M. Linda Workman
Care of Patients with Eye and Vision Problems
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
12 Explain the consequences of increased intraocular pressure (IOP).
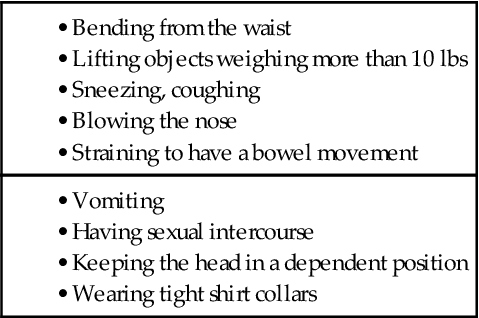
13 Identify common actions, conditions, and positions that increase IOP.
14 Prioritize educational needs for the patient after cataract surgery with lens replacement.
15 Prioritize educational needs for patients with primary open-angle glaucoma.
16 Describe the mechanisms of action and nursing implications of drug therapy for glaucoma.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Concept Map: Glaucoma
Key Points
Review Questions for the NCLEX® Examination
Vision is affected by many factors and problems. Some problems occur gradually, such as cataracts, and others can result from an acute insult or illness. Even when reduced vision is temporary, the patient must make some changes in function or lifestyle.
Eyelid Disorders
The eyelid is composed of thin skin attached to small muscles. It protects the eye surface and spreads tears. Problems can occur with changes in the structure, function, or position of the eyelid. Lid structure may also be altered by age.
Blepharitis
Blepharitis, an inflammation of the eyelid edges, occurs most often in the older adult and those with dry eye syndrome (see the Keratoconjunctivitis Sicca section, p. 1056). Reduced tear production often leads to bacterial infection of the eye, because tears inhibit bacterial growth.
Patients usually have itchy, red, and burning eyes. Seborrhea (greasy, itchy scaling) of the eyebrows and eyelids is often present. Greasy scales and mattering may be seen where the eyelashes exit the eyelid.
Blepharitis is controlled with eyelid care using warm, moist compresses followed by gentle scrubbing with dilute baby shampoo. Instruct the patient to avoid rubbing the eyes, because if infection is present, this action can spread the infection to other eye structures.
Entropion and Ectropion
An entropion is the turning inward of the eyelid causing the lashes to rub against the eye. Entropion can be caused by eyelid muscle spasms or by scarring and deformity of the eyelid after trauma. It occurs often among older adults because of age-related loss of tissue support.
The patient usually reports “feeling something in my eye.” Pain and tears may also be present. The eyelid is turned inward, and the conjunctiva is red. Corneal abrasion may result from constant irritation.
Surgery corrects eyelid position by either tightening the orbicular muscles and moving the eyelid to a normal position or by preventing inward rotation of the eyelid. After surgery, the eye is covered with a patch and the patient is discharged a few hours later.
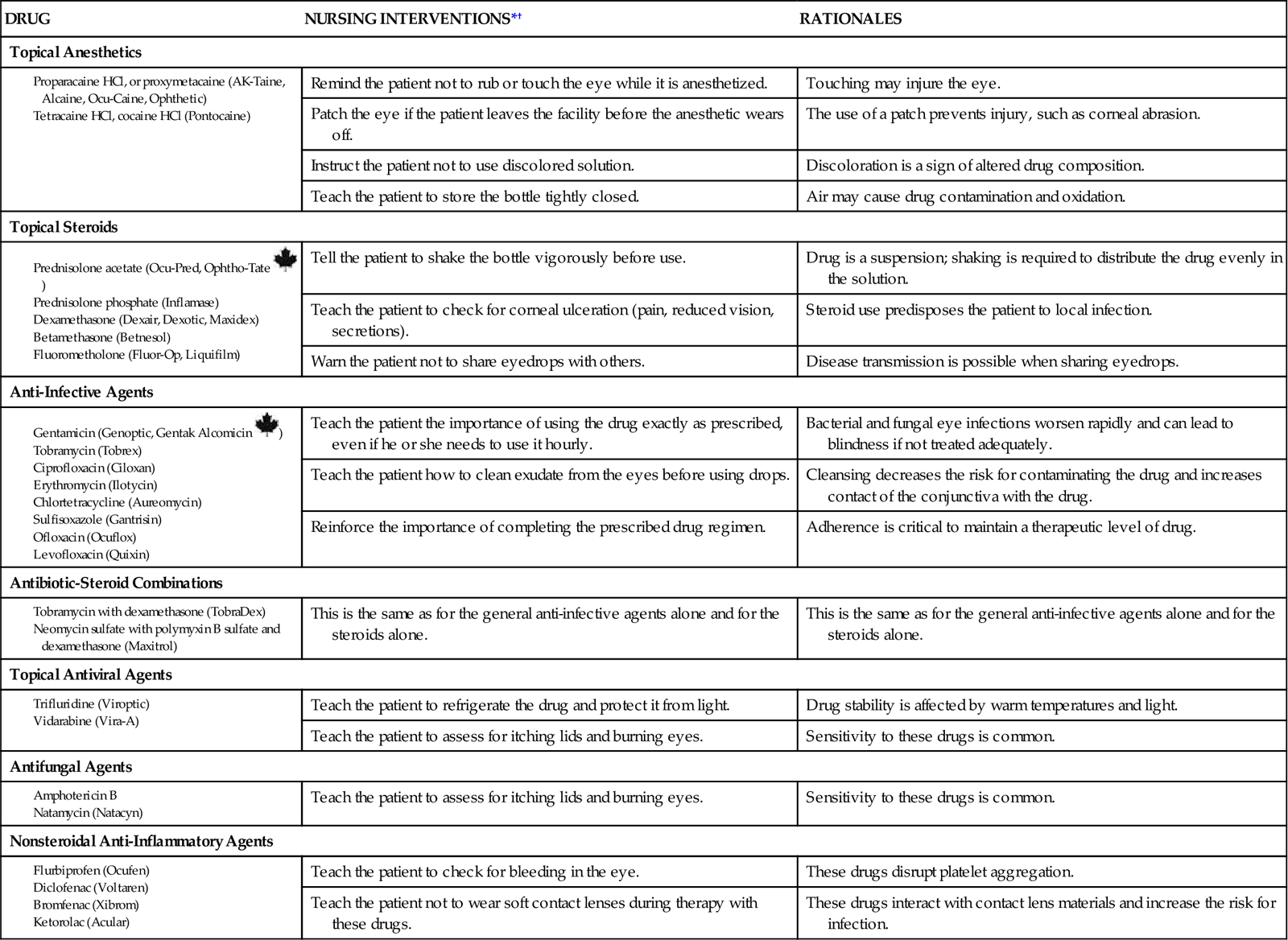
Demonstrate instillation of eyedrops, and evaluate the patient’s ability to instill the drops. Instruct the patient to leave the patch in place until he or she is seen by the ophthalmologist and to report any pain or drainage under the patch. Teach the patient or family member how to clean the suture line with a cotton swab and the prescribed solution. A small amount of antibiotic ointment may be applied (Fig. 49-1). Chart 49-1 describes how to apply ophthalmic ointment. Chart 49-2 lists information on common ophthalmic drugs for eye inflammation and infection.

An ectropion is the turning outward and sagging of the eyelid, which often occurs with aging, caused by muscle relaxation or weakness. This lid position reduces the washing action of tears, leading to corneal drying and ulceration.
Patients often have constant tears and a sagging lower eyelid. Surgery can restore lid alignment. After surgery, the eye is covered with a patch and the patient is discharged. Nursing care is the same as for an entropion.
Hordeolum
A hordeolum, or stye, is an infection of the sweat glands in the eyelid (external hordeolum) or of the eyelid sebaceous gland (internal hordeolum). A red, swollen, tender area occurs on the skin surface side of the eyelid. The most common causative organisms are Staphylococcus aureus, Staphylococcus epidermidis, and Streptococcus. The hordeolum usually affects only one eyelid at a time. Vision is not affected.
Small, beady, swollen areas may be on the skin side of the eyelid or on the conjunctival side of the eyelid. Pain occurs as the hordeolum fills with purulent material.
Management includes applying warm compresses four times a day and an antibacterial ointment. When the lesion opens, the pus drains and the pain subsides.
Nursing interventions include instructing the patient how to apply compresses. Chart 49-3 describes the proper technique for application of an eye compress.
After compresses have been applied, instill antibiotic ointment. Advise the patient that ointments may cause blurred vision, and teach him or her to remove the ointment from the eyes before driving or operating machinery. To remove the ointment, teach the patient to close the eye and then gently wipe the closed eyelid from the nasal side of the eye outward.
Chalazion
A chalazion is an inflammation of a sebaceous gland in the eyelid. It begins with redness and tenderness, followed by a gradual painless swelling. Later, redness and tenderness are not present. Most chalazia protrude on the inside of the eyelid. The patient has eye fatigue, light sensitivity, and excessive tears.
Management includes applying warm compresses four times a day, followed by instillation of ophthalmic ointment. If the chalazion is large enough to affect vision or is cosmetically displeasing, it may be removed surgically.
After surgery, antibiotic ointment is instilled and the eye is covered with a patch. Best practices for application of a nonpressure eye patch are described in Chart 49-4.
Instruct the patient to leave the eye patch in place for about 6 hours and then remove the patch and apply warm, wet compresses. Antibiotic eyedrops are instilled after use of the compresses. Teach him or her to immediately report increasing redness, purulent drainage, or reduced vision to the ophthalmologist.
Keratoconjunctivitis Sicca
Pathophysiology
The lacrimal system moistens the eye surface with tears and removes tears from the eye. Problems arise from reduced tear production, infection, or inflammation in the lacrimal system.
Keratoconjunctivitis sicca, or dry eye syndrome, results from changes in tear production, tear composition, or tear distribution. Drugs (e.g., antihistamines, beta-adrenergic blocking agents, anticholinergic drugs) also can reduce tear production. Diseases associated with decreased tear production include rheumatoid arthritis, leukemia, sarcoidosis, and Sjögren’s syndrome. Radiation or chemical burns to the eye also decrease tear production. Injury to cranial nerve VII inhibits tears. Eye dryness may follow vision-enhancing surgery. Dry eye syndromes are much more common in women than in men (Pullen & Hall, 2010).
Patient-Centered Collaborative Care
The patient has a foreign body sensation in the eye, burning and itching eyes, and photophobia (sensitivity to light). The corneal light reflex is dulled. Tears contain mucus strands.
Management depends on symptom severity. Cyclosporine (Restasis) eyedrops may be prescribed to increase tear production. Artificial tears (HypoTears, Refresh) also can be used to reduce daytime dryness. A lubricating ointment (Lacri-Lube SOP, Refresh P.M.) is used at night. If the dry eye syndrome is caused by an abnormal eyelid position, surgery may be needed.
Conjunctival Disorders
The conjunctiva is a thin mucous membrane that covers and protects the eye. Because of its location, the conjunctiva is subject to trauma and infection.
Hemorrhage
Conjunctival blood vessels are fragile and can break with increased pressure during sneezing, coughing, or vomiting. Hemorrhages may also occur with hypertension, trauma, or blood clotting problems.
The small, well-defined area of hemorrhage is bright red under the conjunctiva. The patient is usually concerned about its appearance although no pain or visual impairment occurs with the hemorrhage. It resolves within 14 days without treatment.
Conjunctivitis
Conjunctivitis is an inflammation or infection of the conjunctiva. Inflammation occurs from exposure to allergens or irritants. Infectious conjunctivitis occurs with bacterial or viral infection and is readily transmitted from person to person (Saligan & Yeh, 2008).
Allergic conjunctivitis manifestations are edema, a sensation of burning, a “bloodshot” eye appearance, excessive tears, and itching. Management includes vasoconstrictor and corticosteroid eyedrops (see Chart 49-2). Teach women to avoid using makeup near the eye until all symptoms have subsided.
Bacterial conjunctivitis, or “pink eye,” is usually caused by Staphylococcus aureus or Haemophilus influenzae. Manifestations are blood vessel dilation, mild edema, tears, and discharge. The discharge is watery at first and then becomes thicker, with shreds of mucus.
Cultures of the drainage are obtained to identify the organism. Drug therapy with topical antibiotics is prescribed to eliminate the infection. Nursing interventions focus on preventing infection spread to the other eye or to other people. Document the amount, color, and type of drainage. Remind the patient to wash his or her hands after touching the eye and before using eyedrops. Warn him or her not to touch the unaffected eye without first washing the hands and to avoid sharing washcloths and towels with others. Instruct women to discard eye makeup and applicators used at the time the infection developed to avoid the possibility of recontamination.
Trachoma
Trachoma is a chronic conjunctivitis caused by Chlamydia trachomatis. It scars the conjunctiva and is a common cause of preventable blindness worldwide. The incidence is highest in warm, moist climates where sanitation is poor.
The incubation period is 5 to 14 days, and at first the disease resembles bacterial conjunctivitis. Manifestations include tears, photophobia, and eyelid edema. Follicles form on the upper eyelid conjunctiva. As the disease progresses, the eyelid scars and turns inward, causing the eyelashes to damage the cornea.
Cultures are used to identify the causative organism. A 4-week course of oral or topical tetracycline (Achromycin, Apo-Tetra ![]() ) or erythromycin (Apo-Erythro-EC
) or erythromycin (Apo-Erythro-EC ![]() , E-Mycin, E.E.S.) is given. Azithromycin (Zithromax) can be used once per week for 1 to 3 weeks.
, E-Mycin, E.E.S.) is given. Azithromycin (Zithromax) can be used once per week for 1 to 3 weeks.
Nursing interventions focus on infection control. Teach the patient to wash the hands before and after touching the eyes. Teach him or her to keep washcloths separate from those of unaffected people and to launder them separately.
Corneal Disorders
For a sharp image to be focused on the retina, the cornea must be transparent and intact. Corneal problems may be caused by irritation or infection (keratitis) with ulceration of the corneal surface, degeneration of the cornea (keratoconus), or deposits in the cornea. All corneal problems reduce the refracting power of the cornea, and some can lead to blindness.
Corneal Abrasion, Ulceration, and Infection
Pathophysiology
A corneal abrasion is a scrape or scratch of the cornea that disrupts its integrity. This painful condition can be caused by a small foreign body, trauma, or, most commonly, contact lens use. Other conditions that promote loss of corneal integrity include malnutrition, dry eye syndromes, and some cancer therapies. The abrasion allows organisms to enter, leading to corneal infection. Bacterial, protozoal, and fungal infections can lead to corneal ulceration, which is a deeper disruption of the epithelium. This problem is an emergency because the cornea has no separate blood supply and infections that can permanently impair vision develop rapidly. Use of homemade contact lens solutions and the use of large-volume solution containers that can easily become contaminated have led to a sharp rise in the incidence of corneal ulcers infected with Pseudomonas aeruginosa and fungi.
Patient-Centered Collaborative Care
The patient with a corneal disorder has pain, reduced vision, photophobia, and eye secretions. Cloudy or purulent fluid may be present on the eyelids or lashes. Wear gloves when examining the eye.
The entire cornea may look hazy or cloudy with a patchy area of ulceration. When fluorescein stain is used, the patchy areas appear green. Microbial culture and corneal scrapings can help determine the causative organism. Anti-infective therapy is started before the organism is identified because of the high risk for vision loss. For culture, obtain swabs from the ulcer and its edges. For corneal scrapings, the cornea is anesthetized with a topical agent and a physician or advanced practice nurse remove samples from the center and edge of the ulcer.
Antibiotics, antifungals, and antivirals are prescribed to reduce or eliminate the organisms. Usually, a broad-spectrum antibiotic is prescribed first and may be changed when culture results are known. Steroids may be used with antibiotics to reduce the inflammatory response in the eye. Drugs can be given topically as eyedrops, injected subconjunctivally, or injected IV. Chart 48-4 in Chapter 48 lists best practices for instilling eyedrops. The nursing priorities are to begin the drug therapy, to ensure patient understanding of the drug therapy regimen, and to prevent infection spread.
Often, the anti-infective therapy involves instilling eyedrops every hour for the first 24 hours. Teach the patient how to apply the eyedrops correctly. (See Chart 48-2 in Chapter 48.) Use sterile saline eyedrops to demonstrate the technique, and obtain a return demonstration. If the patient cannot safely self-apply the drugs, teach a family member how to do it.
If the eye infection occurs from a corneal abrasion or ulcer, only one eye is affected. Teach the patient not to use the drug in the unaffected eye. In addition, teach him or her to wash hands after touching the affected eye and before touching or doing anything to the healthy eye. If both eyes are infected, separate bottles of drugs are needed for each eye. Teach the patient to clearly label the bottles “right eye” and “left eye” and not to switch the drugs from eye to eye. Also teach him or her to completely care for one eye, then wash the hands, and using the drugs for the remaining eye, care for that eye. Teach the patient not to wear contact lenses during the entire time that these drugs are being used because the eye then has fewer protections against infection or injury. In addition, the drugs can cloud or damage the contact lenses.
Stress the importance of applying the drug as often as prescribed, even at night. Stopping the infection at this stage can save the vision in the infected eye. Also instruct the patient to make and keep all follow-up appointments; usually the patient is seen again in 24 hours or less.
The type of anti-infective used and the frequency of application may change when the organism is identified and the infection is responding to the therapy. Drug therapy may continue for 3 or more weeks to ensure eradication of the infection. Warn women to avoid using makeup around the eye until the infection has cleared to prevent spread of infection. Instruct patients to discard all open containers of contact lens solutions and bottles of eyedrops because these may be contaminated. Patients should not wear contact lenses for weeks to months until the infection is gone and the ulcer is healed.
Keratoconus and Corneal Opacities
Pathophysiology
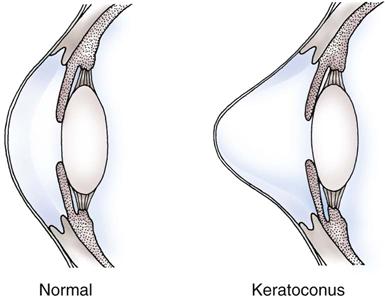
The cornea can permanently lose it shape, become scarred or cloudy, or become thinner. When these conditions occur, refraction is reduced and images are not focused sufficiently for useful vision. Keratoconus, the degeneration of the corneal tissue resulting in abnormal corneal shape, can occur with trauma or may be an inherited disorder (Fig. 49-2). Inadequately treated corneal infections and severe trauma can damage and scar the cornea and lead to severe visual impairment that can be improved only by surgical interventions.
Patient-Centered Collaborative Care
For a misshaped cornea that is still clear, surgical management involves a corneal implant that adjusts the shape of the cornea. The device approved for this procedure is the Intacs corneal ring. With this procedure, the shape of the cornea is changed by placing a flexible ring in the outer edges of the cornea (outside of the optical zone).
The procedure is performed on both eyes during one surgery under local anesthesia. Improvement to best vision is immediate. Overcorrection or undercorrection of refraction is possible. However, removal, replacement, or adjustment of ring tightness can enhance satisfaction. In addition, replacements can be made if the patient’s vision changes further as a result of aging. Because the ring is applied to the cornea outside of the optical zone, the risk for corneal clouding or scarring is lower than with other surgical eye procedures.
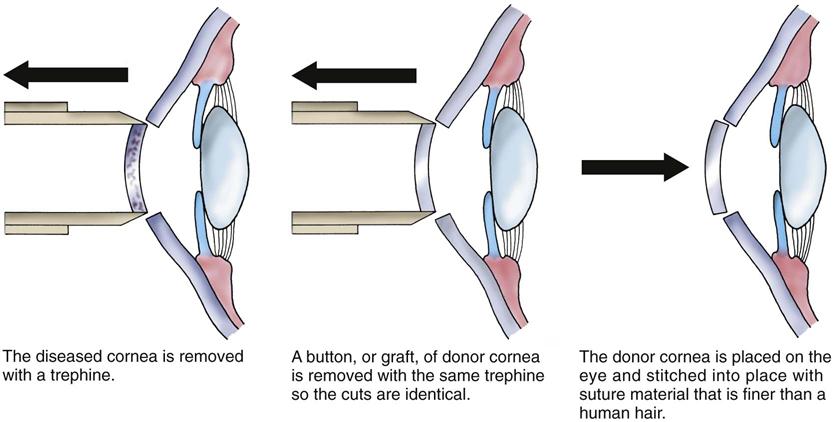
Surgery to improve clarity for a permanent corneal disorder that obscures vision is a keratoplasty (corneal transplant), in which the diseased corneal tissue is removed and replaced with tissue from a human donor cornea. This process improves vision by removing corneal deformities and replacing them with healthy corneal tissue.
Preoperative care may be short, with little time for teaching because transplantation is performed when the donor cornea becomes available. The patient is usually anxious. Use a calm approach to assess his or her knowledge of the surgery and of care before and after surgery.
Examine the eyes for signs of infection, and report any redness, drainage, or edema to the ophthalmologist. Instill prescribed antibiotic eyedrops, and obtain IV access before surgery.
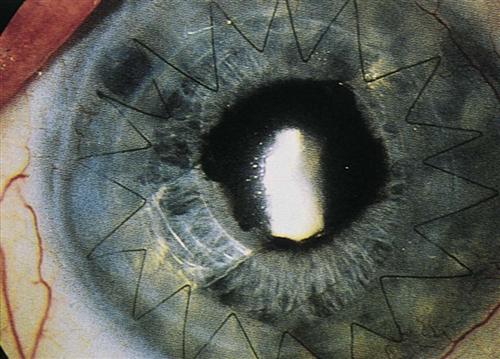
Operative procedures are keratoplasties and are usually performed with local anesthesia in an ambulatory surgical setting. The transplant may involve the entire depth of corneal tissue (penetrating keratoplasty) or only certain layers of the corneal tissue (lamellar keratoplasty). The nerves around and behind the eye are numbed so that the patient cannot move or see out of the eye. The center 7 to 8 mm of the diseased cornea is removed (Fig. 49-3) with an instrument that works like a cookie cutter. The same instrument is used to cut the tissue graft from the donor cornea so that the graft will be a perfect fit. The donor corneal graft is sutured into place on the eye. Fig. 49-4 shows the eye after transplantation. The procedure usually takes about an hour, and the patient is discharged to home 1 to 2 hours after the procedure.
Postoperative care involves extensive patient teaching. After the procedure, an antibiotic is injected under the conjunctiva and an antibiotic ointment instilled. The eye is covered with a pressure patch and a protective shield until the next day, when the patient returns to the surgeon.
Notify the ophthalmologist of changes in vital signs or of drainage on the dressing. Instruct the patient to lie on the nonoperative side to reduce intraocular pressure (IOP).
Show the patient or family member how to apply a patch, and obtain a return demonstration. The patch may need to be worn during the day for the first 3 to 5 days. Teach the patient to wear the shield at night for the first month after surgery and whenever he or she is around small children or pets. Instruct him or her not to use an ice pack on the eye. Complications after surgery include bleeding, wound leakage, infection, and graft rejection. Teach the patient how to instill eyedrops, and obtain a return demonstration. Show pictures of what the eye and sutures should look like. Teach him or her to examine the eye (or have a family member do the examination) daily for the presence of infection or graft rejection. The presence of purulent discharge, a continuous leak of clear fluid from around the graft site (not tears), or excessive bleeding should be reported immediately to the surgeon. Other complications include decreased vision, increased reddening of the eye, pain, increased sensitivity to light, and the presence of light flashes or “floaters” in the field of vision. Teach the patient to report any of these manifestations to the surgeon if they develop after the first 48 hours and persist for more than 6 hours.
The eye should be protected from any activity that can increase the pressure on, around, or inside the eye. Teach the patient to avoid jogging, running, dancing, and any other activity that promotes rapid or jerky head motions for several weeks after surgery. Other activities that may raise intraocular pressure (IOP) and should be avoided are listed in Table 49-1. Returning to work depends on the type of work. Patients who have sedentary jobs, such as secretaries, may return to work in 1 week, whereas those who perform heavy lifting or manual labor may need to be off work for 6 to 8 weeks.
Graft rejection can occur. Inflammation starts in the donor cornea near the graft edge and moves toward the center. Vision is reduced, and the cornea becomes cloudy. Topical corticosteroids and other immunosuppressants are used to stop the rejection process. If rejection continues, the graft becomes opaque and blood vessels branch into the opaque tissue.
Eye donation is a common procedure and needed for corneal transplantation. Corneal tissue is obtained from a local eye or tissue bank. An eye bank obtains its supply of corneal tissue from volunteer donors. These donors must be free of infectious disease or cancer at the time of death. If a deceased patient is a potential eye donor, follow these steps:
• Raise the head of the bed 30 degrees.
• Instill prescribed antibiotic eyedrops, such as Neosporin or tobramycin.
• Close the eyes, and apply a small ice pack to the closed eyes.
Cataract
Pathophysiology
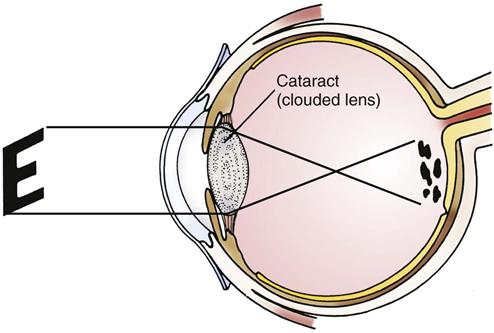
The lens is a transparent, refractive elastic structure suspended behind the iris. A cataract is a lens opacity that distorts the image projected onto the retina (Fig. 49-5). With aging, the lens gradually loses water and increases in density (Touhy & Jett, 2010). This increased density occurs as older lens fibers are compressed and new fibers are produced in the outer layers. Lens proteins dry out and form crystals. As the density of the lens increases, it becomes opaque with a painless loss of transparency. Both eyes may have cataracts; however, the rate of progression in each eye is usually different.
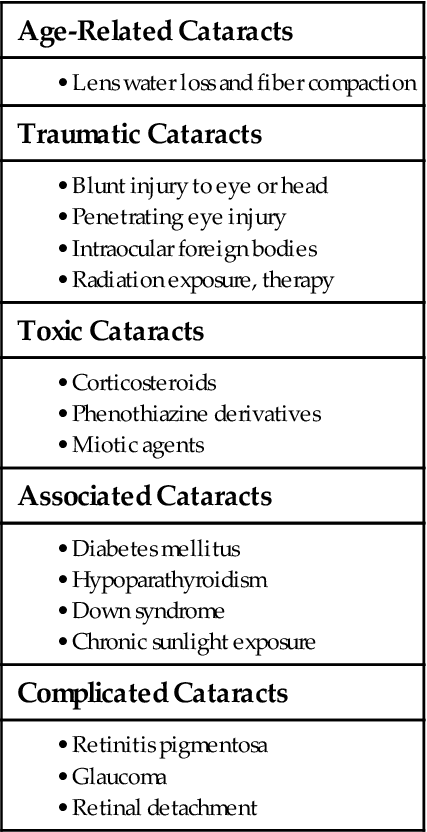
Etiology and Genetic Risk
Cataracts are classified by nature or by onset. They may be present at birth or develop at any time. Cataracts may be age-related or caused by trauma or exposure to toxic agents. They also occur with other diseases and eye disorders (Table 49-2).
Incidence/Prevalence
About 20 to 22 million people in North America have cataracts (National Eye Institute, 2010; Statistics Canada, 2010). The age-related cataract is the most common type. Some degree of cataract formation is expected in all people older than 70 years.
Health Promotion and Maintenance
Although most cases of cataracts in North America are age-related, the onset of cataract formation occurs earlier with heavy sun exposure or exposure to other sources of ultraviolet (UV) light. Teach people to reduce the risk for cataract by wearing sunglasses that limit exposure to UV light whenever they are out in bright sunlight. Cataracts also may result from direct eye injury. Urge all people to wear eye and head protection during sports, such as baseball, or any activity that increases the risk for the eye being hit by objects in motion.
Patient-Centered Collaborative Care
Assessment
History
Age is important because cataracts are most prevalent in the older adult. Ask about these predisposing factors:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 – to
– to  -inch thin strip of ointment into the pocket you have made with the patient’s lower lid. Start at the nose side of the pocket, and move toward the outer edge of the pocket.
-inch thin strip of ointment into the pocket you have made with the patient’s lower lid. Start at the nose side of the pocket, and move toward the outer edge of the pocket.