M. Linda Workman
Care of Patients with Problems of the Thyroid and Parathyroid Glands
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
7 Compare the clinical manifestations of hyperthyroidism with those of hypothyroidism.
10 Identify teaching priorities for the patient taking thyroid hormone replacement therapy.
11 Compare the clinical manifestations of hyperparathyroidism with those of hypoparathyroidism.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
The thyroid and parathyroid glands secrete hormones that affect overall metabolism, electrolyte balance, and excitable membrane activity. Thus problems of either gland usually have widespread effects and manifestations. Mild disturbances produce subtle problems. More severe disturbances may produce life-threatening problems.
Thyroid Disorders
Hyperthyroidism
Pathophysiology
Hyperthyroidism is excessive thyroid hormone secretion from the thyroid gland. The manifestations of hyperthyroidism are called thyrotoxicosis, regardless of the origin of the thyroid hormones (Davies & Larsen, 2008). (For example, a person who takes a large amount of synthetic thyroid hormones can have thyrotoxicosis but does not have hyperthyroidism.) Thyroid hormones increase metabolism in all body organs, and excesses produce many different manifestations. Hyperthyroidism can be temporary or permanent, depending on the cause.
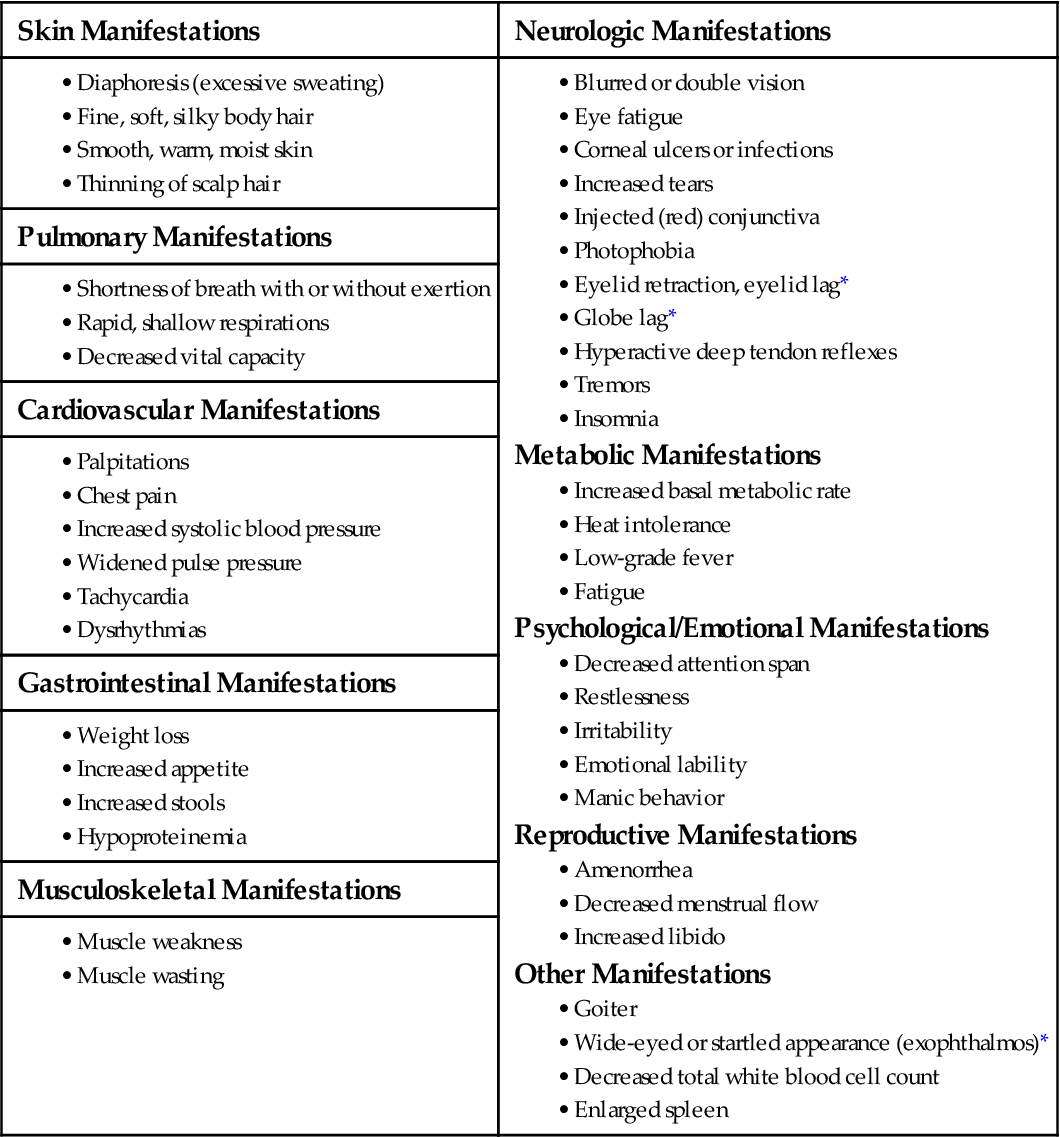
In hyperthyroidism the excessive thyroid hormones stimulate most body systems, causing hypermetabolism and increased sympathetic nervous system activity. Many of the manifestations are caused by the body’s response to the demands of hypermetabolism (Chart 66-1).
Thyroid hormones stimulate the heart, increasing both heart rate and stroke volume. These responses increase cardiac output, systolic blood pressure, and blood flow (Burton, 2011).
Elevated thyroid hormone levels affect protein, lipid, and carbohydrate metabolism. Protein synthesis (buildup) and degradation (breakdown) are increased, but breakdown exceeds buildup, causing a net loss of body protein known as a negative nitrogen balance. Glucose tolerance is decreased, and the patient has hyperglycemia (elevated blood glucose levels). Fat metabolism is increased, and body fat decreases. Although the patient has an increased appetite, the increased metabolism causes weight loss and nutritional deficiency.
Thyroid hormones are produced in response to the stimulation hormones secreted by the hypothalamus and anterior pituitary glands. Thus oversecretion of thyroid hormones changes the secretion of hormones from the hypothalamus and anterior pituitary gland through negative feedback (see Chapter 64). Thyroid hormones also have some influence over sex hormone production in both men and women. Women have menstrual problems and decreased fertility. Both men and women with hyperthyroidism have an increased libido (sexual urge or interest).
Etiology and Genetic Risk
Hyperthyroidism has many causes, the most common of which is Graves’ disease, also called toxic diffuse goiter. Graves’ disease is an autoimmune disorder in which antibodies (thyroid-stimulating immunoglobulins [TSIs]) are made and attach to the thyroid-stimulating hormone (TSH) receptors on the thyroid tissue. The thyroid gland responds by increasing the number and size of glandular cells, which enlarges the gland, forming a goiter, and overproduces thyroid hormones (thyrotoxicosis). Other manifestations specific to Graves’ disease include exophthalmos (abnormal protrusion of the eyes) and pretibial myxedema (dry, waxy swelling of the front surfaces of the lower legs). Not all patients with a goiter have hyperthyroidism.
Hyperthyroidism caused by multiple thyroid nodules is termed toxic multinodular goiter. The nodules may be enlarged thyroid tissues or benign tumors (adenomas). These patients usually have had a goiter for years. The overproduction of thyroid hormones is milder than that seen in Graves’ disease, and the patient does not have exophthalmos or pretibial edema.
Hyperthyroidism also can be caused by excessive use of thyroid replacement hormones. This type of problem is called exogenous hyperthyroidism.
Incidence/Prevalence
Hyperthyroidism is a common endocrine disorder. Graves’ disease can occur at any age but is diagnosed most often in women between 20 and 40 years of age, affecting women about ten times more often than men (Davies & Larsen, 2008). Toxic multinodular goiter usually occurs after the age of 50 and affects women four times more often than men (McCance et al, 2010).
Patient-Centered Collaborative Care
Assessment
History
The patient may have noticed many changes and problems because hyperthyroidism affects all body systems, although changes may occur over such a long period that not all patients are aware of them. Record age, gender, and usual weight. The patient may report a recent unplanned weight loss, an increased appetite, and an increase in the number of bowel movements per day.
A hallmark of hyperthyroidism is heat intolerance. The patient may have diaphoresis (increased sweating) even when environmental temperatures are comfortable for others. He or she often wears lighter clothing in cold weather. The patient may also report palpitations or chest pain as a result of the cardiovascular effects. Ask about changes in breathing patterns, because dyspnea (with or without exertion) is common.
Visual changes may be the earliest problem the patient notices, especially exophthalmos with Graves’ disease (Fig. 66-1). Ask about changes in vision, such as blurring or double vision and tiring of the eyes.

Ask whether he or she has noticed a change in energy level or in the ability to perform ADLs. Fatigue, weakness, and insomnia are common. Family and friends may report that the patient has become irritable or depressed.
Ask women about changes in menses, because amenorrhea or a decreased menstrual flow is common. Initially, both men and women may have an increase in libido, but this changes as the patient becomes more fatigued.
Explore the patient’s medical history. Information about previous thyroid surgery or radiation therapy to the neck is important to obtain because some people remain hyperthyroid after surgery or are resistant to radiation therapy. Ask about past and current drugs, especially the use of thyroid hormone replacement or antithyroid drugs.
Physical Assessment/Clinical Manifestations
Exophthalmos is common in patients with Graves’ disease. The wide-eyed or “startled” look is due to edema in the extraocular muscles and increased fatty tissue behind the eye, which pushes the eyeball forward. Pressure on the optic nerve may impair vision. Swelling and shortening of the muscles may cause problems with focusing. If the eyelid fails to close completely and the eye is unprotected, the eye may become overly dry and develop corneal ulcers or infection. Observe the patient’s eyes for excessive tearing and a bloodshot appearance, and ask about sensitivity to light (photophobia).
Observe the patient’s general appearance. In addition to the exophthalmos of Graves’ disease, two other eye problems are common in all types of hyperthyroidism: eyelid retraction (eyelid lag) and globe (eyeball) lag. In eyelid lag, the upper eyelid fails to descend when the patient gazes slowly downward. In globe lag, the upper eyelid pulls back faster than the eyeball when the patient gazes upward. During assessment, ask the patient to look down and then up, and document the response.
Observe the size and symmetry of the thyroid gland. Palpate the thyroid gland to assess the presence of a mass or general enlargement. In goiter, a generalized thyroid enlargement, the thyroid gland may increase to four times its normal size (Fig. 66-2). Goiters are common in Graves’s disease and are classified by size (Table 66-1). Bruits (turbulence from increased blood flow) may be heard in the neck with a stethoscope. (See Chapter 64 for thyroid palpation and auscultation.)

TABLE 66-1
| GOITER GRADE | DESCRIPTION |
| 0 | No palpable or visible goiter. |
| 1 | Mass is not visible with neck in the normal position. Goiter can be palpated and moves up when the patient swallows. |
| 2 | Mass is visible as swelling when the neck is in the normal position. Goiter is easily palpated and is usually asymmetric. |
The cardiovascular problems of hyperthyroidism include increased systolic blood pressure, tachycardia, and dysrhythmias. Usually the diastolic pressure is decreased, causing a widened pulse pressure.
Inspect the hair and skin. Fine, soft, silky hair and smooth, warm, moist skin are common. Muscle weakness and hyperactive deep tendon reflexes are common. Observe motor movements of the hands for tremors. The patient may appear restless, irritable, and fatigued.
Psychosocial Assessment
The patient with hyperthyroidism often has wide mood swings, irritability, decreased attention span, and manic behavior. Hyperactivity often leads to fatigue because of the inability to sleep well. Some patients describe their activity as having two modes—either “full speed ahead” or “completely stopped.” Ask whether he or she cries or laughs without cause or has difficulty concentrating. Family members often report a change in the patient’s mental or emotional status.
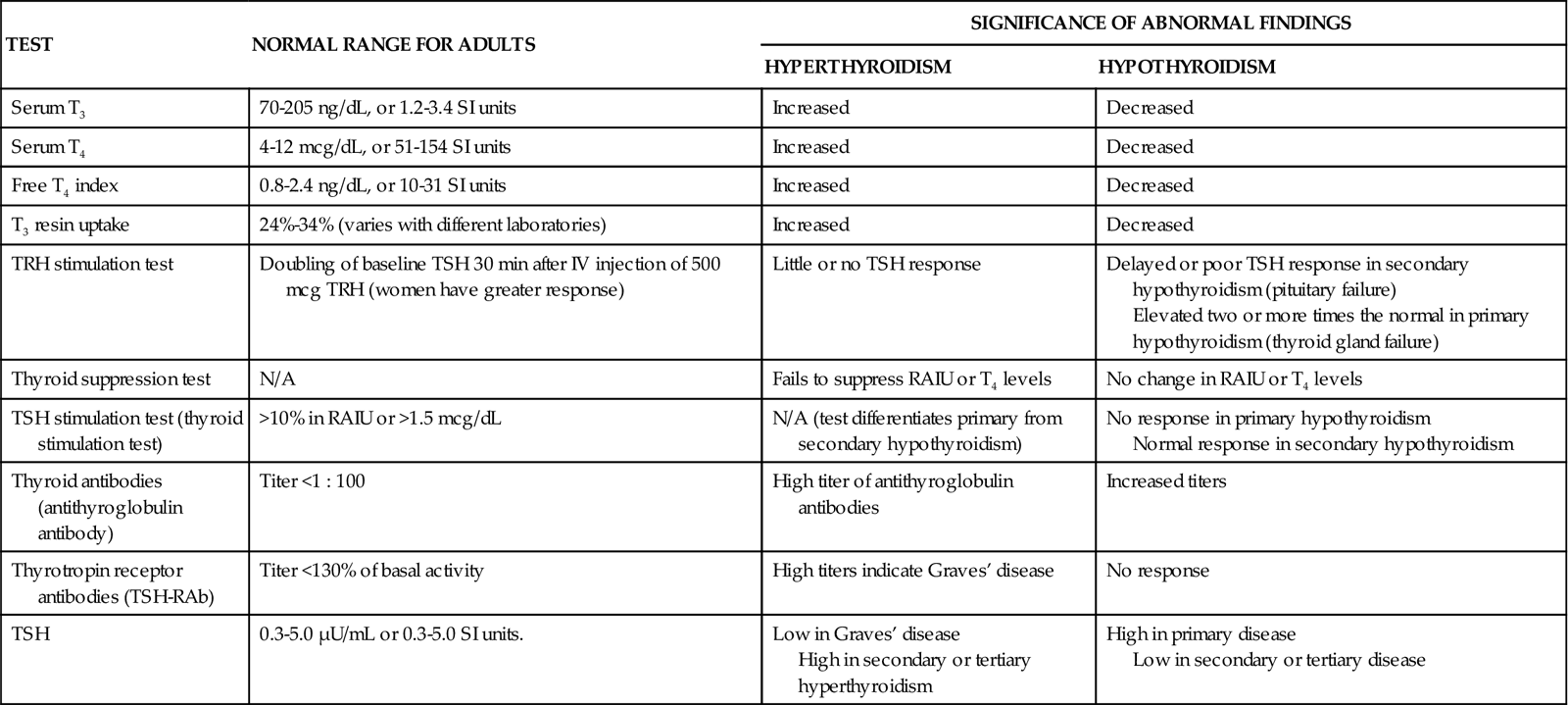
Laboratory Assessment
Testing for hyperthyroidism involves measurement of blood values for triiodothyronine (T3), thyroxine (T4), T3 resin uptake (T3RU), and thyroid-stimulating hormone (TSH). Antibodies to TSH (TSH-RAb) are measured to diagnose Graves’ disease. The most common changes in laboratory tests for Graves’ disease and other forms of hyperthyroidism are listed in Chart 66-2.
Other Diagnostic Assessment
Thyroid scan evaluates the position, size, and functioning of the thyroid gland. Radioactive iodine (RAI [123I]) is given by mouth, and the uptake of iodine by the thyroid gland (radioactive iodine uptake [RAIU]) is measured. The half-life of 123I is short, and radiation precautions are not needed. Pregnancy should be ruled out before the scan is performed. The normal thyroid gland has an uptake of 5% to 35% of the given dose at 24 hours. RAIU is increased in hyperthyroidism.
Assess whether the patient has undergone procedures or has taken drugs that might affect the results of the scan. Procedures that use iodine-containing dye (e.g., renography) should not be performed for at least 4 weeks before a thyroid scan is done. Any drug that contains iodine should be discontinued for 1 week before the scan.
Ultrasonography of the thyroid gland can determine its size and the general composition of any masses or nodules. This procedure takes about 30 minutes to perform and is painless.
Electrocardiography (ECG) usually shows tachycardia. Other ECG changes with hyperthyroidism include atrial fibrillation, dysrhythmias, and changes in P and T waveforms.
Interventions
Because Graves’ disease is the most common form of hyperthyroidism, the interventions discussed in the following sections include those specific for the problems that occur with Graves’ disease. The purposes of medical management are to decrease the effect of thyroid hormone on cardiac function and to reduce thyroid hormone secretion. The priorities for nursing care focus on monitoring for complications, reducing stimulation, promoting comfort, and teaching the patient and family about therapeutic drugs and procedures.
Nonsurgical Management
Monitoring includes measuring the patient’s apical pulse, blood pressure (BP), and temperature at least every 4 hours. Instruct the patient to report immediately any palpitations, dyspnea, vertigo, or chest pain. Increases in temperature may indicate a rapid worsening of the patient’s condition and the onset of thyroid storm, a life-threatening event that occurs with uncontrolled hyperthyroidism and is characterized by high fever and severe hypertension. Immediately report a temperature increase of even one degree Fahrenheit. If this task is delegated to unlicensed assistive personnel (UAP), instruct them to report the patient’s temperature to you as soon as it has been obtained. If a temperature elevation is reported, immediately assess the patient’s cardiac status. If the patient has a cardiac monitor, check for dysrhythmias.
Reducing stimulation is important because a noisy or stressful environment can increase the manifestations of hyperthyroidism and increase the risk for cardiac complications. Encourage the patient to rest. Keep the environment as quiet as possible by closing the door to his or her room, limiting visitors, and eliminating or postponing nonessential care or treatments.
Promoting comfort can be accomplished through actions such as reducing the room temperature to decrease discomfort caused by heat intolerance. Instruct UAP to ensure the patient always has a fresh pitcher of ice water and to change the bed linen whenever it becomes damp from diaphoresis. Suggest that the patient take a cool shower several times each day. If showering is not possible, cool sponge baths may increase comfort. Prevent eye dryness in patients with exophthalmos by encouraging the use of artificial tears and by taping the eyelids closed for sleep.
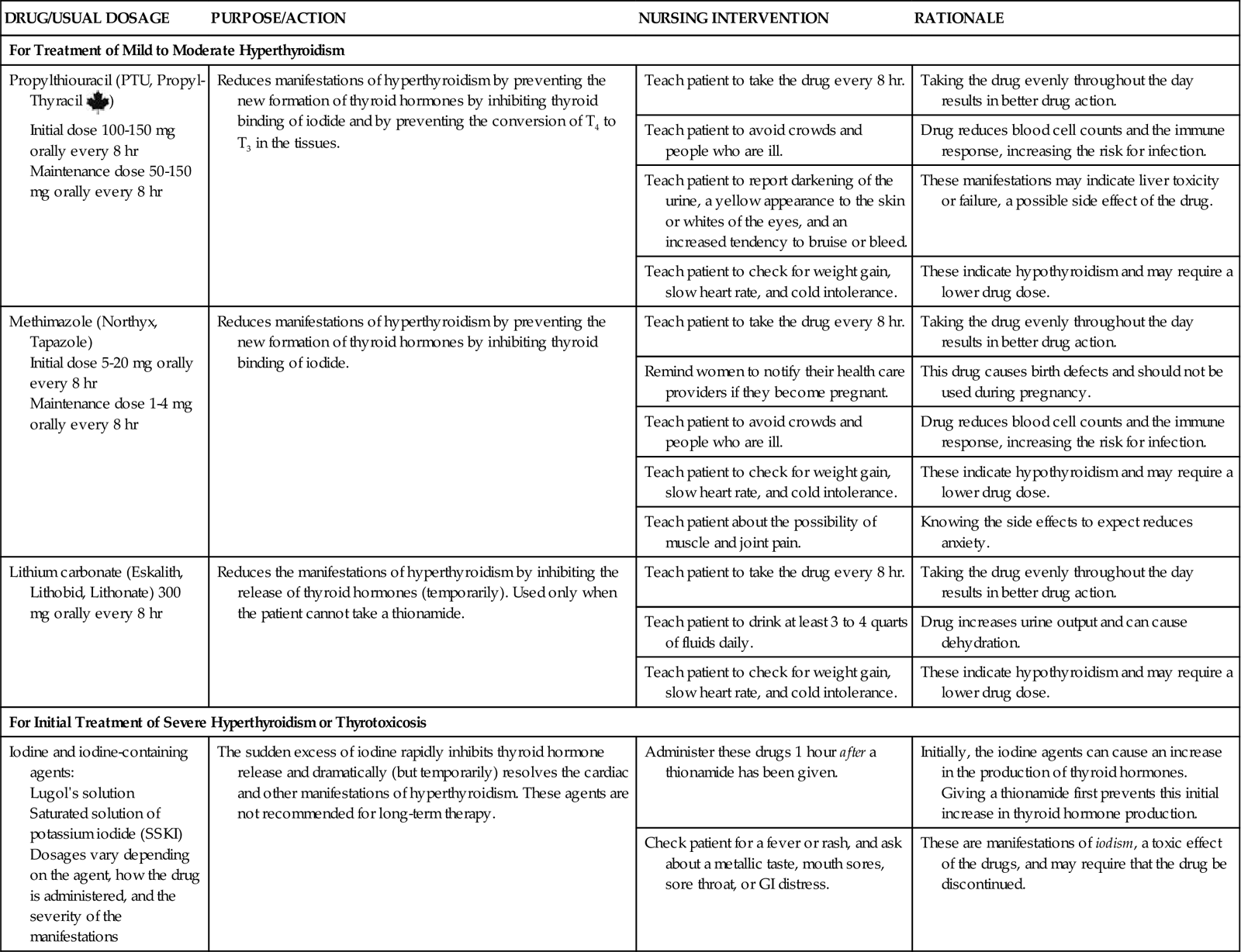
Drug therapy with antithyroid drugs is the initial treatment of hyperthyroidism. Chart 66-3 lists teaching priorities for the patient receiving drug therapy for hyperthyroidism. The preferred drugs are the thionamides, which include propylthiouracil (PTU) and methimazole (Tapazole). These drugs block thyroid hormone production by preventing iodide binding in the thyroid gland (see Chart 66-3). In addition, PTU also prevents T4 from being converted to the more powerful T3 in the tissues. Methimazole doses are lower than PTU doses. The response to these drugs is delayed because the patient may have large amounts of stored thyroid hormones that continue to be released.
Iodine preparations may be used for short-term therapy before surgery. They decrease blood flow through the thyroid gland, reducing the production and release of thyroid hormone. Improvement usually occurs within 2 weeks, but it may be weeks before metabolism returns to normal. This treatment can result in hypothyroidism, and the patient is monitored closely for the need to adjust the drug regimen.
Lithium also inhibits thyroid hormone release. However, its use is limited because of side effects such as depression, diabetes insipidus, tremors, nausea, and vomiting. Lithium may be used for a patient who cannot tolerate other antithyroid drugs.
Beta-adrenergic blocking drugs, such as propranolol (Inderal, Detensol ![]() ) may be used as supportive therapy. These drugs relieve diaphoresis, anxiety, tachycardia, and palpitations but do not inhibit thyroid hormone production. See Chapters 36 and 40 for a discussion of the actions and nursing implications of these agents.
) may be used as supportive therapy. These drugs relieve diaphoresis, anxiety, tachycardia, and palpitations but do not inhibit thyroid hormone production. See Chapters 36 and 40 for a discussion of the actions and nursing implications of these agents.
Radioactive iodine (RAI) therapy is not used in pregnant women because 131I crosses the placenta and can damage the fetal thyroid gland. The patient with hyperthyroidism may receive RAI in the form of oral 131I. The dosage depends on the thyroid gland’s size and sensitivity to radiation. The thyroid gland picks up the RAI, and some of the cells that produce thyroid hormone are destroyed by the local radiation. Because the thyroid gland stores thyroid hormones to some degree, the patient may not have complete symptom relief until 6 to 8 weeks after RAI therapy. Additional drug therapy for hyperthyroidism is still needed during the first few weeks after RAI treatment.
RAI therapy is performed on an outpatient basis. One dose may be sufficient, although some patients need a second or third dose. The radiation dose is low and is usually completely eliminated within a month; however, the source is unsealed, and some radioactivity is present in the patient’s body fluids and stool for a few weeks after therapy (Al-Shakhrah, 2008). Radiation precautions are needed to prevent exposure to family members and other people. Chart 66-4 lists precautions to teach the patient during the first few weeks after receiving 131I.