Chapter 39 Care of Patients with Shock
Safe and Effective Care Environment
1. Evaluate patient risk for hypovolemic shock or sepsis and septic shock.
2. Ensure vital sign measurements are accurate, and monitor them for changes indicating the presence of shock.
3. Apply principles of infection control to prevent infection and sepsis in susceptible patients, especially older adults.
Health Promotion and Maintenance
4. Teach all people to avoid dehydration.
5. Teach all people to use safety devices to avoid trauma.
6. Instruct all patients going home after surgery or invasive procedures to seek immediate attention for persistent manifestations of early shock.
7. Teach all patients who have a local infection to seek medical attention when manifestations of systemic infection appear.
8. Assess the vital signs, especially pulse and oxygen saturation, for any patient who has a sudden change in mental status, including increased anxiety, apprehension, or agitation.
9. Reassure the patient in shock that the appropriate interventions are being implemented.
10. Compare the risk factors, causes, and manifestations of different types of shock.
11. Identify the manifestations associated with shock progression.
12. Use laboratory data and clinical manifestations to determine the effectiveness of therapy for shock.
13. Describe the actions, side effects, and nursing implications of drug therapy for shock.
14. Coordinate the nursing care for the patient experiencing any stage of hypovolemic shock.
15. Explain the role of the systemic inflammatory response syndrome (SIRS) in the manifestations and progression of sepsis and septic shock.
16. Prioritize the nursing care for the patient with sepsis or septic shock.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Concept Map: Hypovolemic Shock
Review Questions for the NCLEX® Examination
Overview
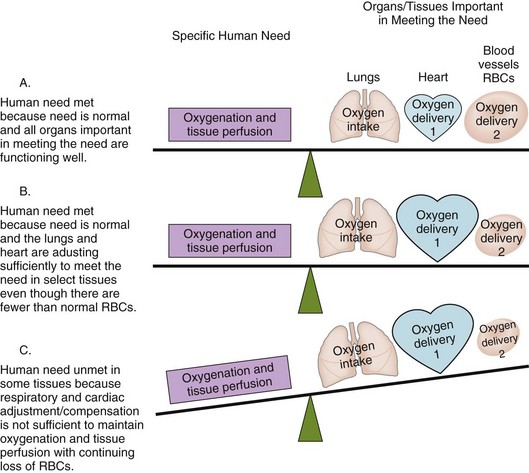
A continuous supply of oxygen is needed by all organs, tissues, and cells to function properly. The lungs first bring oxygen into the body, and the cardiovascular system (heart, blood, and blood vessels) delivers oxygen to all tissues and removes cellular wastes (Fig. 39-1). Shock is widespread abnormal cellular metabolism that occurs when oxygenation and tissue perfusion needs are not met to the level necessary to maintain cell function (McCance et al., 2010). It is a condition rather than a disease and represents the “whole-body” response that occurs when too little oxygen is delivered to the tissues. All body organs are affected by shock and either work harder to adapt and compensate for reduced oxygenation (see Fig. 39-1) or fail to function because of hypoxia. Shock is a “syndrome” because the cellular, tissue, and organ events occur in a predictable sequence.
Shock is classified by the functional impairment it causes into the categories of hypovolemic shock, cardiogenic shock, distributive shock (which includes septic shock, neurogenic shock, and anaphylactic shock), and obstructive shock. Table 39-1 describes the functional impairment classification and common causes of shock.
TABLE 39-1 CAUSES AND TYPES OF SHOCK BY FUNCTIONAL IMPAIRMENT
| Hypovolemic Shock |
| Overall Cause |
| Specific Cause or Risk Factors |
| Cardiogenic Shock |
| Overall Cause |
| Specific Cause or Risk Factors |
| Distributive Shock |
| Overall Cause |
| Specific Cause or Risk Factors |
| Obstructive Shock |
| Overall Cause |
| Specific Cause or Risk Factors |
Most manifestations of shock are similar regardless of what starts the process or which tissues are affected first. These common manifestations result from physiologic adjustments (compensatory mechanisms) in the attempt to ensure continued oxygenation of vital organs. These adjustment actions are performed by the sympathetic nervous system, triggering the stress response and activating the endocrine and cardiovascular systems. Manifestations unique to any one type of shock result from specific tissue dysfunction. The common features of shock are listed in Chart 39-1.
Shock
Review of Oxygenation and Tissue Perfusion
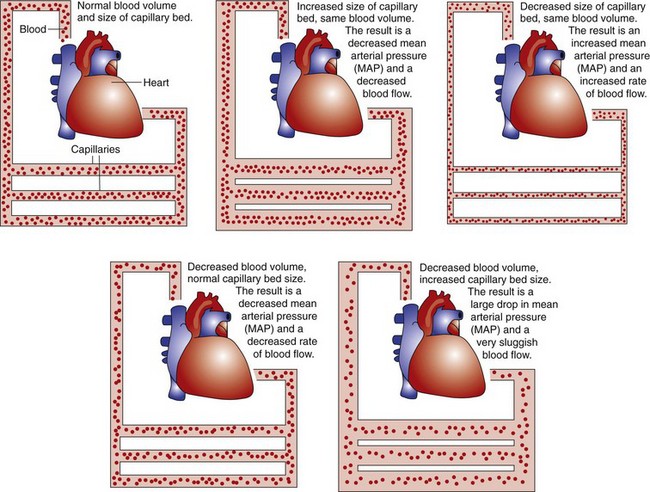
The size of the vascular bed is inversely (negatively) related to MAP. This means that increases in the size of the vascular bed lower MAP and decreases raise MAP (Fig. 39-2). The small arteries and veins connected to capillaries can increase in diameter by relaxing the smooth muscle in vessel walls (dilation) or decrease in diameter by contracting the muscle (vasoconstriction). When blood vessels dilate and total blood volume remains the same, blood pressure decreases and blood flow is slower. When blood vessels constrict and total blood volume remains the same, blood pressure increases and blood flow is faster.
Types of Shock
Types of shock and their causes vary because shock is a manifestation of a pathologic condition rather than a disease state (see Table 39-1). More than one type of shock can be present at the same time. For example, trauma caused by a car crash may trigger hemorrhage (leading to hypovolemic shock) and a myocardial infarction (leading to cardiogenic shock).
Cardiogenic shock occurs when the actual heart muscle is unhealthy and pumping is directly impaired. Myocardial infarction is the most common cause of direct pump failure (Held & Sturtz, 2009). Other causes are listed in Table 39-1. Any type of pump failure decreases cardiac output and MAP. Chapter 40 discusses the pathophysiology and care for the person with cardiogenic shock from myocardial infarction.
Neural-induced distributive shock is a loss of MAP that occurs when sympathetic nerve impulses controlling blood vessel smooth muscle are decreased and the smooth muscles relax, causing vasodilation. This blood vessel dilation can be a normal local response to injury, but shock results when vasodilation is widespread (King & Olson, 2007). Problems leading to loss of sympathetic tone are listed in Table 39-1.
Anaphylaxis is one result of type I allergic reactions. It begins within seconds to minutes after exposure to a specific allergen in a susceptible person. The result is widespread loss of blood vessel tone and decreased cardiac output. Table 22-2 (in Chapter 22) lists common allergens that can cause anaphylaxis. Chapter 22 describes the pathophysiology, prevention, and care of the patient with anaphylactic shock.
Obstructive shock is caused by problems that impair the ability of the normal heart muscle to pump effectively. The heart itself remains normal, but conditions outside the heart prevent either adequate filling of the heart or adequate contraction of the healthy heart muscle. The most common causes of obstructive shock are pericarditis and cardiac tamponade (see Table 39-1). Care of the person with cardiac tamponade is presented in detail in Chapter 37 (pericarditis) and Chapter 40 (as a complication after cardiac bypass graft surgery).
Although the causes and initial manifestations associated with the different types of shock vary, eventually the effects of hypotension and anaerobic cellular metabolism (metabolism without oxygen) result in the common key features of shock listed in Chart 39-1. The origin of these features is explained below in the discussion of Pathophysiology in the Hypovolemic Shock section.
Physiological Integrity
A. The blood, blood vessels, and heart are directly connected to each other so that when one is affected, all three are affected.
B. Because blood loss occurs with all types of shock, the most common first manifestation is hypotension.
C. Every type of shock interferes with oxygenation and metabolism of all cells in the same sequence.
D. The sympathetic nervous system is triggered by any type of shock and initiates the stress response.
Hypovolemic Shock
Pathophysiology
The basic problem of hypovolemic shock is a loss of blood volume from the vascular space, resulting in a decreased mean arterial pressure (MAP) (see Fig. 39-2) and a loss of oxygen-carrying capacity from the loss of circulating red blood cells (RBCs). The reduced MAP slows blood flow, resulting in decreased tissue perfusion. The loss of RBCs decreases the ability of the blood to oxygenate the tissue it does reach. These oxygenation and perfusion problems lead to cellular anaerobic (without oxygen) conditions and abnormal cellular metabolism.
If the events that caused the initial decrease in MAP are halted now, compensatory mechanisms provide adequate oxygenation and perfusion without outside intervention. If the initiating events continue and MAP decreases further, some tissues function under anaerobic conditions. This condition increases lactic acid levels and other harmful metabolites (e.g., protein-destroying enzymes, oxygen free radicals). These substances cause electrolyte and acid-base imbalances with tissue-damaging effects and depressed heart muscle activity. These effects are temporary and reversible if the cause of shock is corrected within 1 to 2 hours after onset. When shock conditions continue for longer periods without help, the resulting acid-base imbalance, electrolyte imbalances, and increased metabolites cause so much cell damage in vital organs that multiple organ dysfunction syndrome (MODS) occurs and recovery from shock is no longer possible. Table 39-2 summarizes the responses during the progression of shock.
TABLE 39-2 ADAPTIVE RESPONSES AND EVENTS DURING HYPOVOLEMIC SHOCK
| Initial Stage |
| Nonprogressive Stage |
| Progressive Stage |
| Refractory Stage |
Stages of Shock
Nonprogressive Stage of Shock (Compensatory Stage)
The kidneys and baroreceptors sense an ongoing decrease in MAP and trigger the release of renin, antidiuretic hormone (ADH), aldosterone, epinephrine, and norepinephrine to start kidney compensation. Renin, secreted by the kidney, causes decreased urine output, increased sodium reabsorption, and widespread blood vessel constriction (see Fig. 13-6 in Chapter 13). ADH increases water reabsorption in the kidney, further reducing urine output, and also causes blood vessel constriction in the skin and other less vital tissue areas. Together these actions compensate for shock by maintaining the fluid volume within the central blood vessels.
If the patient is stable and compensatory mechanisms are supported by medical and nursing interventions, he or she can remain in this stage for hours without having permanent damage. Stopping the conditions that started the shock at this stage and providing supportive interventions can prevent the shock from progressing. The cellular effects of this stage are reversible when nurses recognize the problem and coordinate with the health care team to start appropriate interventions (Mattiace, 2008; Stricker, 2010).
Etiology
Hypovolemic shock from external hemorrhage is common after trauma and surgery. Hypovolemic shock from internal hemorrhage occurs with blunt trauma, GI ulcers, and poor control of surgical bleeding. Hemorrhage also can be caused by any problem that reduces the levels of clotting factors (see Table 39-1). Hypovolemia as a result of dehydration can be caused by any problem that decreases fluid intake or increases fluid loss (see Table 39-1).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree