Donna D. Ignatavicius
Care of Patients with Liver Problems
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
7 Explain the pathophysiology and complications associated with cirrhosis of the liver.
8 Interpret laboratory test findings commonly seen in patients with cirrhosis.
9 Analyze assessment data from patients with cirrhosis to determine priority patient problems.
10 Develop a collaborative plan of care for the patient with late-stage cirrhosis.
12 Identify emergency interventions for the patient with bleeding esophageal varices.
13 Explain the role of the nurse when assisting with a paracentesis procedure.
14 Compare and contrast the transmission of hepatitis viral infections.
15 Explain ways in which each type of hepatitis can be prevented.
16 Identify potentially life-threatening complications of liver trauma.
17 Describe treatment options for patients with cancer of the liver.
18 Describe the common complications that result from liver transplantation.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
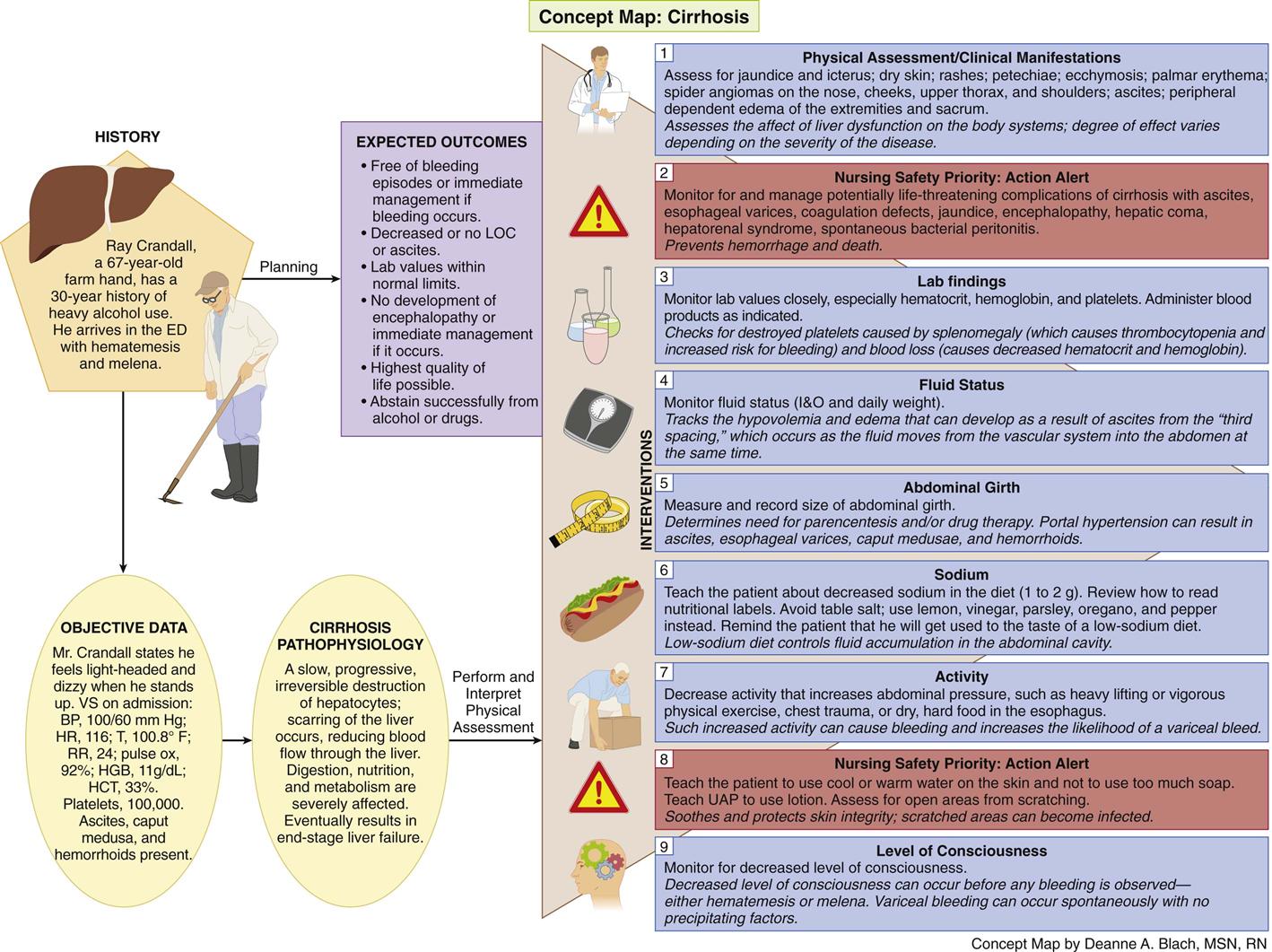
Concept Map: Cirrhosis
Key Points
Review Questions for the NCLEX® Examination
The liver is the largest and one of the most vital internal organs, performing more than 400 functions and affecting every system in the body. When the liver is diseased or damaged, it cannot provide these activities. As a result, digestion, nutrition, and metabolism can be severely affected. Liver diseases range in severity from mild hepatic inflammation to chronic end-stage cirrhosis.
Cirrhosis
Cirrhosis is extensive, irreversible scarring of the liver, usually caused by a chronic reaction to hepatic inflammation and necrosis. The disease typically develops slowly and has a progressive, prolonged, destructive course resulting in end-stage liver disease. The most common causes for cirrhosis in the United States are hepatitis C, alcoholism, and biliary obstruction. Worldwide, hepatitis B and hepatitis D are the leading causes. Without liver transplantation, cirrhosis is usually fatal (Kelso, 2008).
Pathophysiology
Cirrhosis is characterized by widespread fibrotic (scarred) bands of connective tissue that change the liver’s normal makeup. Inflammation caused by either toxins or disease results in extensive degeneration and destruction of hepatocytes (liver cells). As cirrhosis develops, the tissue becomes nodular. These nodules can block bile ducts and normal blood flow throughout the liver. Impairments in blood and lymph flow result from compression caused by excessive fibrous tissue. In early disease, the liver is usually enlarged, firm, and hard. As the pathologic process continues, the liver shrinks in size, resulting in decreased liver function, which can occur in weeks to years. Some patients with cirrhosis have no symptoms until serious complications occur. The impaired liver function results in elevated serum liver enzymes (Pagana & Pagana, 2010).
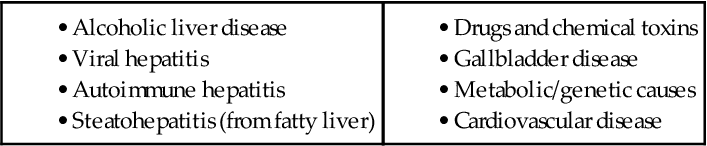
Cirrhosis of the liver can be divided into several common types, depending on the cause of the disease (McCance et al., 2010):
Complications of Cirrhosis
Common problems and complications associated with hepatic cirrhosis depend on the amount of damage sustained by the liver. In compensated cirrhosis, the liver is scarred but can still perform essential functions without causing major symptoms. In decompensated cirrhosis, liver function is impaired with obvious manifestations of liver failure.
The loss of hepatic function contributes to the development of metabolic abnormalities. Hepatic cell damage may lead to these common complications:
• Ascites and esophageal varices
• Jaundice
• Portal-systemic encephalopathy (PSE) with hepatic coma
Portal Hypertension.
Portal hypertension, a persistent increase in pressure within the portal vein greater than 5 mm Hg, is a major complication of cirrhosis (Minano & Garcia-Tsao, 2010). It results from increased resistance to or obstruction (blockage) of the flow of blood through the portal vein and its branches. The blood meets resistance to flow and seeks collateral (alternative) venous channels around the high-pressure area.
Blood flow backs into the spleen, causing splenomegaly (spleen enlargement). Veins in the esophagus, stomach, intestines, abdomen, and rectum become dilated. Portal hypertension can result in ascites (abdominal fluid), esophageal varices (distended veins), prominent abdominal veins (caput medusae), and hemorrhoids.
Ascites and Esophageal Varices.
Ascites is the collection of free fluid within the peritoneal cavity caused by increased hydrostatic pressure from portal hypertension (McCance et al., 2010). The collection of plasma protein in the peritoneal fluid reduces the amount of circulating plasma protein in the blood. When this decrease is combined with the inability of the liver to produce albumin because of impaired liver cell functioning, the serum colloid osmotic pressure is decreased in the circulatory system. The result is a fluid shift from the vascular system into the abdomen, a form of “third spacing.” As a result, the patient may have hypovolemia and edema at the same time.
Massive ascites may cause renal vasoconstriction, triggering the renin-angiotensin system. This results in sodium and water retention, which increases hydrostatic pressure and the vascular volume and leads to more ascites.
As a result of portal hypertension, the blood backs up from the liver and enters the esophageal and gastric veins. Esophageal varices occur when fragile, thin-walled esophageal veins become distended and tortuous from increased pressure. The potential for varices to bleed depends on their size; size is determined by direct endoscopic observation. Varices occur most often in the distal esophagus but can also be present in the stomach and rectum.
Bleeding esophageal varices is a life-threatening medical emergency. Severe blood loss may occur, resulting in shock from hypovolemia. The bleeding may be either hematemesis (vomiting blood) or melena (black, tarry stools). Loss of consciousness may occur before any observed bleeding. Variceal bleeding can occur spontaneously with no precipitating factors. However, any activity that increases abdominal pressure may increase the likelihood of a variceal bleed, including heavy lifting or vigorous physical exercise. In addition, chest trauma or dry, hard food in the esophagus can cause bleeding.
Patients with portal hypertension may also have portal hypertensive gastropathy. This complication can occur with or without esophageal varices. Slow gastric mucosal bleeding occurs, which may result in chronic slow blood loss, occult-positive stools, and anemia.
Splenomegaly (enlarged spleen) results from the backup of blood into the spleen. The enlarged spleen destroys platelets, causing thrombocytopenia (low serum platelet count) and increased risk for bleeding. Thrombocytopenia is often the first clinical sign that a patient has liver dysfunction.
Biliary Obstruction.
In patients with cirrhosis, the production of bile in the liver is decreased. This prevents the absorption of fat-soluble vitamins (e.g., vitamin K). Without vitamin K, clotting factors II, VII, IX, and X are not produced in sufficient quantities and the patient is susceptible to bleeding and easy bruising. These abnormalities are confirmed by coagulation studies.
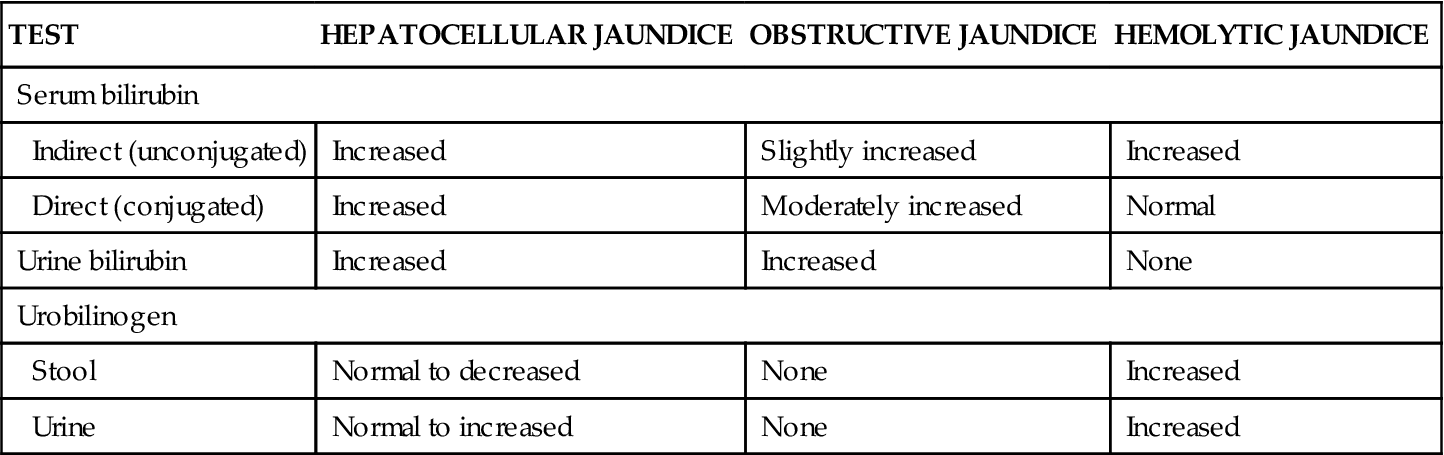
Jaundice (yellowish coloration of the skin) in patients with cirrhosis is caused by one of two mechanisms: hepatocellular disease or intrahepatic obstruction (Table 61-1). Hepatocellular jaundice develops because the liver cells cannot effectively excrete bilirubin. This decreased excretion results in excessive circulating bilirubin levels. Intrahepatic obstructive jaundice results from edema, fibrosis, or scarring of the hepatic bile channels and bile ducts, which interferes with normal bile and bilirubin excretion. Patients with jaundice often report pruritus (itching).
TABLE 61-1
LABORATORY DIAGNOSTIC DIFFERENTIATION OF JAUNDICE
| TEST | HEPATOCELLULAR JAUNDICE | OBSTRUCTIVE JAUNDICE | HEMOLYTIC JAUNDICE |
| Serum bilirubin | |||
| Indirect (unconjugated) | Increased | Slightly increased | Increased |
| Direct (conjugated) | Increased | Moderately increased | Normal |
| Urine bilirubin | Increased | Increased | None |
| Urobilinogen | |||
| Stool | Normal to decreased | None | Increased |
| Urine | Normal to increased | None | Increased |
Hepatic Encephalopathy.
Hepatic encephalopathy (also called portal-systemic encephalopathy [PSE]) is a complex cognitive syndrome that results from liver failure and cirrhosis. Patients report sleep disturbance, mood disturbance, mental status changes, and speech problems early as this complication begins. Hepatic encephalopathy may be reversible with early intervention. Later neurologic symptoms include an altered level of consciousness, impaired thinking processes, and neuromuscular problems.
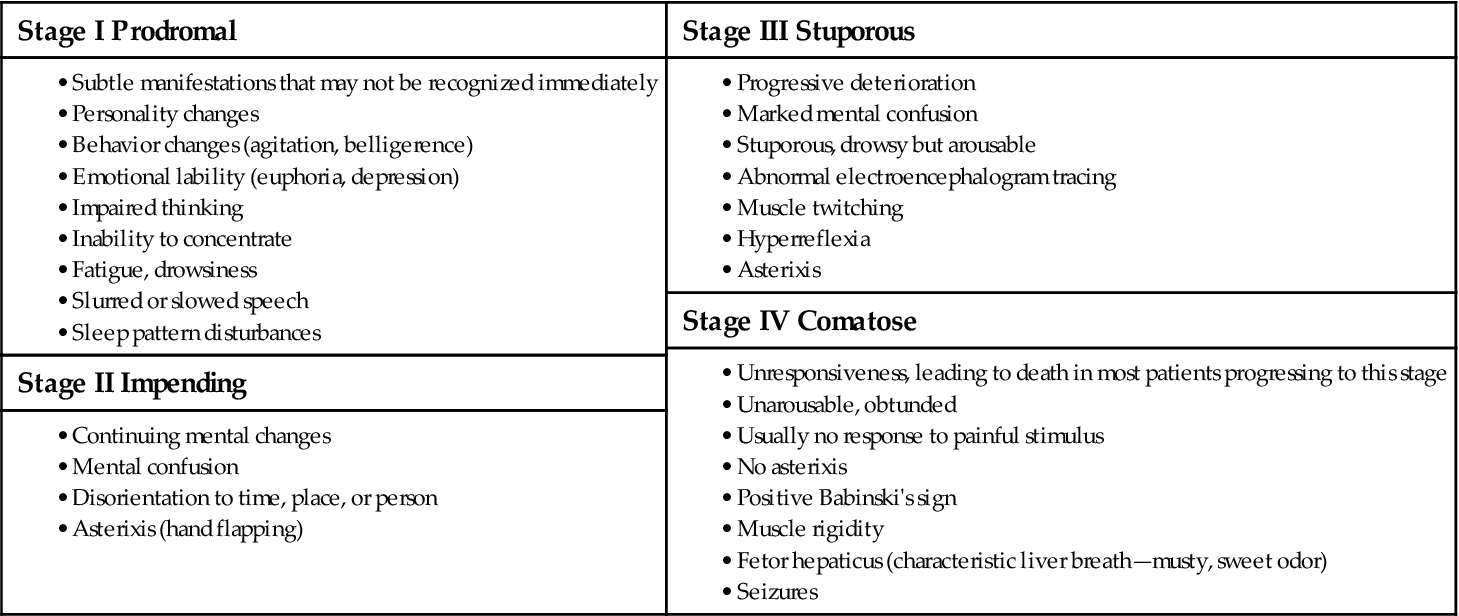
Hepatic encephalopathy may develop slowly in patients with chronic liver disease and go undetected until the late stages. Symptoms develop rapidly in acute liver dysfunction. Four stages of development have been identified: prodromal, impending, stuporous, and comatose (Table 61-2). The patient’s symptoms may gradually progress to coma or fluctuate among the four stages.
TABLE 61-2
STAGES OF PORTAL-SYSTEMIC ENCEPHALOPATHY
The exact mechanisms causing hepatic encephalopathy are not clearly understood but probably are the result of the shunting of portal venous blood into the central circulation so that the liver is bypassed. As a result, substances absorbed by the intestine are not broken down or detoxified and may lead to metabolic abnormalities, such as elevated serum ammonia and gamma-aminobutyric acid (GABA) (Kelso, 2008). Elevated serum ammonia results from the inability of the liver to detoxify protein by-products and is common in patients with hepatic encephalopathy. However, it is not a clear indicator of the presence of encephalopathy. Some patients may have major impairment without high elevations of serum ammonia, and elevations of ammonia can occur without evidence of encephalopathy.
Factors that may lead to hepatic encephalopathy in patients with cirrhosis include:
• Hypovolemia (decreased fluid volume)
• Hypokalemia (decreased serum potassium)
• GI bleeding (causes a large protein load in the intestines)
• Drugs (e.g., hypnotics, opioids, sedatives, analgesics, diuretics, illicit drugs)
The prognosis depends on the severity of the underlying cause, the precipitating factors, and the degree of liver dysfunction.
Other Complications.
The development of hepatorenal syndrome (HRS) indicates a poor prognosis for the patient with liver failure. It is often the cause of death in these patients. This syndrome is manifested by:
HRS often occurs after clinical deterioration from GI bleeding or the onset of hepatic encephalopathy. It may also complicate other liver diseases, including acute hepatitis and fulminant liver failure.
Patients with cirrhosis and ascites may develop acute spontaneous bacterial peritonitis (SBP). Those who are particularly susceptible are patients with very advanced liver disease. This may be the result of low concentrations of proteins; proteins normally provide some protection against bacteria.
The bacteria responsible for SBP are typically from the bowel and reach the ascitic fluid after migrating through the bowel wall and transversing the lymphatics. Clinical manifestations vary but may include fever, chills, and abdominal pain and tenderness. However, manifestations can also be minimal with only mild symptoms in the absence of fever. Worsening encephalopathy and increased jaundice may also be present without abdominal symptoms.
The diagnosis of SBP is made when a sample of ascitic fluid is obtained by paracentesis for cell counts and culture. An ascitic fluid leukocyte count of more than 250 polymorphonuclear (PMN) leukocytes may indicate the need for treatment.
Etiology and Genetic Risk
Hepatitis C is the leading cause of cirrhosis and liver failure in the United States. It is an infectious bloodborne illness that usually causes chronic disease. Inflammation caused by infection over time leads to progressive scarring of the liver. It usually takes decades for cirrhosis to develop, although alcohol use in combination with hepatitis C may speed the process.
Hepatitis B and hepatitis D are the most common causes of cirrhosis worldwide. Hepatitis B also causes inflammation and low-grade damage over decades that can ultimately lead to cirrhosis. Hepatitis D is another virus that infects the liver but only in people who already have hepatitis B (see discussion of hepatitis on p. 1305).
Cirrhosis can occur as a result of other factors. For example, alcohol has a direct toxic effect on the hepatocytes and causes liver inflammation (alcoholic hepatitis). The liver becomes enlarged, with cellular degeneration and infiltration by fat, leukocytes, and lymphocytes. Over time, the inflammatory process decreases and the destructive phase increases. Early scar formation is caused by fibroblast infiltration and collagen formation. Damage to the liver tissue progresses as malnutrition and repeated exposure to the alcohol continue. If alcohol is withheld, the fatty infiltration and inflammation is reversible. If alcohol abuse continues, widespread scar tissue formation and fibrosis infiltrate the liver as a result of cellular necrosis. The long-term use of illicit drugs, such as cocaine, has similar effects on the liver.
The amount of alcohol necessary to cause cirrhosis varies widely from person to person, and there are gender differences. In women, it may take as few as two to three drinks per day over a minimum of 10 years. In men, perhaps six drinks per day over the same time period may be needed to cause disease. Binge drinking can increase risk for hepatitis and fatty liver.
Biliary cirrhosis occurs as a result of obstruction of the bile duct, usually from gallbladder disease or an autoimmune form of the disease called primary biliary cirrhosis (PBC). Patients with PBC typically have a genetic predisposition to the disease and a positive antimitochondrial antibody (AMA) (Lindor et al., 2009). Table 61-3 summarizes known causes of liver cirrhosis.
Incidence/Prevalence
The incidence of cirrhosis in the United States is not well known, but about 27,000 die from it each year. The disease affects twice as many men as women (Kelso, 2008).
Patient-Centered Collaborative Care
Assessment
History
Obtain data from patients with suspected cirrhosis, including age, gender, and employment history, especially history of exposure to alcohol, drugs (prescribed and illicit), and chemical toxins. Keep in mind that all exposures are important regardless of how long ago they occurred. Determine whether there has ever been a needle stick injury. Sexual history and orientation may be important in determining an infectious cause for liver disease, because men having sex with men (MSM) are at high risk for hepatitis A, hepatitis B, and hepatitis C. People with hepatitis can develop cirrhosis (American Liver Foundation, 2011).
Inquire about whether there is a family history of alcoholism and/or liver disease. Ask the patient to describe his or her alcohol intake, including the amount consumed during a given period. Is there a history of illicit drug use, including oral, IV, and intranasal forms? Is there a history of tattoos? Has the patient been in the military or in prison? Is the patient a health care worker, firefighter, or police officer? For patients previously or currently in an alcohol or drug recovery program, how long have they been sober? This information is sensitive and often difficult for the patient to answer. Be sure to establish why you are asking these questions, and accept answers in a nonjudgmental manner. Provide privacy during the interview. For many people, the behaviors causing the liver disease occurred years before the onset of their current illness and they are regretful and often embarrassed.
Ask the patient about previous medical conditions, such as an episode of jaundice or acute viral hepatitis, biliary tract disorders (such as cholecystitis), viral infections, surgery, blood transfusions, autoimmune disorders, obesity, altered lipid profile, heart failure, respiratory disorders, or liver injury.
Physical Assessment/Clinical Manifestations
Because cirrhosis has a slow onset, many of the early manifestations are vague and nonspecific. Assess for:
• Fatigue
• Significant change in weight
• GI symptoms, such as anorexia and vomiting
• Abdominal pain and liver tenderness (both of which may be ignored by the patient)
Liver function problems are often found during a routine physical examination or when laboratory tests are completed for an unrelated illness or problem. The patient with compensated cirrhosis may be completely unaware that there is a liver problem. The first sign may present before the onset of symptoms when routine laboratory tests, presurgical evaluations, or life and health insurance assessments show abnormalities. These tests could indicate abnormal liver function or thrombocytopenia, requiring a more thorough diagnostic workup.
The development of late signs of advanced cirrhosis (also called “end-stage liver failure”) usually causes the patient to seek medical treatment. GI bleeding, jaundice, ascites, and spontaneous bruising indicate poor liver function and complications of cirrhosis.
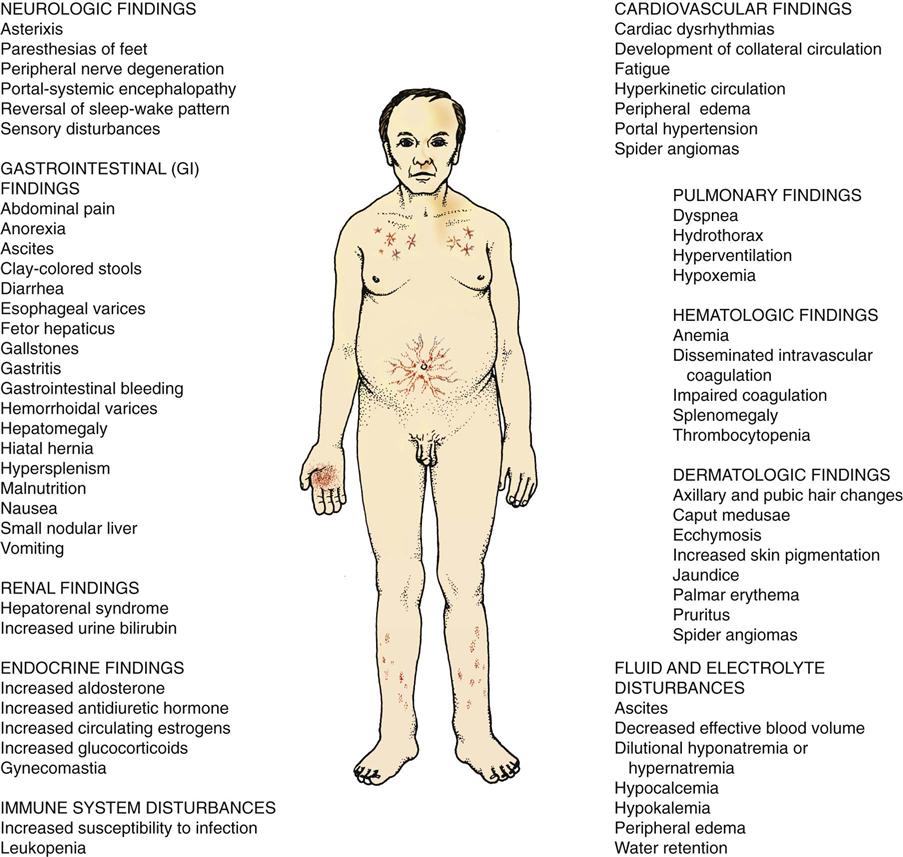
Thoroughly assess the patient with liver dysfunction or failure because it affects every body system (Fig. 61-1). The clinical picture and course vary from patient to patient depending on the severity of the disease. Assess for:
• Obvious yellowing of the skin (jaundice) and sclerae (icterus)
• Dry skin
• Rashes
• Warm and bright red palms of the hands (palmar erythema)
• Peripheral dependent edema of the extremities and sacrum
• Sicca syndrome (in patients with primary biliary cirrhosis [PBC]) (Lindor et al., 2009)
• Osteoporosis (especially in patients with PBC) (Lindor et al., 2009)
• Vitamin deficiency (especially fat-soluble vitamins A, D, E, and K)
Abdominal Assessment.
Massive ascites can be detected as a distended abdomen with bulging flanks. The umbilicus may protrude, and dilated abdominal veins (caput medusae) may radiate from the umbilicus. Ascites can cause physical problems. For example, orthopnea and dyspnea from increased abdominal distention can interfere with lung expansion. The patient may have difficulty maintaining an erect body posture, and problems with balance may affect walking. Inspect and palpate for the presence of inguinal or umbilical hernias, which are likely to develop because of increased intra-abdominal pressure.
Minimal ascites is often more difficult to detect, especially in the obese patient. Advanced assessment techniques, such as the percussion test for shifting dullness and the presence of a fluid wave, may be performed by the health care provider.
When performing an assessment of the abdomen, keep in mind that hepatomegaly (liver enlargement) occurs in many cases of early cirrhosis. Splenomegaly is common in nonalcoholic causes of cirrhosis. As the liver deteriorates, it may become hard and small. The advanced practice nurse or other health care provider palpates the right upper quadrant for hepatomegaly below the costal (rib cage) border. It may also be assessed by percussing for dullness over the enlarged liver.
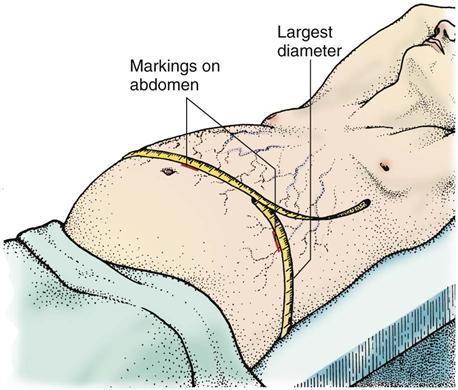
Measure the patient’s abdominal girth to evaluate the progression of ascites (Fig. 61-2). To measure abdominal girth, the patient lies flat while the nurse or other examiner pulls a tape measure around the largest diameter (usually over the umbilicus) of the abdomen. The girth is measured at the end of exhalation. Mark the abdominal skin and flanks to ensure the same tape measure placement on subsequent readings. Taking daily weights, however, is the most reliable indicator of fluid retention.
Other Physical Assessment.
Observe vomitus and stool for blood. This may be indicated by frank blood in the excrement or by a positive fecal occult blood test (FOBT) (Hema-Check, Hematest). Gastritis, stomach ulceration, or oozing esophageal varices may be responsible for the blood in the stool.
Note the presence of fetor hepaticus, which is the distinctive breath odor of chronic liver disease and hepatic encephalopathy and is characterized by a fruity or musty odor. Fetor hepaticus results from the inability of the damaged liver to metabolize and detoxify mercaptan, which is produced by bacterial breakdown of methionine, a sulfurous amino acid.
Amenorrhea (no menstrual period) may occur in women and men may exhibit testicular atrophy, gynecomastia (enlarged breasts), and impotence as a result of inactive hormones. Patients with problems of the hematologic system caused by hepatic failure may have bruising and petechiae (small, purplish hemorrhagic spots on the skin).
Continually assess the patient’s neurologic function. Subtle changes in mental status and personality often progress to coma, a late complication of encephalopathy. Monitor for asterixis, a coarse tremor characterized by rapid, nonrhythmic extensions and flexions in the wrists and fingers.
Psychosocial Assessment
The patient with hepatic cirrhosis may undergo subtle or obvious personality, cognitive, and behavior changes, such as agitation. He or she may experience sleep pattern disturbances or may exhibit signs of emotional lability (fluctuations in emotions), euphoria (a very elevated mood), or depression. A psychosocial assessment identifies needs and helps guide care.
Repeated hospitalizations are common for patients with cirrhosis. It is a life-altering chronic disease, impacting not only the patient but also the immediate and extended family members and significant others. There are significant emotional, physical, and financial changes. Substance abuse may continue even as health worsens. It is important, whenever possible, to use resources available to these patients and their families. Collaborate with social workers, substance abuse counselors, and mental health/behavioral health care professionals as needed for patient assessment and management.
Laboratory Assessment
Laboratory study abnormalities are common in patients with liver disease (Table 61-4). Serum levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), and lactate dehydrogenase (LDH) may be elevated because these enzymes are released into the blood during hepatic inflammation. However, as the liver deteriorates, the hepatocytes may be unable to create an inflammatory response and the AST and ALT may be normal. ALT levels are more specific to the liver whereas AST can be found in muscle, kidney, brain, and heart. An AST/ALT ratio greater than 2 is usually found in alcoholic liver disease.
TABLE 61-4
ASSESSMENT OF ABNORMAL LABORATORY FINDINGS IN LIVER DISEASE
| ABNORMAL FINDING | SIGNIFICANCE |
| Serum Enzymes | |
| Elevated serum aspartate aminotransferase (AST) | Hepatic cell destruction, hepatitis (most specific indicator) |
| Elevated serum alanine aminotransferase (ALT) | Hepatic cell destruction, hepatitis |
| Elevated lactate dehydrogenase (LDH) | Hepatic cell destruction |
| Elevated serum alkaline phosphatase | Obstructive jaundice, hepatic metastasis |
| Bilirubin | |
| Elevated serum total bilirubin | Hepatic cell disease |
| Elevated serum direct conjugated bilirubin | Hepatitis, liver metastasis |
| Elevated serum indirect unconjugated bilirubin | Cirrhosis |
| Elevated urine bilirubin | Hepatocellular obstruction, viral or toxic liver disease |
| Elevated urine urobilinogen | Hepatic dysfunction |
| Decreased fecal urobilinogen | Obstructive liver disease |
| Serum Proteins | |
| Increased serum total protein | Acute liver disease |
| Decreased serum total protein | Chronic liver disease |
| Decreased serum albumin | Severe liver disease |
| Elevated serum globulin | Immune response to liver disease |
| Other Tests | |
| Elevated serum ammonia | Advanced liver disease or portal-systemic encephalopathy (PSE) |
| Prolonged prothrombin time (PT) or international normalized ratio (INR) | Hepatic cell damage and decreased synthesis of prothrombin |
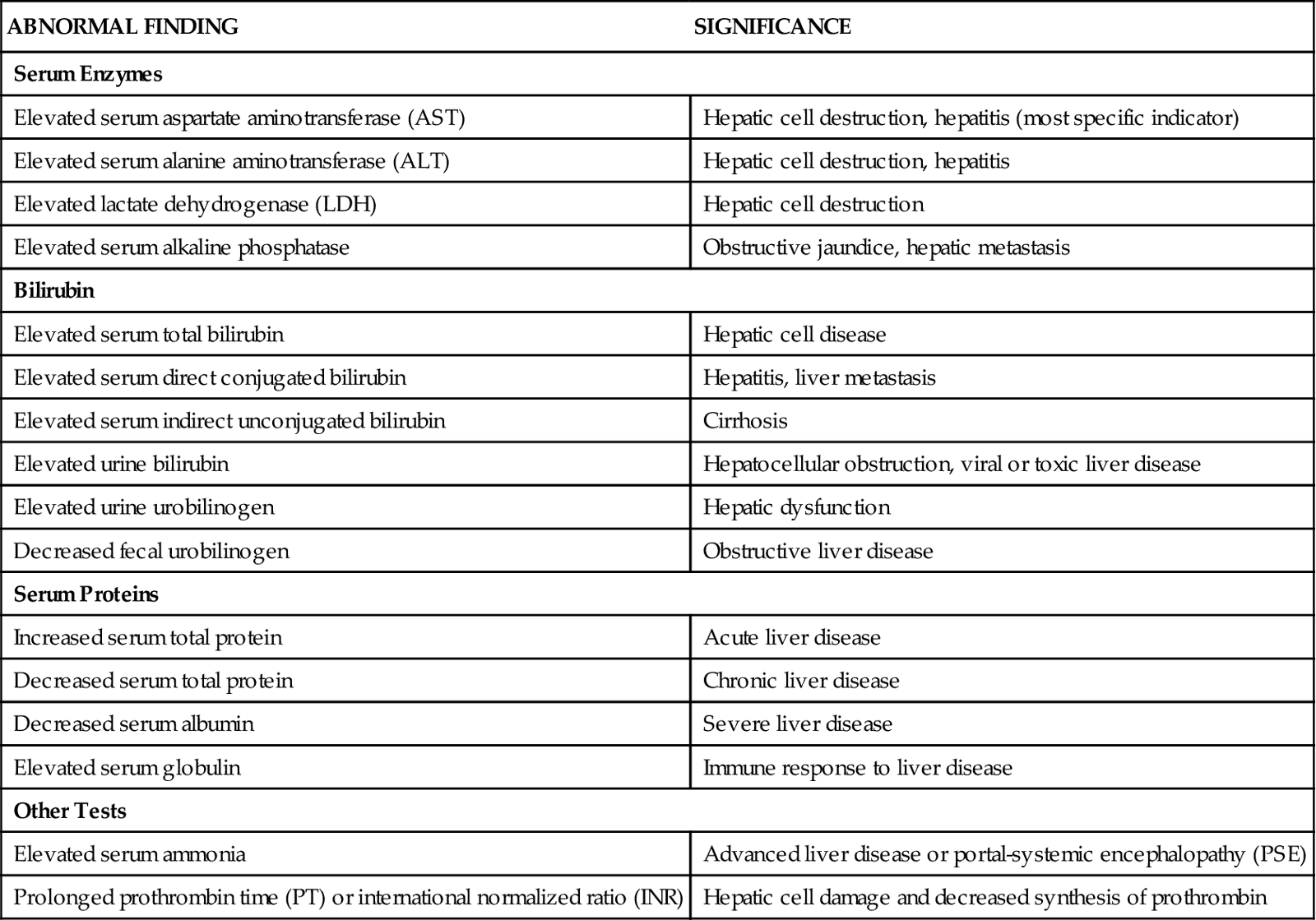
Increased alkaline phosphatase and gamma-glutamyl transpeptidase (GGT) levels are caused by biliary obstruction and therefore may increase in patients with cirrhosis (Kelso, 2008). However, alkaline phosphatase also increases when bone disease, such as osteoporosis, is present. Total serum bilirubin levels also rise. Indirect bilirubin levels increase in patients with cirrhosis because of the inability of the failing liver to excrete bilirubin. Therefore bilirubin is present in the urine (urobilinogen) in increased amounts. Fecal urobilinogen concentration is decreased in patients with biliary tract obstruction. These patients have light- or clay-colored stools.
Total serum protein and albumin levels are decreased in patients with severe or chronic liver disease as a result of decreased synthesis by the liver (Pagana & Pagana, 2010). Loss of osmotic “pull” proteins like albumin promotes the movement of intravascular fluid into the interstitial tissues (e.g., ascites). Prothrombin time/international normalized ratio (PT/INR) is prolonged because the liver decreases the production of prothrombin. The platelet count is low, resulting in a characteristic thrombocytopenia of cirrhosis. Anemia may be reflected by decreased red blood cell (RBC), hemoglobin, and hematocrit values. The white blood cell (WBC) count may also be decreased. Ammonia levels are usually elevated in patients with advanced liver disease. Serum creatinine may be elevated in patients with deteriorating kidney function. Dilutional hyponatremia (low serum sodium) may occur in patients with ascites.
Patients with primary biliary cirrhosis, an autoimmune disease, usually have high disease-specific AMA and anti-nuclear antibody (ANA) titers and elevated levels of immunoglobulin M (IgM) (Lindor et al., 2009).
Imaging Assessment
Plain x-rays of the abdomen may show hepatomegaly, splenomegaly, or massive ascites. A computed tomography (CT) scan may be requested.
Magnetic resonance imaging (MRI) is another test used to diagnose the patient with liver disease. It can reveal mass lesions, giving additional specific information. This information is helpful in determining whether the condition is malignant or benign.
Other Diagnostic Assessment
Ultrasound (US) of the liver is often the first assessment for a person with suspected liver disease to detect ascites, hepatomegaly, and splenomegaly. It can also determine the presence of biliary stones or biliary duct obstruction. Liver US is useful in detecting portal vein thrombosis and evaluating whether the direction of portal blood flow is normal.
Some patients being assessed for liver disease require biopsies to determine the exact pathology and the extent of disease progression. This procedure can be problematic because a large number of patients are at risk for bleeding. Even a percutaneous (through the skin) biopsy can pose a significant risk to the patient. To minimize this risk, an interventional radiologist can perform a liver biopsy using a long sheath through a jugular vein that then is threaded into the hepatic vein and liver. A tissue sample is obtained for microscopic evaluation. If a biopsy procedure is not possible, a radioisotope liver scan may be used to identify cirrhosis or other diffuse disease.
The physician may request arteriography if US is not conclusive in finding portal vein thrombosis. To evaluate the portal vein and its branches, a portal venogram may be performed instead, by passing a catheter into the liver and into the portal vein. This procedure is described on p. 1302 in the Transjugular Intrahepatic Portal-Systemic Shunt section.
The physician may perform an esophagogastroduodenoscopy (EGD) to directly visualize the upper GI tract and to detect the presence of bleeding or oozing esophageal varices, stomach irritation and ulceration, or duodenal ulceration and bleeding. EGD is performed by introducing a flexible fiberoptic endoscope into the mouth, esophagus, and stomach while the patient is under moderate sedation. A camera attached to the scope permits direct visualization of the mucosal lining of the upper GI tract. An endoscopic retrograde cholangiopancreatography (ERCP) uses the endoscope to inject contrast material via the sphincter of Oddi to view the biliary tract and allow for stone removals, sphincterotomies, biopsies, and stent placements if required. These procedures are described in more detail in Chapter 55.
Analysis
The priority problems for patients with cirrhosis include:
Planning and Implementation
Managing Fluid Volume
Planning: Expected Outcomes.
The patient with cirrhosis is expected to have less excess fluid volume as evidenced by decreased ascites and peripheral edema and adequate circulatory volume. If ascites continues, the patient will not have respiratory distress and will manage ascites by adhering to the collaborative plan of care (see the Concept Map for liver failure due to cirrhosis on p. 1301).
Interventions.
Fluid accumulations are minimal during the early stages of ascites. Therefore interventions are aimed at preventing the accumulation of additional fluid and moving the existing fluid collection. Nonsurgical treatment measures are used to treat ascites in most cases.
Supportive measures to control abdominal ascites include nutrition therapy, drug therapy, paracentesis, and respiratory support. The patient’s fluid and electrolyte status is also carefully monitored. If the patient is jaundiced, he or she will likely scratch the skin because the excess bilirubin products cause irritation and pruritus (itching).
Nutrition Therapy.
The health care provider usually places the patient with abdominal ascites on a low-sodium diet as an initial means of controlling fluid accumulation in the abdominal cavity. The amount of daily sodium (Na+) intake restriction varies, but a 1- to 2-gram (2000 mg) Na+ restriction may be tried first. In collaboration with the dietitian, explain the purpose of the restriction and advise the patient and family to read the sodium content labels on all food and beverages. Table salt should be completely excluded. Low-sodium diets may be distasteful, so suggest alternative flavoring additives such as lemon, vinegar, parsley, oregano, and pepper. Remind the patient that seasoned and salty food is an acquired taste; in time, he or she will become used to the decrease in dietary sodium.
In general, patients with late-stage cirrhosis are malnourished and have multiple dietary deficiencies. Vitamin supplements such as thiamine (due to alcohol withdrawal), folate, and multivitamin preparations are typically added to the IV fluids because the liver cannot store vitamins. For patients with biliary cirrhosis, bile may not be available for fat-soluble vitamin transport and absorption. Oral vitamins are prescribed when IV fluid administration is discontinued.
Drug Therapy.
The health care provider usually prescribes a diuretic to reduce fluid accumulation and to prevent cardiac and respiratory problems. Monitor the effect of diuretic therapy by weighing the patient daily, measuring daily intake and output, measuring abdominal girth, documenting peripheral edema, and assessing electrolyte levels. Serious electrolyte imbalances, such as hypokalemia (decreased potassium) and hyponatremia (decreased sodium), may occur with loop diuretic therapy. Depending on the diuretic selected, the provider may prescribe an oral or IV potassium supplement. Some clinicians prescribe a combination of furosemide (Lasix) and spironolactone (Aldactone) as a combination diuretic therapy for the treatment of ascites. Because these drugs work differently, they are used for maintenance of sodium and potassium balance. For example, furosemide causes potassium loss, whereas spironolactone conserves it in the body.
All patients with ascites have the potential to develop spontaneous bacterial peritonitis (SBP) from bacteria in the collected ascitic fluid. In some patients, mild symptoms such as low-grade fever and loss of appetite occur. In others, there may be abdominal pain, fever, and change in mental status. When performing an abdominal assessment, listen for bowel sounds and assess for abdominal wall rigidity. Send a sample of ascitic fluid for a culture before drug therapy begins. Quinolones such as norfloxacin (Noroxin) are the drugs of choice for SBP. If the patient is allergic to this class of antibiotics, combination antibiotics like trimethoprim-sulfamethoxazole (Bactrim) are given.
Paracentesis.
For some patients, abdominal paracentesis may be needed. Nursing implications associated with this procedure are described in Chart 61-1. The procedure is performed at the bedside, in an interventional radiology department, or in an ambulatory care setting. The physician inserts a trocar catheter or drain into the abdomen to remove the ascitic fluid from the peritoneal cavity. This procedure is done using ultrasound for added safety. In some situations, a short-term ascites drain catheter may be placed while the patient is awaiting surgical intervention, or new tunneled ascites drains (e.g., PleurX drains) can allow a patient or family caregiver to drain ascites at home.