first bring oxygen into the body, and the cardiovascular system (heart, blood, and blood vessels) delivers oxygen to all tissues and removes cellular wastes (Fig. 39-1). Shock is widespread abnormal cellular metabolism that occurs when oxygenation and tissue perfusion needs are not met to the level necessary to maintain cell function (McCance et al., 2010). It is a condition rather than a disease and represents the “whole-body” response that occurs when too little oxygen is delivered to the tissues. All body organs are affected by shock and either work harder to adapt and compensate for reduced oxygenation (see Fig. 39-1) or fail to function because of hypoxia. Shock is a “syndrome” because the cellular, tissue, and organ events occur in a predictable sequence.
Any problem that impairs oxygen delivery to tissues and organs can start the syndrome of shock and lead to a life-threatening emergency. Most often, shock is a result of cardiovascular problems and changes. Patients in acute care settings are at higher risk, but shock can occur in any setting. For example, older patients in long-term care settings are at risk for sepsis and shock related to urinary tract infections. When the body’s adaptive adjustments (compensation) or health care interventions are not effective and shock progresses, severe hypoxia can lead to cell loss, multiple organ dysfunction syndrome (MODS), and death.
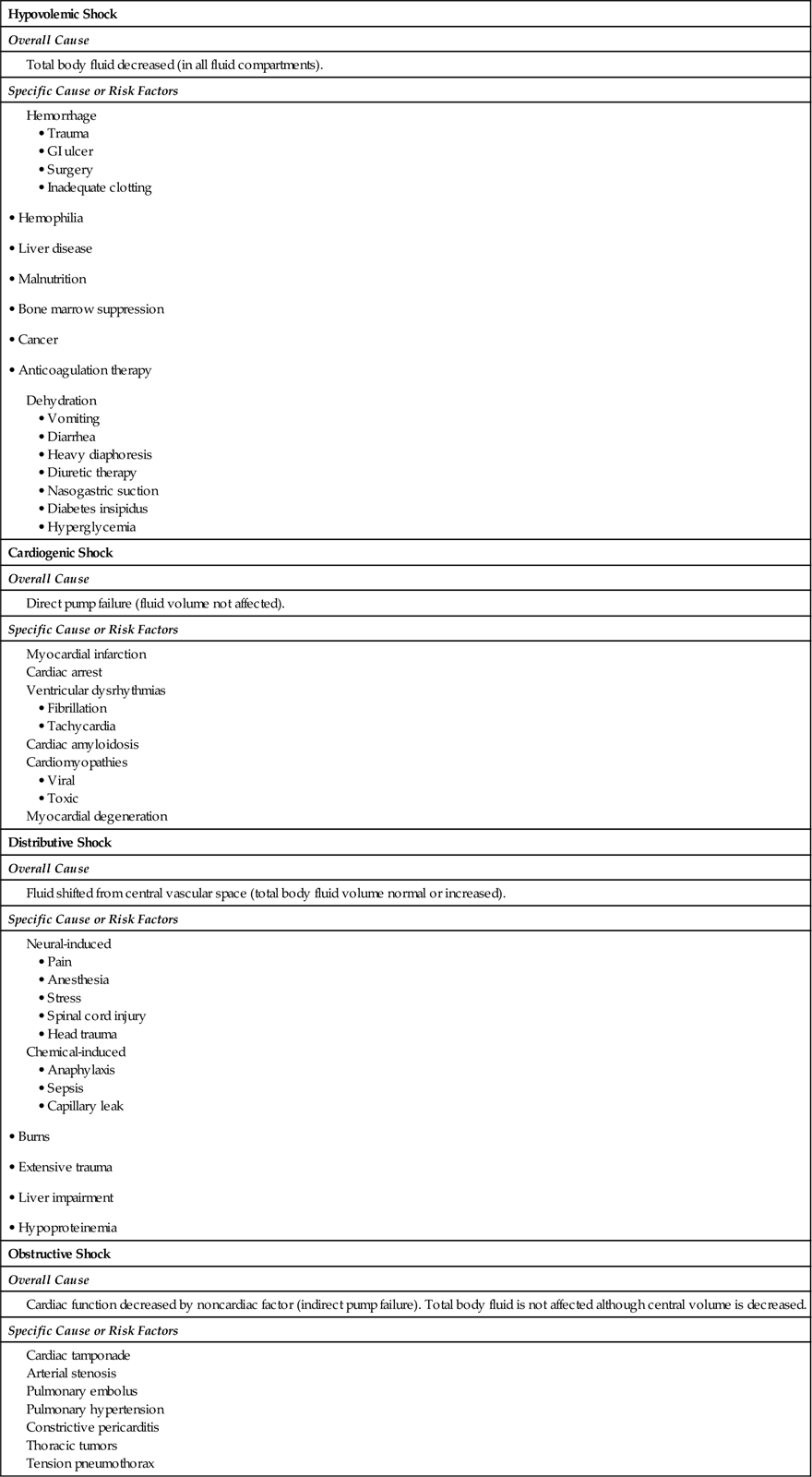
Shock is classified by the functional impairment it causes into the categories of hypovolemic shock, cardiogenic shock, distributive shock (which includes septic shock, neurogenic shock, and anaphylactic shock), and obstructive shock. Table 39-1 describes the functional impairment classification and common causes of shock.
