Chapter 22 Care of Patients with Immune Function Excess
Hypersensitivity (Allergy) and Autoimmunity
Safe and Effective Care Environment
1. Verify that known hypersensitivities of each patient are documented in the medical record and communicated to all members of the health care team.
2. Coordinate with other members of the health care team to ensure a safe environment for the patient with a latex allergy.
Health Promotion and Maintenance
4. Encourage all patients with a severe allergy or history of anaphylaxis to wear a medical alert bracelet or other identification.
5. Teach patients with allergies how to avoid known allergens and, if needed, how to self-inject epinephrine.
6. Describe allergy testing techniques.
7. Compare the characteristics and manifestations of type I, type II, type III, type IV, and type V hypersensitivity reactions.
8. Prioritize care for the patient experiencing anaphylaxis.
9. Explain the rationale for types of drug therapy for autoimmune disorders.
10. Identify the manifestations of hypersensitivity reactions.
11. Prioritize care for the patient experiencing anaphylaxis.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Clip: High- and Low-Pitched Crackles
Audio Clip: High- and Low-Pitched Wheezes
Review Questions for the NCLEX® Examination
Most of the time, the inflammatory and immune responses are helpful for protection against infection and cancer development. However, when inflammation or immune responses are prolonged or excessive or occur at an inappropriate time, normal tissues are damaged. These responses are “overreactions” to invaders and foreign antigens and are known as hypersensitivity or allergic responses. When these responses fail to recognize and protect self cells, normal body tissues are attacked and harmed. This type of reaction is known as an autoimmune response. Hypersensitivity and autoimmune responses can severely damage cells, tissues, and organs (Abbas et al., 2010).
Hypersensitivities/Allergies
Hypersensitivity or allergy is an increased or excessive response to the presence of an antigen (foreign protein or allergen) to which the patient usually has been previously exposed. These responses cause problems that range from uncomfortable (e.g., itchy, watery eyes or sneezing) to life threatening (e.g., allergic asthma, anaphylaxis, bronchoconstriction, or circulatory collapse). The terms hypersensitivity and allergy are used interchangeably. Hypersensitivity reactions are classified into five basic types, determined by differences in timing, pathophysiology, and clinical manifestations (Table 22-1). Each type may occur alone or along with one or more other types (McCance et al., 2010).
TABLE 22-1 MECHANISMS AND EXAMPLES OF TYPES OF HYPERSENSITIVITIES
| MECHANISM | CLINICAL EXAMPLES |
|---|---|
| Type I: Immediate | |
| Reaction of IgE antibody on mast cells with antigen, which results in release of mediators, especially histamine | |
| Type II: Cytotoxic | |
| Reaction of IgG with host cell membrane or antigen adsorbed by host cell membrane | |
| Type III: Immune Complex–Mediated | |
| Formation of immune complex of antigen and antibody, which deposits in walls of blood vessels and results in complement release and inflammation | |
| Type IV: Delayed | |
| Reaction of sensitized T-cells with antigen and release of lymphokines, which activates macrophages and induces inflammation | |
| Type V: Stimulated | |
| Reaction of autoantibodies with normal cell-surface receptors, which stimulates a continual overreaction of the target cell | |
IgE, Immunoglobulin E; IgG, immunoglobulin G; TB, tuberculosis.
Type I: Rapid Hypersensitivity Reactions
Type I, or rapid, hypersensitivity, also called atopic allergy, is the most common type of hypersensitivity. This type results from the increased production of the immunoglobulin E (IgE) antibody class. Acute inflammation occurs when IgE responds to an antigen, such as pollen, and causes the release of histamine and other vasoactive amines from basophils, eosinophils, and mast cells. Examples of type I reactions include anaphylaxis and allergic asthma (discussed in Chapter 32); atopic allergies such as hay fever and allergic rhinitis; and allergies to specific allergens such as latex, bee venom, peanuts, iodine, shellfish, drugs, and thousands of other environmental antigens. Allergens can be contacted in these ways:
• Inhaled (plant pollens, fungal spores, animal dander, house dust, grass, ragweed)
• Ingested (foods, food additives, drugs)
• Injected (bee venom, drugs, biologic substances such as contrast dyes)
Some reactions occur just in the areas exposed to the antigen, such as the mucous membranes of the nose and eyes, causing symptoms of rhinorrhea, sneezing, and itchy, red, watery eyes. Other reactions may involve all blood vessels and bronchiolar smooth muscle causing widespread blood vessel dilation, decreased cardiac output, and bronchoconstriction. This condition is known as anaphylaxis. When symptoms of anaphylaxis occur in a patient who has not been previously exposed to the allergen, the condition is known as an anaphylactoid reaction (Watson, 2010).
Allergic Rhinitis
Pathophysiology
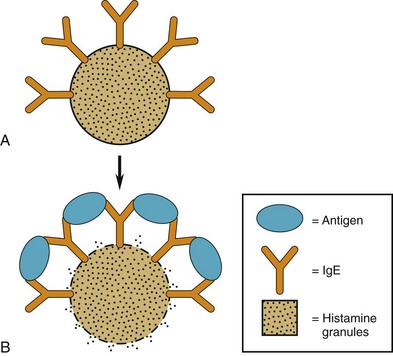
On first exposure to an allergen (an antigen that provokes allergic sensitization), the person responds by making antigen-specific IgE. This antigen-specific IgE binds to the surface of basophils and mast cells (see Fig. 19-9 on p. 311 in Chapter 19). These cells have many granules containing vasoactive amines (including histamine) that are released when stimulated. Once the antigen-specific IgE is formed, the person is sensitized to that allergen.
In a type I allergic reaction, the already sensitized person is re-exposed to the provoking allergen. The resulting response has a primary phase and a secondary phase. In the primary phase, the allergen binds to two adjacent IgE molecules on the surface of a basophil or mast cell, which breaks or distorts the cell membrane. These changes cause the cell membrane to open and release the vasoactive amines within the granules into the tissue fluids (Fig. 22-1).
The secondary phase results from the release of other proteins. These other proteins draw more white blood cells to the area and stimulate a more general inflammatory reaction through actions of leukotriene and prostaglandins (other mediators of inflammation; see Chapter 19). This reaction occurs in addition to the allergic reaction stimulated in the primary phase. The resulting inflammation increases the clinical manifestations and is probably responsible for continuing the response.
The tendency to produce IgE in response to antigen exposure is based on genetic inheritance, but no single gene has been found to be responsible. Although allergic tendencies are inherited, specific allergies are not inherited (Nussbaum et al., 2007). For example, a mother who has an allergy to penicillin but not to peanuts may have a child with an allergy to peanuts but not to penicillin. About 50% of patients with allergic rhinitis have one parent with type I allergies. Atopic allergies, including allergic rhinitis, affect about 10% of the population in North America (McCance et al., 2010).
Patient-Centered Collaborative Care
Assessment
Allergy Testing
Follow-up Care
Repeat open application testing (ROAT) is a form of self-administered patch testing that can help determine which hygiene or beauty products are responsible for a person’s contact dermatitis (Gelpi & Jacob, 2008). (Hygiene, laundry, and beauty products are the most frequent causes of contact dermatitis.) Often, just one application of a suspected allergen does not produce a positive result. With ROAT, the person showers and then draws a 3-cm circle on the inner aspect of the upper arm. The person then selects one product as a suspected allergen and applies it to the circled area. The product is applied to the area twice daily for 7 days. The patient is instructed to protect the area from sunlight and to check it daily for a reaction. A positive reaction may include the presence of increased redness, small bumps, water blisters, or skin scaling. Once a product is identified as an allergen, the patient avoids using it.
Physiological Integrity
Drug Therapy
Drug Alert
Leukotriene modifiers may be used to treat allergic rhinitis. Zileuton (Zyflo) prevents leukotriene synthesis. (See Chapter 19 for a discussion of the role of leukotriene in inflammatory and allergic responses.) Zafirlukast (Accolate) blocks the leukotriene receptor. Both are oral agents and work best in the prevention of allergic rhinitis.
Desensitization Therapy
Desensitization appears to reduce allergic responses by competition. In theory, the very small amounts of allergen first injected are too low to bind to the IgE already present but are enough to induce immunoglobulin G (IgG) production against that allergen. Because IgG is not associated with either mast cells or basal cells, allergens that bind to IgG do not trigger allergic responses. IgG removes the allergen from the body by precipitation (see Chapter 19). By gradually increasing the allergen injection, large amounts of IgG are produced against the allergen. When the patient is then exposed to the allergen in the environment, the IgG binds to it and clears it from the body before IgE can bind to it and trigger an allergic reaction. Because so much more IgG can be produced compared with IgE, IgG is successful in the competition to bind the allergen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree