Judith Laver Bierschbach
Care of Patients with Ear and Hearing Problems
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
9 Safely remove impacted cerumen from the ear canal of an older patient.
10 Coordinate the care of the patient with Ménière’s disease.
11 Prioritize nursing care needs for the patient after tympanoplasty.
12 Prioritize educational needs for the patient after stapedectomy.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
The ears are important for hearing and balance. Ear disorders may lead to hearing difficulty, balance problems, and impaired general function. Hearing problems reduce the ability of patients to fully communicate with the world around them. They can lead to confusion, mistrust, social isolation, and the inability to give and receive accurate information. Although ear and hearing disorders are often easily managed, early recognition and intervention are necessary to prevent additional damage and to promote a maximum level of wellness.
Conditions Affecting the External Ear
The external ear is the outermost part of the ear structures and is subject to outside factors that can cause problems. Disorders of the external ear include congenital malformation (birth defects), trauma, and infectious or noninfectious lesions of the pinna, auricle, or auditory canal. The presence of birth defects in one area does not necessarily mean that other areas of the ear also will be affected. Abnormalities of the external ear range from crumpling or falling forward of the pinna to complete absence (atresia) of the auditory canal. Trauma can damage or destroy the auricle and external canal. Surgical reconstruction can re-form the pinna with skin grafts and plastic prostheses. Trauma to the auricle resulting in a hematoma requires the removal of blood via needle aspiration to prevent calcification and hardening, which is often referred to as a cauliflower or boxer’s ear.
Benign cysts or polyps of the auricle or external canal are surgically removed if they block the canal and affect hearing. Cancer cells, usually basal cell carcinoma, can occur on the pinna. Usually, treatment consists of simple excision. When the lesion becomes larger, its location near the skull and facial nerve makes treatment more difficult.
External Otitis
Pathophysiology
External otitis is a painful condition caused when irritating or infective agents come into contact with the skin of the external ear. The result is either an allergic response or inflammation with or without infection. Affected skin becomes red, swollen, and tender to touch or movement. Swelling of the ear canal can lead to temporary hearing loss due to obstruction. Allergic external otitis is often caused by contact with cosmetics, hair sprays, earphones, earrings, or hearing aids. The most common infectious organisms are Pseudomonas aeruginosa, Streptococcus, Staphylococcus, and Aspergillus.
External otitis occurs more often in hot, humid environments, especially in the summer, and is known as swimmer’s ear because it occurs most often in people involved in water sports. Patients who have traumatized their external ear canal with sharp or small objects (e.g., hairpins, cotton-tipped applicators) or with headphones also are more susceptible to external otitis.
Necrotizing or malignant otitis is the most virulent form of external otitis. Organisms spread beyond the external ear canal into the ear and skull. The high mortality rate seen with malignant external otitis results from complications such as meningitis, brain abscess, and destruction of cranial nerve VII.
Patient-Centered Collaborative Care
Manifestations of external otitis range from mild itching to pain with movement of the pinna or tragus, particularly when upward pressure is applied to the external canal. Patients report feeling as if the ear is plugged and hearing is reduced.
Use caution during otoscopic examination to avoid pressing on the walls of the external canal, which causes pain. Drainage from the ear is often greenish white. To prevent cross-contamination, examine the unaffected ear first. Hearing loss in the affected ear can be severe when inflammation obstructs the ear canal and prevents sounds from reaching the eardrum (tympanic membrane).
Management focuses on reducing inflammation, edema, and pain. Nursing priorities include comfort measures, such as applying heat to the ear for 20 minutes three times a day. This can be accomplished by using towels warmed with water and then wrapped in a plastic bag or by using a heating pad placed on a low setting. Teach the patient that minimizing head movements reduces pain.
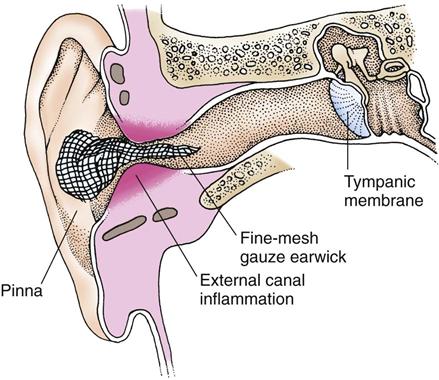
Topical antibiotic and steroid therapies are most effective in decreasing inflammation and pain. Review best practices for instilling eardrops with the patient, as shown in Chart 51-1. Observe the patient self-administer the eardrops to make sure that proper technique is used. If edema obstructs the external canal, an earwick is inserted past the blockage, with drugs applied to the outside end (Fig. 51-1). A long piece of gauze dressing serves as an earwick, which the health care provider inserts using forceps to push carefully through the blocked external auditory canal to the eardrum. The earwick may be removed when eardrops can flow freely into the canal. Use handwashing whenever the infected ear is touched. Oral or IV antibiotics are used in severe cases, especially when infection spreads to surrounding tissue or area lymph nodes are enlarged.
Analgesics, including opioids, may be needed for pain relief during the initial days of treatment. NSAIDs, such as acetylsalicylic acid (aspirin, Entrophen ![]() ) and ibuprofen (Advil), or acetaminophen (Tylenol, Abenol
) and ibuprofen (Advil), or acetaminophen (Tylenol, Abenol ![]() ) may relieve less-severe pain.
) may relieve less-severe pain.
After the inflammation has subsided, a solution of 50% rubbing alcohol, 25% white vinegar, and 25% distilled water may be dropped into the ear to keep it clean and dry and to prevent recurrence. Teach the patient not to use cotton-tipped applicators to dry the ears, because this use could damage the canal and increase the risk for infection or inflammation. Teach him or her to use preventive measures for minimizing ear canal moisture, trauma, or exposure to materials that lead to local irritation or contact dermatitis. Recommend the use of earplugs when engaging in water sports to those patients with recurrent episodes of external otitis.
Furuncle
A furuncle is a localized external otitis caused by bacterial infection, usually Staphylococcus, of a hair follicle. Most furuncles occur on the outer half of the external canal.
The manifestations of a furuncle include intense local pain to light touch. The area is swollen and red, with tight skin covering the area, possibly with a purulent head. No drainage is seen unless the furuncle has ruptured. Hearing is impaired if the lesion blocks the canal.
Treatment consists of local and systemic antibiotics and local heat application. An earwick may be used with one-half strength Burow’s solution to relieve pain. The furuncle may need to be incised and drained if it does not resolve with antibiotic therapy.
Perichondritis
Perichondritis is an infection of the perichondrium, a tough, fibrous tissue layer that surrounds the cartilage and shapes the pinna. This tissue supplies blood to the ear cartilage. Infection can be caused by opening an area of pus or localized infection, insect bites, trauma, postoperative complication of tympanoplasty, and cartilage ear piercing. When infection occurs between the perichondrium and the cartilage, blood flow to the cartilage can be reduced to the point that necrosis occurs and the pinna may become deformed. This can occur as a complication of high helical ear piercing and may require removal of necrotic tissue.
The purposes of management are to eliminate the infection and ensure that the perichondrium stays in direct contact with the cartilage. In addition to systemic antibiotic therapy, a wide incision is made and suction drainage is used to remove pus and other fluid.
Cerumen or Foreign Bodies
Pathophysiology
Cerumen (wax) is the most common cause of an impacted canal. A canal can also become impacted as a result of foreign bodies that can enter or be placed in the external ear canal, such as vegetables, beads, pencil erasers, and insects. Although uncomfortable, cerumen or foreign bodies are rarely true emergencies and can be carefully removed by a health care professional. Cerumen impaction in the older adult is common, and removal of the cerumen from older adults often improves hearing (Holcomb, 2009).
Patient-Centered Collaborative Care
Patients with a cerumen impaction or a foreign body in the ear may experience a sensation of fullness in the ear, with or without hearing loss, and may have ear pain, itching, dizziness, or bleeding from the ear. The object may be visible with direct inspection.
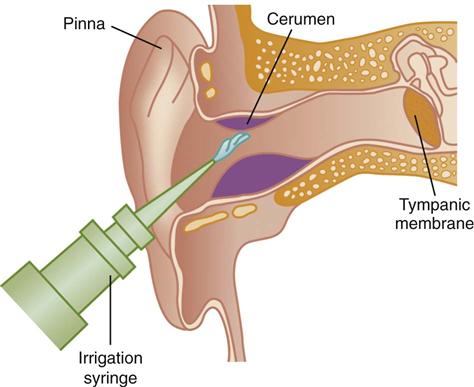
When the occluding material is cerumen, management options include watchful waiting, manual removal, and the use of ceruminolytic agents followed by either manual irrigation or the use of a low-pressure, electronic, oral irrigation device (Holcomb, 2009). The canal can be irrigated with a mixture of water and hydrogen peroxide at body temperature (Fig. 51-2), following best practices for proper irrigation (Chart 51-2). Removal of a cerumen obstruction by irrigation is a slow process and may take more than one sitting. When it is the cause of hearing loss, cerumen removal may improve hearing. Between 50 and 70 mL of solution is the maximum amount that the patient with an impaction usually can tolerate at one sitting.
If the cerumen is thick and dry or cannot be removed easily, suggest an over-the-counter ceruminolytic product such as Cerumenex to soften the wax before trying to remove it. Another way to soften cerumen is to add 3 drops of glycerin or mineral oil to the ear at bedtime and 3 drops of hydrogen peroxide twice a day. After several days of this treatment, the cerumen is more easily removed by irrigation. In some cases, a small curette or cerumen spoon may be used by a health care professional to scoop out the wax. Care is taken with this method because damage to the canal or the eardrum can occur with improper technique.
Discourage the use of cotton swabs and ear candles (hollow tubes coated in wax inserted into the ear and then lighted at the far end) to clean the ears or remove cerumen. Chart 50-3 in Chapter 50 describes steps to teach patients regarding ear hygiene and self–ear irrigation. Refer to Chart 51-3 for nursing care considerations of older adult patients with cerumen impaction.
Insects are killed before removal unless they can be coaxed out by a flashlight or a humming noise. Lidocaine, a numbing agent, can be placed in the ear canal for pain relief. Mineral oil or diluted alcohol instilled into the ear can suffocate the insect, which is then removed with ear forceps.
If the patient has local irritation, an antibiotic or steroid ointment may be applied to prevent infection and reduce local irritation. Hearing acuity is tested if hearing loss is not resolved by removal of the object.
Surgical removal of the foreign object may be required. The object is removed through the ear canal (transcanal route) using a wire bent at a 90-degree angle. The wire is looped around the object, and the object is pulled out. Because this procedure is painful, general anesthesia is needed.
Conditions Affecting the Middle Ear
Otitis Media
Pathophysiology
The three common forms of otitis media are acute otitis media, chronic otitis media, and serous otitis media. Each type affects the middle ear but has different causes and pathologic changes. If otitis progresses or is untreated, permanent conductive hearing loss may occur.
Acute otitis media and chronic otitis media, also known as suppurant or purulent otitis media, are similar. An infecting agent in the middle ear causes inflammation of the mucosa, leading to swelling and irritation of the small bones (ossicles) within the middle ear, followed by purulent inflammatory exudate. Acute disease has a sudden onset and lasts 3 weeks or less. Chronic otitis media often follows repeated acute episodes, has a longer duration, and causes greater middle ear injury. It may be a result of the continuing presence of a biofilm in the middle ear. A biofilm is a community of bacteria working together to overcome host defense mechanisms to continue to survive and proliferate (Lee et al., 2009). (See Chapter 25 for more information about biofilms.) Therapy for complications associated with chronic otitis media, unlike that of acute otitis media, usually involves surgical intervention.
The eustachian tube and mastoid, connected to the middle ear by a sheet of cells, are also affected by the infection. If the eardrum membrane perforates and infective materials spill into the external ear, external otitis develops that thickens and scars the middle ear if left untreated. Necrosis of the ossicles destroys middle ear structures and causes hearing loss.
Patient-Centered Collaborative Care
Assessment
The patient with acute or chronic otitis media has ear pain with and without movement of the external ear. Acute otitis media causes more intense pain. As the pressure in the middle ear increases, there is a sensation of fullness in the ear. Hearing is reduced and distorted. The patient may notice a sticking or cracking sound in the ear upon yawning or swallowing or may have tinnitus in the form of a low hum or a low-pitched sound. Conductive hearing loss may occur as sound wave transmission is obstructed. Headaches and systemic symptoms such as malaise, fever, nausea, and vomiting can occur. As the pressure on the middle ear pushes against the inner ear, the patient may have dizziness or vertigo.
Otoscopic examination findings vary, depending on the stage of the condition. The eardrum is initially retracted, which allows landmarks of the ear to be seen clearly. At this early stage, the patient has only vague ear discomfort. As the condition progresses, the eardrum’s blood vessels dilate and appear red (Fig. 51-3). In the third stage, the eardrum becomes red, thickened, and bulging, with loss of landmarks. Decreased eardrum mobility is evident on inspection with a pneumatic otoscope. Pus may be seen behind the membrane.

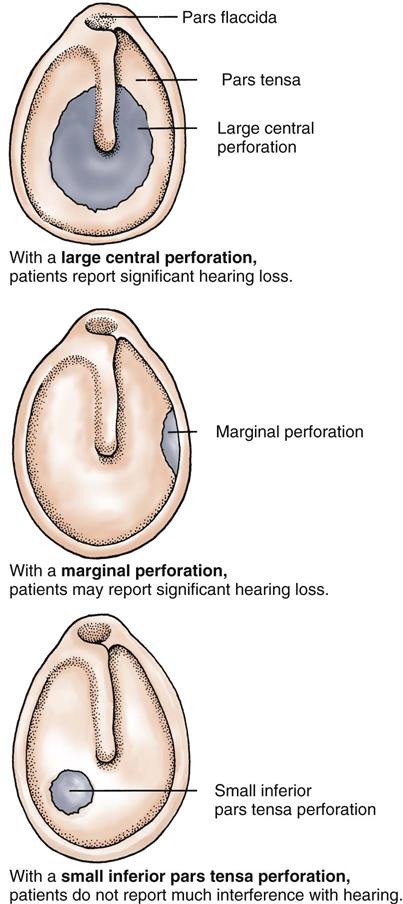
If the condition progresses, the eardrum spontaneously perforates (ruptures) and pus or blood drains from the ear (Fig. 51-4). When the membrane ruptures, the patient notices a marked decrease in pain as the pressure on middle ear structures is relieved (Fig. 51-5). Eardrum perforations from any cause may heal if the underlying problem is controlled. Initially, the eardrum membrane is thinner over the healed perforation. A simple central perforation does not interfere with hearing unless the small bones of the middle ear are damaged or the perforation is large. Repeated perforations with extensive scarring can cause hearing loss.
Cultures of drainage after a perforation from uncontrolled otitis media may reveal the infecting agent. Cultures are taken only when previous treatment is ineffective. When the eardrum is not perforated, a needle aspiration or myringotomy may be performed by a physician or nurse practitioner to withdraw fluid for culture.
Interventions
Nonsurgical Management
Management can be as simple as putting the patient in a quiet environment. Bedrest limits head movements that intensify the pain. Heat may be applied by using a heating pad adjusted to a low setting. Application of cold also may relieve pain.
Topical antibiotics are not used to treat otitis media. Systemic antibiotic therapy decreases pain by reducing inflammation. Teach the patient to complete the antibiotic therapy as prescribed and to not stop taking the drug when manifestations are no longer present. Stopping the drug early may result in infection recurrence and contributes to antibiotic resistance. Analgesics such as aspirin, ibuprofen (Advil), and acetaminophen (Tylenol, Abenol ![]() ) relieve pain and reduce fever, helping the patient feel better. When pain is severe, opioid analgesics such as codeine also may be prescribed.
) relieve pain and reduce fever, helping the patient feel better. When pain is severe, opioid analgesics such as codeine also may be prescribed.
Antihistamines and decongestants are prescribed to decrease fluid in the middle ear. The body can then reabsorb the fluid, reducing pressure and pain.
Surgical Management
If pain persists after antibiotic therapy and the eardrum continues to bulge, a myringotomy (surgical opening of the pars tensa of the eardrum) is performed. This procedure drains middle ear fluids and immediately relieves pain.
Preoperative care includes reassuring the patient that the myringotomy will relieve pain and is usually performed without anesthesia. Many people are concerned about a perforation and its effect on hearing. To relieve some of this anxiety, discuss the reasons for the procedure and encourage the patient to use techniques such as deep breathing before and during the procedure. Systemic antibiotic therapy continues before and after this procedure. Clean the external canal with a bacteriostatic solution such as povidone-iodine (Betadine) before the myringotomy.
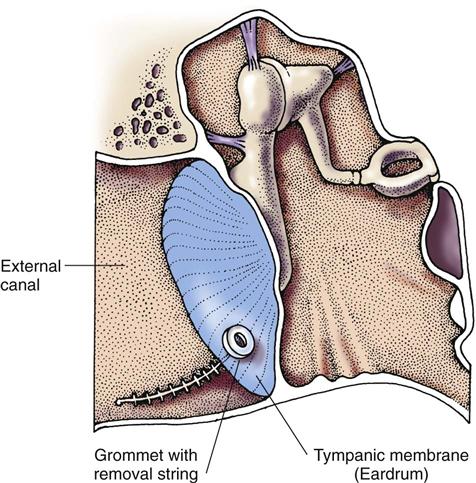
The operative procedure is a small surgical incision often performed in an office or clinic setting and heals rapidly. Another approach is the removal of fluid from the middle ear with a needle. For relief of pressure caused by serous otitis media and for those patients who have repeated episodes of otitis media, a small grommet (polyethylene tube) may be surgically placed through the eardrum to allow continuous drainage of middle ear fluids (Fig. 51-6).
Postoperative care priorities include teaching the patient to keep the external ear and canal free of other substances while the incision is healing. Instruct him or her to keep the head dry by not washing the hair or showering for several days. Other instructions after surgery are listed in Chart 51-4.
Mastoiditis
Pathophysiology
The lining of the middle ear is continuous with the lining of the mastoid air cells, which are embedded in the temporal bone. Mastoiditis is an infection of the mastoid air cells caused by untreated or inadequately treated otitis media. This infection can be acute or chronic. Antibiotic therapy is used to treat the middle ear infection before it progresses to mastoiditis.
Patient-Centered Collaborative Care
The manifestations of mastoiditis include swelling behind the ear and pain with minimal movement of the tragus, the pinna, or the head. Pain is not relieved by myringotomy. Cellulitis (infection spreading sideways through the tissues of the skin) develops on the skin or external scalp over the mastoid process. The ear is pushed sideways and down. Otoscopic examination shows a red, dull, thick, immobile eardrum with or without perforation. Lymph nodes behind the ear are tender and enlarged. Patients may have low-grade fever, malaise, ear drainage, and loss of appetite. Hearing loss occurs, and computed tomography (CT) scans show fluid in the air cells of the mastoid process.
Interventions focus on halting the infection before it spreads to other structures. IV antibiotics are used to prevent the spread of infection. These drugs have limited use in actual mastoiditis treatment because they do not easily penetrate the infected bony structure of the mastoid. Cultures of the ear drainage determine which antibiotics should be most effective. Surgical removal of the infected tissue is needed if the infection does not respond to antibiotic therapy within a few days. A simple or modified radical mastoidectomy with tympanoplasty is the most common treatment. All infected tissue must be removed so that the infection does not spread to other structures. A tympanoplasty is then performed to reconstruct the ossicles and the eardrum to restore hearing. Patient preparation, the operative procedure, and follow-up care for tympanoplasty are discussed on pp. 1101 and 1102.
Complications occur when infective material is not removed completely or when other structures are contaminated. Complications include damage to cranial nerves VI and VII, decreasing the patient’s ability to look sideways (cranial nerve VI) and causing a drooping of the mouth on the affected side (cranial nerve VII). Other complications include vertigo, meningitis, brain abscess, chronic purulent otitis media, and wound infection.
Trauma
Pathophysiology
Trauma and damage may occur to the eardrum and ossicles by infection, by direct damage, or through rapid changes in the middle ear pressure. Foreign objects placed in the external canal exert pressure on the eardrum and cause perforation. If the objects continue through the canal, the bones of the middle ear may be damaged. Blunt injury to the skull and ears can also damage or fracture middle ear structures. Slapping the external ear increases the pressure in the ear canal and can tear the eardrum. The eardrum has a limited stretching ability and gives way under high pressure. Excessive nose blowing and rapid changes of pressure that occur with nonpressurized air flight (barotrauma) can increase pressure within the middle ear. High pressure damages the ossicles and can perforate the eardrum.
Patient-Centered Collaborative Care
Most eardrum perforations heal within a week or two without treatment. Repeated perforations, especially from chronic otitis media, heal more slowly, with scarring. Depending on the amount of damage to the ossicles, hearing may or may not return. Hearing aids can improve hearing in this type of hearing loss. Surgical reconstruction of the ossicles and eardrum through a tympanoplasty or a myringoplasty may also improve hearing. (See later discussion of nursing care on p. 1102 in the Tympanoplasty section.)
Nursing care priorities focus on teaching about trauma prevention. Caution patients to avoid inserting objects into the external canal and to follow the steps in Chart 50-3 in Chapter 50 for ear hygiene. Stress the importance of using ear protectors when blunt trauma is likely, especially in sports such as boxing and wrestling.
Neoplasms
Tumors of the middle ear are rare, and the most common type is the glomus jugulare, a benign lesion arising from the jugular vein. Malignant ear tumors also can occur. The growth of any lesion within the middle ear area disrupts conductive hearing, erodes the ossicles, and may spread to the inner ear and nearby cranial nerves.
Patients have progressive hearing loss and tinnitus. Infection and pain rarely occur with glomus jugulare tumors. Otoscopic examination shows a bulging eardrum or a mass extending to the external ear canal. The many blood vessels of the glomus jugulare tumor give it a reddish color and a visible pulsation when seen through the eardrum.
Diagnosis is made by physical examination, tomography, and angiography. Tumors are removed by surgery, which often destroys hearing in the affected ear. If all of the edges of the tumor can be seen clearly through the eardrum, surgery is performed through the ear canal to remove the tumor. When the tumor edges extend past the eardrum, more testing is needed to determine the extent of involvement. Radiation therapy is used to decrease the blood supply of the glomus jugulare tumor but is not the preferred method of treatment.
Benign tumors are removed because, with continued growth, other structures can be affected, further damaging the facial or trigeminal nerve. When possible, reconstruction of the middle ear structures is performed later to restore conductive hearing.
Conditions Affecting the Inner Ear
Tinnitus
Tinnitus (continuous ringing or noise perception in the ear) is a common hearing problem. Diagnostic testing cannot confirm tinnitus, nor can the disorder be observed. Testing is performed, however, to assess hearing and rule out other disorders.
Manifestation of tinnitus range from mild ringing, which can go unnoticed during the day, to a loud roaring in the ear, which can interfere with thinking and attention span. Some patients feel as if the constant ringing could drive them mad. When patients report tinnitus, consider the many factors that cause tinnitus: presbycusis, otosclerosis (irregular bone growth around ossicles), Ménière’s disease, certain drugs, exposure to loud noise, and other inner ear problems (Bauer & Brozoski, 2008).
The problem and its management vary with the underlying cause (Newman et al., 2008). When no cause can be found or the disorder is untreatable, therapy focuses on ways to mask the tinnitus with background sound, noisemakers, and music during sleeping hours. Ear mold hearing aids can amplify sounds to drown out the tinnitus during the day. The American Tinnitus Association assists patients in coping with tinnitus. Refer patients with tinnitus to local and online support groups to help cope with this problem (Table 51-1).
TABLE 51-1
RESOURCE AGENCIES FOR EAR AND HEARING IMPAIRMENT
| House Research Institute | American Speech-Language-Hearing Association |
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|