TABLE 39-1
CAUSES AND TYPES OF SHOCK BY FUNCTIONAL IMPAIRMENT
Most manifestations of shock are similar regardless of what starts the process or which tissues are affected first. These common manifestations result from physiologic adjustments (compensatory mechanisms) in the attempt to ensure continued oxygenation of vital organs. These adjustment actions are performed by the sympathetic nervous system, triggering the stress response and activating the endocrine and cardiovascular systems. Manifestations unique to any one type of shock result from specific tissue dysfunction. The common features of shock are listed in Chart 39-1.
Review of Oxygenation and Tissue Perfusion
Oxygenation and perfusion depend on how much oxygen from arterial blood perfuses the tissue. Tissue and organ perfusion is related to mean arterial pressure (MAP). Because the cardiovascular system is a closed but continuous circuit, the factors that influence MAP include:
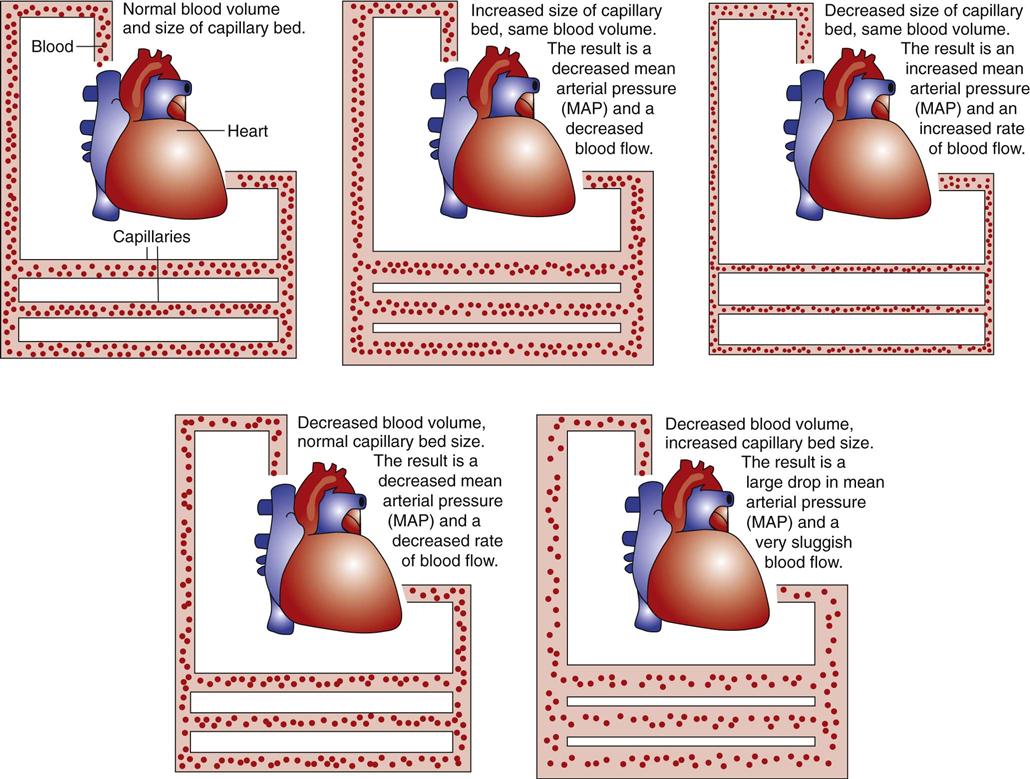
Total blood volume and cardiac output are directly related to MAP, so increases in either total blood volume or cardiac output raise MAP. Decreases in either total blood volume or cardiac output lower MAP.
The size of the vascular bed is inversely (negatively) related to MAP. This means that increases in the size of the vascular bed lower MAP and decreases raise MAP (Fig. 39-2). The small arteries and veins connected to capillaries can increase in diameter by relaxing the smooth muscle in vessel walls (dilation) or decrease in diameter by contracting the muscle (vasoconstriction). When blood vessels dilate and total blood volume remains the same, blood pressure decreases and blood flow is slower. When blood vessels constrict and total blood volume remains the same, blood pressure increases and blood flow is faster.
Blood vessels are innervated by the sympathetic division of the autonomic nervous system. Some nerves continuously stimulate vascular smooth muscle so that the blood vessels are normally partially constricted, a condition called sympathetic tone. Increases in sympathetic stimulation constrict smooth muscle even more, raising MAP. Decreases in sympathetic tone relax smooth muscle, dilating blood vessels and lowering MAP.
Blood flow to organs varies and adjusts to changes in tissue oxygen needs. The body can selectively increase blood flow to some areas while reducing blood flow to others. The skin and skeletal muscles can tolerate low levels of oxygen for hours without dying or being damaged. Other organs (e.g., heart, brain, liver, pancreas) do not tolerate hypoxic (low levels of tissue oxygenation), and only a few minutes without oxygen results in serious damage and cell death.
Types of Shock
Types of shock and their causes vary because shock is a manifestation of a pathologic condition rather than a disease state (see Table 39-1). More than one type of shock can be present at the same time. For example, trauma caused by a car crash may trigger hemorrhage (leading to hypovolemic shock) and a myocardial infarction (leading to cardiogenic shock).
Hypovolemic shock occurs when too little circulating blood volume causes a MAP decrease, resulting in inadequate total body oxygenation. Common problems leading to hypovolemic shock are hemorrhage and dehydration. A complete discussion of the pathophysiology and management of hypovolemic shock begins on p. 812.
Cardiogenic shock occurs when the actual heart muscle is unhealthy and pumping is directly impaired. Myocardial infarction is the most common cause of direct pump failure (Held & Sturtz, 2009). Other causes are listed in Table 39-1. Any type of pump failure decreases cardiac output and MAP. Chapter 40 discusses the pathophysiology and care for the person with cardiogenic shock from myocardial infarction.
Distributive shock occurs when blood volume is not lost from the body but is distributed to the interstitial tissues where it cannot circulate and deliver oxygen. It can be caused by a loss of sympathetic tone, blood vessel dilation, pooling of blood in venous and capillary beds, and increased capillary leak. All these factors can decrease mean arterial pressure (MAP) and may be started by nerve changes (neural-induced) or the presence of some chemicals (chemical-induced).
Neural-induced distributive shock is a loss of MAP that occurs when sympathetic nerve impulses controlling blood vessel smooth muscle are decreased and the smooth muscles relax, causing vasodilation. This blood vessel dilation can be a normal local response to injury, but shock results when vasodilation is widespread (King & Olson, 2007). Problems leading to loss of sympathetic tone are listed in Table 39-1.
Chemical-induced distributive shock has three common origins: anaphylaxis, sepsis, and capillary leak syndrome. It occurs when certain body chemicals or foreign substances in the blood and vessels start widespread changes in blood vessel walls. The chemicals are usually exogenous (originate outside the body), but this type of shock also can be induced by substances normally found in the body (endogenous), such as excessive amounts of the mediator histamine.
Anaphylaxis is one result of type I allergic reactions. It begins within seconds to minutes after exposure to a specific allergen in a susceptible person. The result is widespread loss of blood vessel tone and decreased cardiac output. Table 22-2 (in Chapter 22) lists common allergens that can cause anaphylaxis. Chapter 22 describes the pathophysiology, prevention, and care of the patient with anaphylactic shock.
Sepsis is a widespread infection that triggers a whole-body inflammatory response. It leads to distributive shock when infectious microorganisms are present in the blood. This form of shock is most commonly called septic shock. A complete discussion of the pathophysiology, prevention, and collaborative care for the patient with sepsis and septic shock begins on p. 819.
Capillary leak syndrome is the response of capillaries to the presence of biologic mediators that change blood vessel integrity and allow fluid to shift from the blood vessels into the interstitial tissues. Once in the interstitial tissue, these fluids are stagnant and cannot deliver oxygen or remove tissue waste products. Fluid shifts result from increased size of capillary pores, loss of plasma osmolarity, and increased hydrostatic pressure in the blood. Problems causing fluid shifts include severe burns, liver disorders, ascites, peritonitis, paralytic ileus, severe malnutrition, large wounds, hyperglycemia, kidney disease, hypoproteinemia, and trauma.
Obstructive shock is caused by problems that impair the ability of the normal heart muscle to pump effectively. The heart itself remains normal, but conditions outside the heart prevent either adequate filling of the heart or adequate contraction of the healthy heart muscle. The most common causes of obstructive shock are pericarditis and cardiac tamponade (see Table 39-1). Care of the person with cardiac tamponade is presented in detail in Chapter 37 (pericarditis) and Chapter 40 (as a complication after cardiac bypass graft surgery).
Although the causes and initial manifestations associated with the different types of shock vary, eventually the effects of hypotension and anaerobic cellular metabolism (metabolism without oxygen) result in the common key features of shock listed in Chart 39-1. The origin of these features is explained below in the discussion of Pathophysiology in the Hypovolemic Shock section.
Hypovolemic Shock
Pathophysiology
The basic problem of hypovolemic shock is a loss of blood volume from the vascular space, resulting in a decreased mean arterial pressure (MAP) (see Fig. 39-2) and a loss of oxygen-carrying capacity from the loss of circulating red blood cells (RBCs). The reduced MAP slows blood flow, resulting in decreased tissue perfusion. The loss of RBCs decreases the ability of the blood to oxygenate the tissue it does reach. These oxygenation and perfusion problems lead to cellular anaerobic (without oxygen) conditions and abnormal cellular metabolism.
The main trigger leading to hypovolemic shock is a sustained decrease in MAP that results from decreased circulating blood volume. A decrease in MAP of 5 to 10 mm Hg below the patient’s normal baseline value is detected by pressure-sensitive nerve receptors (baroreceptors) in the aortic arch and carotid sinus. This information is transmitted to brain centers, which stimulate adjustments (compensatory mechanisms) that help ensure continued blood flow and oxygen delivery to vital organs while limiting blood flow to less vital areas. The movement of oxygenated blood into selected areas while bypassing others (“shunting”) results in some shock manifestations.
If the events that caused the initial decrease in MAP are halted now, compensatory mechanisms provide adequate oxygenation and perfusion without outside intervention. If the initiating events continue and MAP decreases further, some tissues function under anaerobic conditions. This condition increases lactic acid levels and other harmful metabolites (e.g., protein-destroying enzymes, oxygen free radicals). These substances cause electrolyte and acid-base imbalances with tissue-damaging effects and depressed heart muscle activity. These effects are temporary and reversible if the cause of shock is corrected within 1 to 2 hours after onset. When shock conditions continue for longer periods without help, the resulting acid-base imbalance, electrolyte imbalances, and increased metabolites cause so much cell damage in vital organs that multiple organ dysfunction syndrome (MODS) occurs and recovery from shock is no longer possible. Table 39-2 summarizes the responses during the progression of shock.
TABLE 39-2
ADAPTIVE RESPONSES AND EVENTS DURING HYPOVOLEMIC SHOCK
| Initial Stage |
| Nonprogressive Stage |
| Progressive Stage |
| Refractory Stage |
Stages of Shock
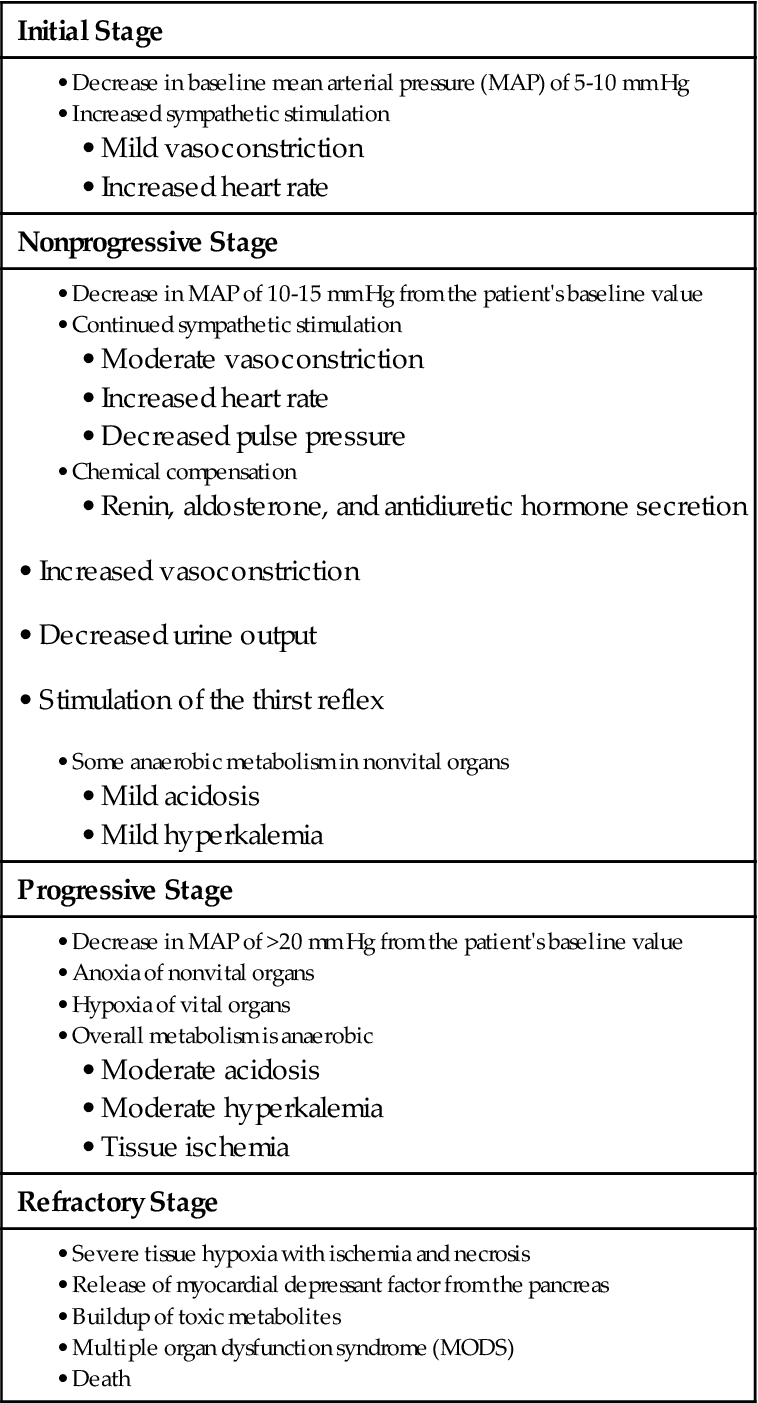
The syndrome of shock progresses in four stages when the conditions that cause shock remain uncorrected and poor cellular oxygenation continues. These stages are:
The stages are defined on the basis of how well compensatory mechanisms are working, the severity of the clinical manifestations, and whether tissue damage is reversible.
Initial Stage of Shock (Early Stage).
The initial (early) stage of shock is present when the patient’s baseline MAP is decreased by less than 10 mm Hg. During this stage, compensatory mechanisms are so effective at returning systolic pressure to normal that oxygenated blood flow to vital organs is maintained. The cellular change in this stage is increased anaerobic metabolism with production of lactic acid, although overall metabolism is still aerobic. The compensation responses of vascular constriction and increased heart rate are effective, and both cardiac output and MAP are maintained within the normal range. Because vital organ function is not disrupted, the manifestations of shock are difficult to detect. A heart and respiratory rate increased from the patient’s baseline level or a slight increase in diastolic blood pressure may be the only objective manifestation of this early stage of shock.
Nonprogressive Stage of Shock (Compensatory Stage).
The nonprogressive (compensatory) stage of shock occurs when MAP decreases by 10 to 15 mm Hg from baseline. Kidney and hormonal compensatory mechanisms are activated because cardiovascular responses alone are not enough to maintain MAP and supply oxygen to vital organs.
The kidneys and baroreceptors sense an ongoing decrease in MAP and trigger the release of renin, antidiuretic hormone (ADH), aldosterone, epinephrine, and norepinephrine to start kidney compensation. Renin, secreted by the kidney, causes decreased urine output, increased sodium reabsorption, and widespread blood vessel constriction (see Fig. 13-6 in Chapter 13). ADH increases water reabsorption in the kidney, further reducing urine output, and also causes blood vessel constriction in the skin and other less vital tissue areas. Together these actions compensate for shock by maintaining the fluid volume within the central blood vessels.
Tissue hypoxia occurs in nonvital organs (e.g., skin, GI tract) and in the kidney, but it is not great enough to cause permanent damage. Because some metabolism is anaerobic, acid-base and electrolyte changes occur in response to the buildup of metabolites. Changes include acidosis (low blood pH) and hyperkalemia (increased blood potassium level).
Manifestations of the nonprogressive stage of shock include both subjective and objective changes resulting from decreased tissue perfusion. Subjective changes include thirst and anxiety. Objective changes include restlessness, tachycardia, increased respiratory rate, decreased urine output, falling systolic blood pressure, rising diastolic blood pressure, narrowing pulse pressure, cool extremities, and a 2% to 5% decrease in oxygen saturation measured by pulse oximetry. Comparing these changes with the values and manifestations obtained earlier is critical to identifying this stage of shock.
If the patient is stable and compensatory mechanisms are supported by medical and nursing interventions, he or she can remain in this stage for hours without having permanent damage. Stopping the conditions that started the shock at this stage and providing supportive interventions can prevent the shock from progressing. The cellular effects of this stage are reversible when nurses recognize the problem and coordinate with the health care team to start appropriate interventions (Mattiace, 2008; Stricker, 2010).
Progressive Stage of Shock (Intermediate Stage).
The progressive stage of shock occurs when there is a sustained decrease in MAP of more than 20 mm Hg from baseline. In this stage, compensatory mechanisms are functioning but can no longer deliver sufficient oxygen, even to vital organs. Vital organs develop hypoxia, and less vital organs become anoxic (no oxygen) and ischemic (cell dysfunction or death from lack of oxygen). As a result of poor oxygenation and a buildup of toxic metabolites, some tissues have severe cell damage and die.
Manifestations of the progressive stage of shock include a worsening of subjective and objective changes resulting from decreased tissue perfusion. Continuous monitoring and comparison with earlier findings are critical to assess therapy effectiveness. Subjective changes include severe thirst sensation and deeper anxiety. The patient may express a sense of “something bad” (impending doom) about to happen. He or she may seem confused. Objective changes are a rapid, weak pulse; low blood pressure; pallor to cyanosis of oral mucosa and nail beds; cool and moist skin; anuria; and a 5% to 20% decrease in oxygen saturation. Laboratory data at this stage may show a low blood pH, along with rising lactic acid and potassium levels.
The progressive stage of shock is a life-threatening emergency. Vital organs can tolerate this situation for only a short time before being damaged permanently. Immediate interventions are needed to reverse the effects of this stage of shock. Tolerance varies from person to person and depends on age and health. The patient’s life usually can be saved if the conditions causing shock are corrected within 1 hour or less of the onset of the progressive stage.
Refractory Stage of Shock (Irreversible Stage).
The refractory stage or irreversible stage of shock occurs when too much cell death and tissue damage result from too little oxygen reaching the tissues. Vital organs have overwhelming damage. The body can no longer respond effectively to interventions, and shock continues. Therapy is not effective in saving the patient’s life, even if the cause of shock is corrected and MAP temporarily returns to normal. So much tissue damage has occurred with widespread release of toxic metabolites and enzymes that cell damage in vital organs continues despite aggressive interventions. Manifestations are a rapid loss of consciousness; nonpalpable pulse; cold, dusky extremities; slow, shallow respirations; and unmeasurable oxygen saturation.
Multiple Organ Dysfunction Syndrome.
The sequence of cell damage caused by the massive release of toxic metabolites and enzymes is termed multiple organ dysfunction syndrome (MODS). Once the damage has started, the sequence becomes a vicious cycle as more dead cells break open and release harmful metabolites. These trigger small clots (microthrombi) to form, which block tissue oxygenation and damage more cells, thus continuing the devastating cycle. Liver, heart, brain, and kidney functions are lost first. The most profound change is damage to the heart muscle. One cause of this damage is the release of myocardial depressant factor (MDF) from the ischemic pancreas.
Etiology
Hypovolemic shock occurs when too little circulating blood volume causes a MAP decrease that prevents total body oxygenation. Common problems leading to hypovolemic shock are hemorrhage (external or internal) and dehydration.
Hypovolemic shock from external hemorrhage is common after trauma and surgery. Hypovolemic shock from internal hemorrhage occurs with blunt trauma, GI ulcers, and poor control of surgical bleeding. Hemorrhage also can be caused by any problem that reduces the levels of clotting factors (see Table 39-1). Hypovolemia as a result of dehydration can be caused by any problem that decreases fluid intake or increases fluid loss (see Table 39-1).
Incidence/Prevalence
The exact incidence of hypovolemic shock is not known because it is a response rather than a disease. It is a common complication among hospitalized patients in emergency departments and after surgery or invasive procedures.
Health Promotion and Maintenance
Hypovolemic shock from most causes can be prevented. Teach all people to prevent dehydration by having an adequate fluid intake during exercise and when in hot, dry environments. Urge people to prevent trauma and hemorrhage by using proper safety equipment and seat belts and being aware of hazards in the home or workplace.
Secondary prevention of hypovolemic shock is a major nursing responsibility. Keep in mind that just being a patient in the acute care setting is a risk factor. Identify patients at risk for dehydration, and assess for early manifestations. This is especially important for those who have reduced cognition or reduced mobility or who are on NPO status.
Assess all patients who have invasive procedures or trauma for obvious or occult bleeding. Compare pulse quality and rate with baseline. Compare urine output with fluid intake. Check vital signs for patients who have persistent thirst. Assess for shock in any patient who develops a change in mental status, an increase in pain, or an increase in anxiety.
When patients have invasive procedures or ambulatory surgery and then go home, teach them and their families the manifestations of shock. Stress the importance of seeking immediate help for obvious heavy bleeding, persistent thirst, decreased urine output, light-headedness, or a sense of impending doom (a feeling that something bad is happening or going to happen).
Patient-Centered Collaborative Care
The Concept Map on p. 815 addresses assessment and nursing care issues related to hypovolemic shock.
Assessment
History
Ask about risk factors related to hypovolemic shock. If the patient is alert and stable, question him or her directly. If the patient is not alert or is not stable, collect information from family members. Age is important because hypovolemic shock from trauma is more common in young adults and other types of shock are more common in older adults. Ask patients about recent illness, trauma, procedures, or chronic health problems that may lead to shock. These problems include GI ulcers, general surgery, hemophilia, liver disorders, and prolonged vomiting and diarrhea. Ask about the use of drugs such as aspirin, other NSAIDs, and diuretics that may cause changes leading to hypovolemic shock.
Ask about fluid intake and output during the previous 24 hours. Information about urine output is especially important because urine output is reduced during the first stages of shock, even when fluid intake is normal.
Assess the patient for obvious signs or factors that can lead to shock. Areas to examine for signs of hemorrhage include the gums, wounds, and sites of dressings, drains, and vascular accesses. Also check under the patient for blood. Observe for any swelling or skin discoloration that may indicate an internal hemorrhage.
Physical Assessment/Clinical Manifestations
Most manifestations of hypovolemic shock are caused by the changes resulting from compensatory efforts. Compensatory mechanisms are physiologic responses that try to keep an adequate blood flow to vital organs. Signs of shock are first evident as changes in cardiovascular function. As shock progresses, changes in the renal, respiratory, integumentary, musculoskeletal, and central nervous systems become evident. Ensure that vital sign measurements are accurate, and monitor them for trends indicating shock.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree