Pamela C. Zickafoose
Care of Patients with Dysrhythmias
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Physiological Integrity
4 Identify typical physical assessment findings associated with common dysrhythmias.
5 Explain how to perform an electrocardiogram (ECG) test.
7 Plan collaborative care for patients experiencing common dysrhythmias.
8 Explain the purpose and types of pacing used as interventions for patients with dysrhythmias.
9 Connect and maintain pacing devices.

http://evolve.elsevier.com/Iggy/
Animation: Conduction of Heart Impulses
Animation: Events Represented by the ECG
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
Cardiac dysrhythmias are abnormal rhythms of the heart’s electrical system that can affect its ability to effectively pump oxygenated blood throughout the body. Some dysrhythmias are life threatening, and others are not. They are the result of disturbances of cardiac electrical impulse formation, conduction, or both. When the heart does not work effectively as a pump, perfusion and oxygenation to vital organs and peripheral tissues can be impaired, resulting in organ dysfunction or failure.
Many health problems, especially coronary artery disease (CAD), electrolyte imbalances, changes in oxygenation, and drug toxicity, can cause abnormal heart rhythms. Dysrhythmias can occur in people of any age but occur most often in older adults. To provide collaborative patient-centered care using best practices, a basic understanding of cardiac electrophysiology, the conduction system of the heart, and the principles of electrocardiography is needed as a medical-surgical nurse. Specialty nurses and advanced practice nurses have a more in-depth knowledge as they manage patients with these cardiac problems in critical care areas.
Review of Cardiac Conduction System
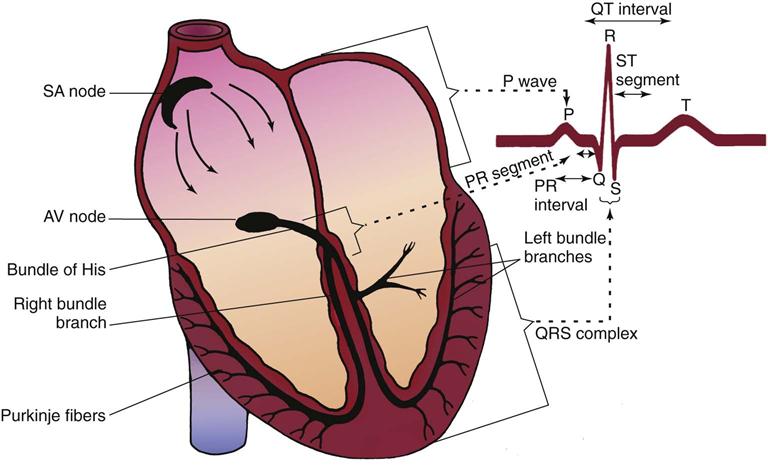
The cardiac conduction system consists of specialized myocardial cells (Fig. 36-1). The electrophysiologic properties of those cells regulate heart rate and rhythm and possess unique properties: automaticity, excitability, conductivity, and contractility.
Automaticity (pacing function) is the ability of cardiac cells to generate an electrical impulse spontaneously and repetitively. Normally, only primary pacemaker cells (sinoatrial [SA] node) can generate an electrical impulse. Under certain conditions, such as myocardial ischemia (decreased blood flow), electrolyte imbalance, hypoxia, drug toxicity, and infarction (cell death), any cardiac cell may produce electrical impulses independently and create dysrhythmias. Disturbances in automaticity may involve either an increase or a decrease in pacing function.
Excitability is the ability of non-pacemaker heart cells to respond to an electrical impulse that begins in pacemaker cells and to depolarize. Depolarization occurs when the normally negatively charged cells within the heart muscle develop a positive charge.
Conductivity is the ability to send an electrical stimulus from cell membrane to cell membrane. As a result, excitable cells depolarize in rapid succession from cell to cell until all cells have depolarized. The wave of depolarization causes the deflections of the electrocardiogram (ECG) waveforms that are recognized as the P wave and the QRS complex. Disturbances in conduction result when conduction is too rapid or too slow, when the pathway is totally blocked, or when the electrical impulse travels an abnormal pathway.
Contractility is the ability of atrial and ventricular muscle cells to shorten their fiber length in response to electrical stimulation, causing sufficient pressure to push blood forward through the heart. In other words, contractility is the mechanical activity of the heart.
Specialized cells of the myocardium are responsible for cardiac conduction. They consist of the sinoatrial node, atrioventricular junctional area, and bundle branch system.
Conduction begins with the sinoatrial (SA) node (also called the sinus node), located close to the surface of the right atrium near its junction with the superior vena cava. The SA node is the heart’s primary pacemaker. It can spontaneously and rhythmically generate electrical impulses at a rate of 60 to 100 beats per minute and therefore has the greatest degree of automaticity.
The SA node is richly supplied by the sympathetic and parasympathetic nervous systems, which increase and decrease the rate of discharge of the sinus node, respectively. This process results in changes in the heart rate.
Impulses from the sinus node move directly through atrial muscle and lead to atrial depolarization, which is reflected in a P wave on the ECG. Atrial muscle contraction should follow. Within the atrial muscle are slow and fast conduction pathways leading to the atrioventricular (AV) node.
The atrioventricular (AV) junctional area consists of a transitional cell zone, the AV node itself, and the bundle of His. The AV node lies just beneath the right atrial endocardium, between the tricuspid valve and the ostium of the coronary sinus. Here T-cells (transitional cells) cause impulses to slow down or to be delayed in the AV node before proceeding to the ventricles. This delay is reflected in the PR segment on the ECG. This slow conduction provides a short delay, allowing the atria to contract and the ventricles to fill. The contraction is known as “atrial kick” and contributes additional blood volume for a greater cardiac output. The AV node is also controlled by both the sympathetic and the parasympathetic nervous systems. The bundle of His connects with the distal portion of the AV node and continues through the interventricular septum.
The bundle of His extends as a right bundle branch down the right side of the interventricular septum to the apex of the right ventricle. On the left side, it extends as a left bundle branch, which further divides.
At the ends of both the right and the left bundle branch systems are the Purkinje fibers. These fibers are an interweaving network located on the endocardial surface of both ventricles, from apex to base. The fibers then partially penetrate into the myocardium. Purkinje cells make up the bundle of His, bundle branches, and terminal Purkinje fibers. These cells are responsible for the rapid conduction of electrical impulses throughout the ventricles, leading to ventricular depolarization and the subsequent ventricular muscle contraction. A few nodal cells in the ventricles also occasionally demonstrate automaticity, giving rise to ventricular beats or rhythms.
Electrocardiography
The electrocardiogram (ECG) provides a graphic representation, or picture, of cardiac electrical activity. The cardiac electrical currents are transmitted to the body surface. Electrodes, consisting of a conductive gel on an adhesive pad, are placed on specific sites on the body and attached to cables connected to an ECG machine or to a monitor. The cardiac electrical current is transmitted via the electrodes and through the lead wires to the machine or monitor, which displays the cardiac electrical activity.
A lead provides one view of the heart’s electrical activity. Multiple leads, or views, can be obtained. Electrode placement is the same for male and female patients.
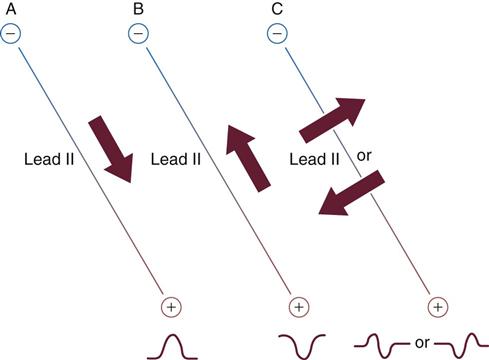
Lead systems are made up of a positive pole and a negative pole. An imaginary line joining these two poles is called the lead axis. The direction of electrical current flow in the heart is the cardiac axis. The relationship between the cardiac axis and the lead axis is responsible for the deflections seen on the ECG pattern:
• If the direction of electrical current flow in the heart (cardiac axis) is toward the positive pole, a positive deflection (above the baseline) is viewed (Fig. 36-2, A).
• If the direction of electrical current flow in the heart (cardiac axis) is moving away from the positive pole toward the negative pole, a negative deflection (below the baseline) is viewed (Fig. 36-2, B).
• If the cardiac axis is moving neither toward nor away from the positive pole, a biphasic complex (both above and below baseline) will result (Fig. 36-2, C).
Lead Systems
The standard 12-lead ECG consists of 12 leads (or views) of the heart’s electrical activity. Six of the leads are called limb leads because the electrodes are placed on the four extremities in the frontal plane. The remaining six leads are called chest (precordial) leads because the electrodes are placed on the chest in the horizontal plane.
Standard bipolar limb leads consist of three leads (I, II, and III) that each measures the electrical activity between two points and a fourth lead (right leg) that acts as a ground electrode. Of the three measuring leads, the right arm is always negative, the left leg is always positive, and the left arm can be either positive or negative.
Other lead systems include the 18-lead ECG, which adds six leads placed on the horizontal plane on the right side of the chest to view the right side of the heart. This is sometimes referred to as a “right-sided ECG.” The extra leads are sometimes placed on the back. The latest evidence indicates an 80-lead ECG, which looks at the heart from 80 views instead of only 12 and gives a 360-degree view of the heart. Evaluation of this 80-lead ECG revealed a 15% increase in diagnosing myocardial infarctions (MIs), particularly in the posterior wall, which was missed in the 12-lead ECG (New 80-lead ECG is easy to interpret, 2008).
Unipolar limb leads consist of a positive electrode only. The unipolar limb leads are aVR, aVL, and aVF, with a meaning augmented. V is a designation for a unipolar lead. The third letter denotes the positive electrode placement: R for right arm, L for left arm, and F for foot (left leg). The positive electrode is at one end of the lead axis. The other end is the center of the electrical field, at about the center of the heart (Table 36-1).
TABLE 36-1
Electrode Placement for 12 Leads
| LEAD | NEGATIVE ELECTRODE | POSITIVE ELECTRODE | GROUND ELECTRODE |
| I | Right arm or under the right clavicle | Left arm or under the left clavicle | Right leg or lowest rib, left midclavicular line |
| II | Right arm or under the right clavicle | Left leg or lowest rib, left midclavicular line | Right leg or under the left clavicle |
| III | Left arm or under the left clavicle | Left leg or lowest rib, left midclavicular line | Right leg or under the right clavicle |
| aVR | Average potential of left arm (or under the left clavicle) and left leg (or lowest rib, left midclavicular line) | Right arm or under the right clavicle | Right leg or lowest rib, right midclavicular line |
| aVL | Average potential of right arm (or under the right clavicle) and left leg (or lowest rib, left midclavicular line) | Left arm or under the left clavicle | Same as for aVR |
| aVF | Average potential of right arm (or under the right clavicle) and left arm (or under the left clavicle) | Left leg or lowest rib, left midclavicular line | Same as for aVR |
| V1 | Average potential of right arm, left arm, and left leg | Fourth intercostal space (ICS), right sternal border | Same as for aVR |
| V2 | Same as for V1 | Fourth ICS, left sternal border | Same as for aVR |
| V3 | Same as for V1 | Midway between V2 and V4 | Same as for aVR |
| V4 | Same as for V1 | Fifth ICS, left midclavicular line | Same as for aVR |
| V5 | Same as for V1 | Horizontal to V4, left anterior axillary line | Same as for aVR |
| V6 | Same as for V1 | Horizontal to V4, left midaxillary line | Same as for aVR |
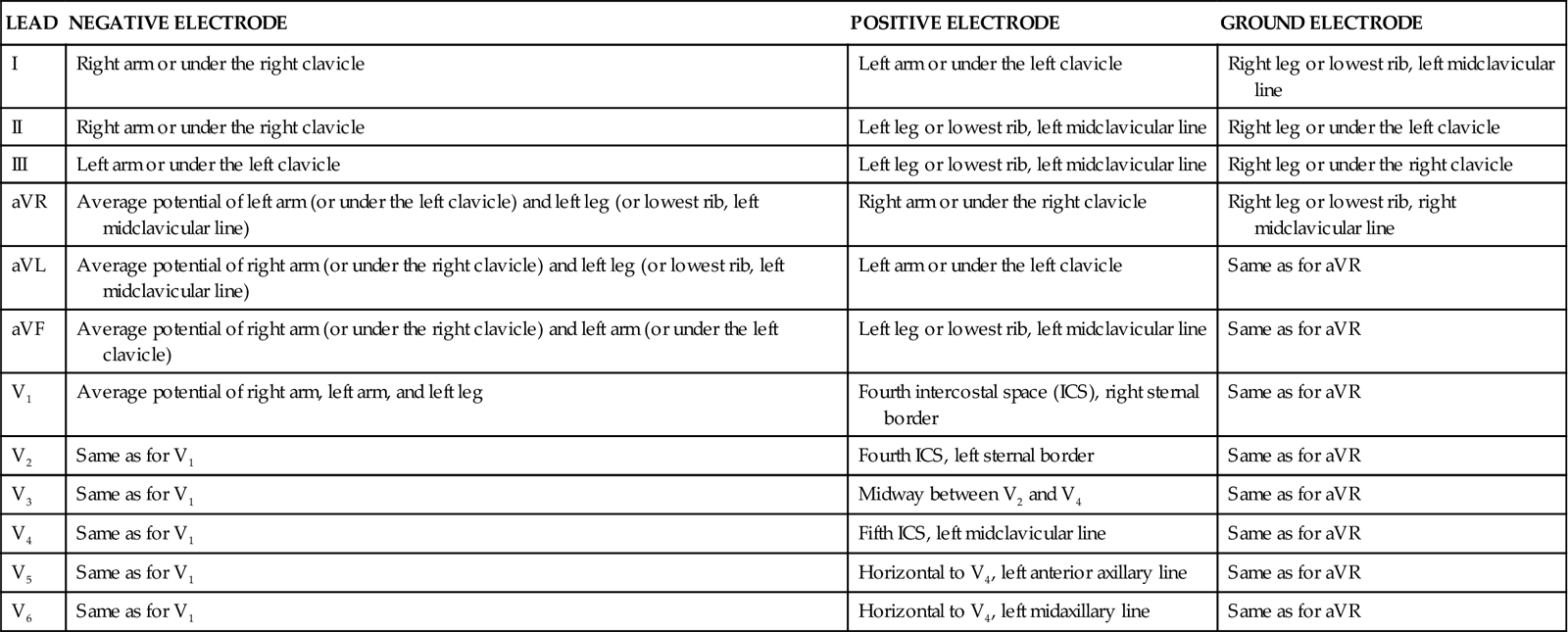
There are six unipolar (or V) chest leads, determined by the placement of the chest electrode. The four limb electrodes are placed on the extremities, as designated on each electrode (right arm, left arm, right leg, and left leg). The fifth (chest) electrode on a monitor system is the positive, or exploring, electrode and is placed in one of six designated positions to obtain the desired chest lead. With a 12-lead ECG, four leads are placed on the limbs and six are placed on the chest, eliminating the need to move any electrodes about the chest.
Positioning of the electrodes is crucial in obtaining an accurate ECG. Comparisons of ECGs taken at different times will be valid only when electrode placement is accurate and identical at each test. Positioning is particularly important when working with patients with chest deformities or large breasts. Patients may be asked to move the breasts to ensure proper electrode placement.
While obtaining a 12-lead ECG, remind the patient to be as still as possible in a semi-reclined position, breathing normally. Any repetitive movement will cause artifact and could lead to inaccurate interpretation of the ECG.
Nurses are sometimes responsible for obtaining 12-lead ECGs, but more commonly, technicians are trained to perform this skill. Remind the technician to notify the nurse or physician of any suspected abnormality. A nurse may direct a technician to take a 12-lead ECG on a patient experiencing chest pain to observe for diagnostic changes, but it is ultimately the physician’s responsibility to interpret the ECG.
Continuous Electrocardiographic Monitoring
For continuous ECG monitoring, the electrodes are not placed on the limbs because movement of the extremities causes “noise,” or motion artifact, on the ECG signal. Place the electrodes on the trunk, a more stable area, to minimize such artifacts and to obtain a clearer signal. If the monitoring system provides five electrode cables, place the electrodes as follows:
• Right arm electrode just below the right clavicle
• Left arm electrode just below the left clavicle
• Right leg electrode on the lowest palpable rib, on the right midclavicular line
• Left leg electrode on the lowest palpable rib, on the left midclavicular line
• Fifth electrode placed to obtain one of the six chest leads
With this placement, the monitor lead select control may be changed to provide lead I, II, III, aVR, aVL, or aVF or one chest lead. The monitor automatically alters the polarity of the electrodes to provide the lead selected.
The clarity of continuous ECG monitor recordings is affected by skin preparation and electrode quality. To ensure the best signal transmission and to decrease skin impedance, clean the skin and clip hairs or shave the area if needed. Make sure the area for electrode placement is dry. The gel on each electrode must be moist and fresh. Attach the electrode to the lead cable and then to the contact site. The contact site should be free of any lotion, tincture, or other substance that increases skin impedance. Electrodes cannot be placed on irritated skin or over scar tissue. The application of electrodes may be done by unlicensed assistive personnel (UAP), but the nurse must determine which lead to select and check for correct electrode placement. Assess the quality of the ECG rhythm transmission to the monitoring system.
The ECG cables can be attached directly to a wall-mounted monitor (a hard-wired system) if the patient’s activity is restricted to bedrest and sitting in a chair, as in a critical care unit. For an ambulatory patient, the ECG cable is attached to a battery-operated transmitter (a telemetry system) held in a pouch. The ECG is transmitted to a remote monitor via antennae located in strategic places, usually in the ceiling. Telemetry allows freedom of movement within a certain area without losing transmission of the ECG.
Most acute care facilities have monitor technicians (monitor “techs”) who are educated in ECG rhythm interpretation and are responsible for:
• Watching a bank of monitors on a unit
• Printing ECG rhythm strips routinely and as needed
• Reporting the patient’s rhythm and significant changes to the nurse
The technical support is particularly helpful on a telemetry unit that does not have monitors at the bedside. The nurse remains ultimately responsible for accurate ECG rhythm interpretation, as well as for patient assessment and management.
Some units have full-disclosure monitors, which continuously store ECG rhythms in memory up to a certain amount of time, allowing nurses and health care providers to access and print them for more thorough patient assessment and management. Routine strips, as well as any changes in rhythm, are printed and documented in the patient’s record.
The health care provider is responsible for determining when monitoring can be suspended, such as during showering. He or she also determines whether monitoring is needed during off-unit testing procedures and for transportation to other facilities.
Prehospital personnel, such as paramedics and emergency medical technicians (EMTs) with advanced training, frequently monitor ECG rhythms at the scene and on the way to a health care facility. They function under medical direction and protocols but may also be communicating with a nurse in the emergency department.
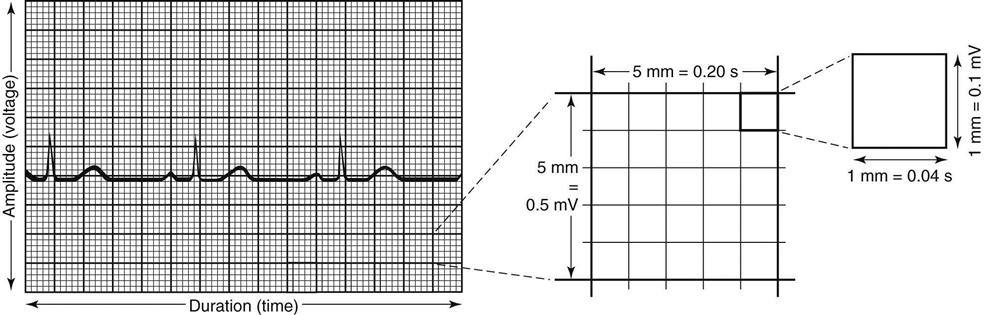
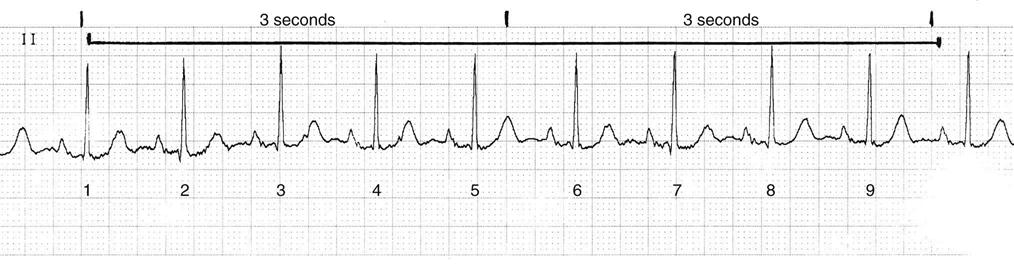
The ECG strip is printed on graph paper (Fig. 36-3), with each small block measuring 1 mm in height and width. ECG recorders and monitors are standardized at a speed of 25 mm/sec. Time is measured on the horizontal axis. At this speed, each small block represents 0.04 second. Five small blocks make up one large block, defined by darker bold lines and representing 0.20 second. Five large blocks represent 1 second, and 30 large blocks represent 6 seconds. Vertical lines in the top margin of the graph paper are usually 15 large blocks apart, representing 3-second segments (Fig. 36-4).
Electrocardiographic Complexes, Segments, and Intervals
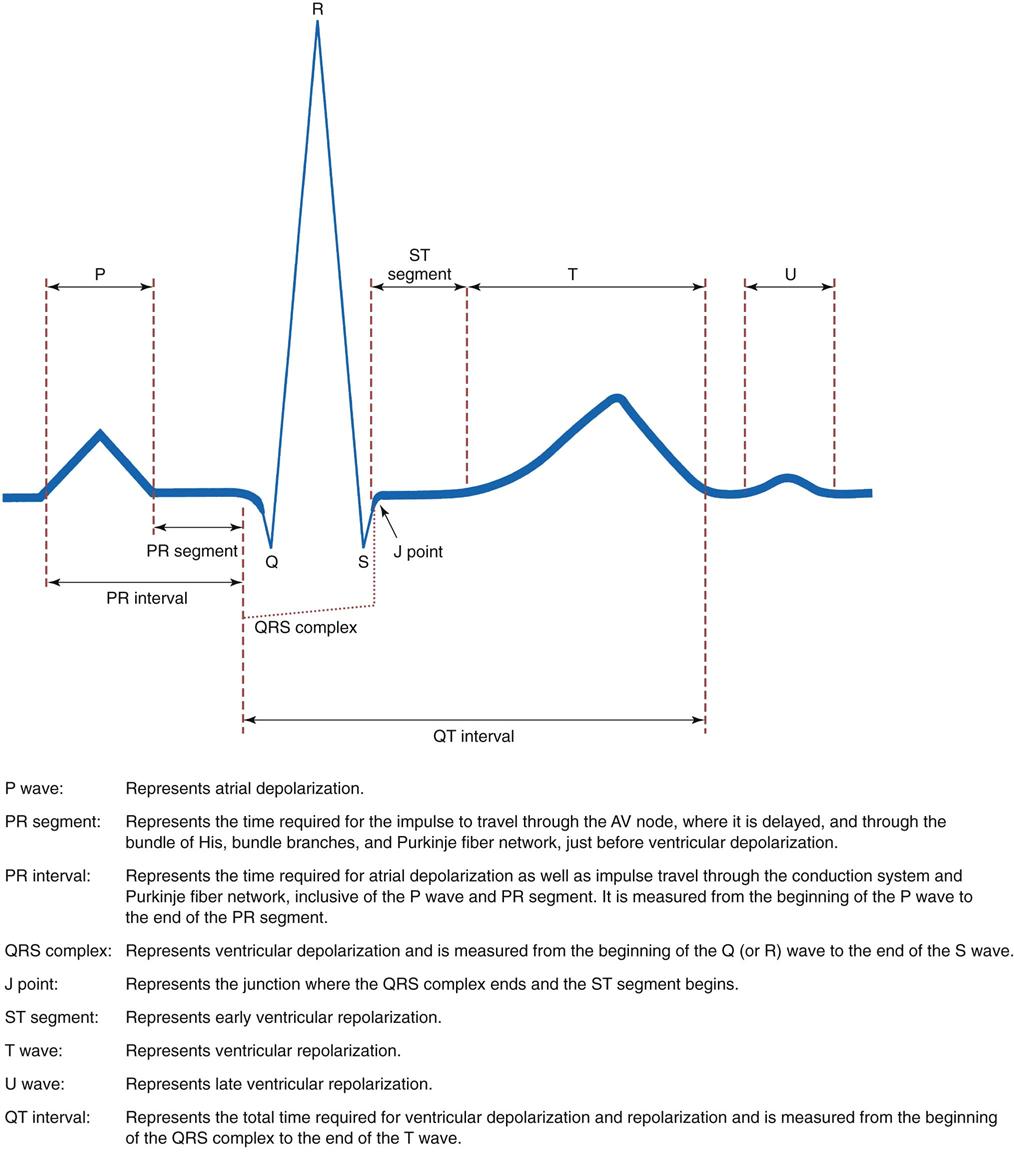
Complexes that make up a normal ECG consist of a P wave, a QRS complex, a T wave, and possibly a U wave. Segments include the PR segment, the ST segment, and the TP segment. Intervals include the PR interval, the QRS duration, and the QT interval (Fig. 36-5).
The P wave is a deflection representing atrial depolarization. The shape of the P wave may be a positive, negative, or biphasic (both positive and negative) deflection, depending on the lead selected. When the electrical impulse is consistently generated from the sinoatrial (SA) node, the P waves have a consistent shape in a given lead. If an impulse is then generated from a different (ectopic) focus, such as atrial tissue, the shape of the P wave changes in that lead, indicating that an ectopic focus has fired.
The PR segment is the isoelectric line from the end of the P wave to the beginning of the QRS complex, when the electrical impulse is traveling through the atrioventricular (AV) node, where it is delayed. It then travels through the ventricular conduction system to the Purkinje fibers.
The PR interval is measured from the beginning of the P wave to the end of the PR segment. It represents the time required for atrial depolarization as well as the impulse delay in the AV node and the travel time to the Purkinje fibers. It normally measures from 0.12 to 0.20 second (five small blocks).
The QRS complex represents ventricular depolarization. The shape of the QRS complex depends on the lead selected. The Q wave is the first negative deflection and is not present in all leads. When present, it is small and represents initial ventricular septal depolarization. When the Q wave is abnormally present in a lead, it represents myocardial necrosis (cell death). The R wave is the first positive deflection. It may be small, large, or absent, depending on the lead. The S wave is a negative deflection following the R wave and is not present in all leads.
The QRS duration represents the time required for depolarization of both ventricles. It is measured from the beginning of the QRS complex to the J point (the junction where the QRS complex ends and the ST segment begins). It normally measures from 0.04 to 0.10 second (up to three small blocks).
The ST segment is normally an isoelectric line and represents early ventricular repolarization. It occurs from the J point to the beginning of the T wave. Its length varies with changes in the heart rate, the administration of medications, and electrolyte disturbances. It is normally not elevated more than 1 mm or depressed more than 0.5 mm from the isoelectric line. Its amplitude is measured at a point 1.5 to 2 mm after the J point. ST elevation or depression can be caused by myocardial injury, ischemia or infarction, conduction abnormalities, or the administration of medications.
The T wave follows the ST segment and represents ventricular repolarization. It is usually positive, rounded, and slightly asymmetric. If an ectopic stimulus excites the ventricles during this time, it may cause ventricular irritability, lethal dysrhythmias, and possible cardiac arrest in the vulnerable heart. This is known as the R-on-T phenomenon. T waves may become tall and peaked, inverted (negative), or flat as a result of myocardial ischemia, potassium or calcium imbalances, medications, or autonomic nervous system effects.
The U wave, when present, follows the T wave and may result from slow repolarization of ventricular Purkinje fibers. It is of the same polarity as the T wave, although generally it is smaller. It is not normally seen in all leads and is more common in lead V3. An abnormal U wave may suggest an electrolyte abnormality (particularly hypokalemia) or other disturbance. Correct identification is important so that it is not mistaken for a P wave. If in doubt, notify the health care provider and request that a potassium level be obtained.
The QT interval represents the total time required for ventricular depolarization and repolarization. The QT interval is measured from the beginning of the QRS complex to the end of the T wave. This interval varies with the patient’s age and gender and changes with the heart rate, lengthening with slower heart rates and shortening with faster rates. It may be prolonged by certain medications, electrolyte disturbances, Prinzmetal’s angina, or subarachnoid hemorrhage. A prolonged QT interval may lead to a unique type of ventricular tachycardia called torsades de pointes.
Artifact is interference seen on the monitor or rhythm strip, which may look like a wandering or fuzzy baseline. It can be caused by patient movement, loose or defective electrodes, improper grounding, or faulty ECG equipment, such as broken wires or cables. Some artifact can mimic lethal dysrhythmias like ventricular tachycardia (with tooth brushing) or ventricular fibrillation (with tapping on the electrode). Assess the patient to differentiate artifact from actual lethal rhythms! Do not rely only on the ECG monitor.
Determination of Heart Rate
The heart rate can be estimated by counting the number of QRS complexes in 6 seconds and multiplying that number by 10 to calculate the rate for a full minute. This is called the 6-second strip method and is a quick method to determine the mean or average heart rate. This method is the least accurate; however, it is the method of choice for irregular rhythms.
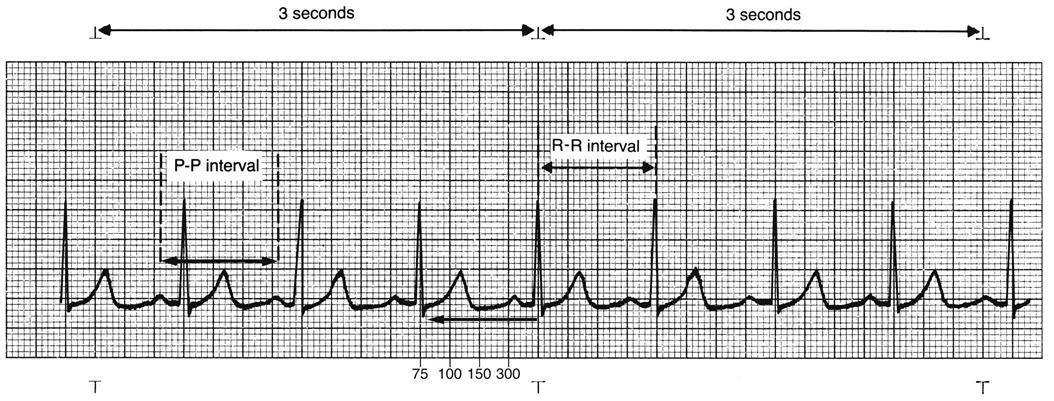
For accuracy, the big block method is used if the QRS complexes are regular or evenly spaced. Count the number of big blocks between the same point in any two successive QRS complexes (usually R wave to R wave) and divide into 300. There are 300 big blocks in 1 minute. It is easiest to use a QRS that falls on a dark line. If little blocks are left over when counting big blocks, count each little block as 0.2, add this to the number of big blocks, and then divide that total into 300 (Fig. 36-6).
Count the number of large blocks in an interval and divide into 300 (the number of large blocks in 1 minute). For example, three large blocks equals a heart rate of 100 beats per minute (300 ÷ 3 = 100).
Another method (called the memory method) relies on memorizing this sequence: 300, 150, 100, 75, 60, 50, 43, 37, 33, 30. This is the big block method with the math already done. Find a QRS complex that falls on the dark line representing 0.2 second or a big block, and count backwards to the next QRS complex. Each dark line is a memorized number. This is the method most widely used in hospitals for calculating heart rates for regular rhythms.
Commercially prepared ECG rate rulers are based on these calculations and may be used for regular rhythms. Current monitoring systems will display a continuous heart rate and print the heart rate on the ECG strip. Use caution and confirm that the rate is correct by assessing the patient’s heart rate directly. Many factors can incorrectly alter the rate displayed by the monitor.
Electrocardiographic Rhythm Analysis
Analysis of an ECG rhythm strip requires a systematic approach using a six-step method facilitated by use of a measurement tool called an ECG caliper:
2 Determine the heart rhythm. Heart rhythms can be either regular or irregular. Irregular rhythms can be regularly irregular, occasionally irregular, or irregularly irregular. Check the regularity of the atrial rhythm by assessing the PP intervals, placing one caliper point on a P wave and placing the other point on the precise spot on the next P wave. Then move the caliper from P wave to P wave along the entire strip (“walking out” the P waves) to determine the regularity of the rhythm. P waves of a different shape (ectopic waves), if present, create an irregularity and do not walk out with the other P waves. A slight irregularity in the PP intervals, varying no more than three small blocks, is considered essentially regular if the P waves are all of the same shape. This alteration is caused by changes in intrathoracic pressure during the respiratory cycle.
Check the regularity of the ventricular rhythm by assessing the RR intervals, placing one caliper point on a portion of the QRS complex (usually the most prominent portion of the deflection) and the other point on the precise spot of the next QRS complex. Move the caliper from QRS complex to QRS complex along the entire strip (walking out the QRS complexes) to determine the regularity of the rhythm. QRS complexes of a different shape (ectopic QRS complexes), if present, create an irregularity and do not walk out with the other QRS complexes. A slight irregularity of no more than three small blocks between intervals is considered essentially regular if the QRS complexes are all of the same shape.
3 Analyze the P waves. Check that the P wave shape is consistent throughout the strip, indicating that atrial depolarization is occurring from impulses originating from one focus, normally the SA node. Determine whether there is one P wave occurring before each QRS complex, establishing that a relationship exists between the P wave and the QRS complex. This relationship indicates that an impulse from one focus is responsible for both atrial and ventricular depolarization. The nurse may observe more than one P wave shape, more P waves than QRS complexes, absent P waves, or P waves coming after the QRS, each indicating that a dysrhythmia exists. Ask these five questions when analyzing P waves:
• Are the P waves occurring regularly?
• Is there one P wave for each QRS complex?
• Are the P waves smooth, rounded, and upright in appearance, or are they inverted?
• Do all the P waves look similar?
4 Measure the PR interval. Place one caliper point at the beginning of the P wave and the other point at the end of the PR segment. The PR interval normally measures between 0.12 and 0.20 second. The measurement should be constant throughout the strip. The PR interval cannot be determined if there are no P waves or if P waves occur after the QRS complex. Ask these three questions about the PR interval:
• Are PR intervals greater than 0.20 second?
• Are PR intervals less than 0.12 second?
• Are PR intervals constant across the ECG strip?
5 Measure the QRS duration. Place one caliper point at the beginning of the QRS complex and the other at the J point, where the QRS complex ends and the ST segment begins. The QRS duration normally measures between 0.04 and 0.10 second. The measurement should be constant throughout the entire strip. Check that the QRS complexes are consistent throughout the strip. When the QRS is narrow (0.10 second or less), this indicates that the impulse was not formed in the ventricles and is referred to as supraventricular or above the ventricles. When the QRS complex is wide (greater than 0.10 second), this indicates that the impulse is either of ventricular origin or of supraventricular origin with aberrant conduction, meaning deviating from the normal course or pattern. More than one QRS complex pattern or occasionally missing QRS complexes may be observed, indicating a dysrhythmia.
Ask these questions to evaluate QRS intervals:
• Are QRS intervals less than or greater than 0.12 second?
• Are the QRS complexes similar in appearance across the ECG paper?
Normal Rhythms
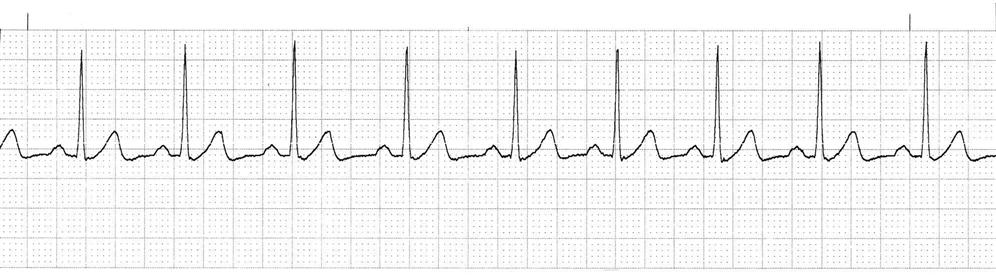
Normal sinus rhythm (NSR) is the rhythm originating from the sinoatrial (SA) node (dominant pacemaker) that meets these ECG criteria (Fig. 36-7):
• Rate: Atrial and ventricular rates of 60 to 100 beats/min
• Rhythm: Atrial and ventricular rhythms regular
• P waves: Present, consistent configuration, one P wave before each QRS complex
• PR interval: 0.12 to 0.20 second and constant
Sinus arrhythmia is a variant of NSR. It results from changes in intrathoracic pressure during breathing. In this context, the term arrhythmia does not mean an absence of rhythm, as the term suggests. Instead, the heart rate increases slightly during inspiration and decreases slightly during exhalation. This irregular rhythm is frequently observed in healthy children as well as adults.
Sinus arrhythmia has all the characteristics of NSR except for its irregularity. The PP and RR intervals vary, with the difference between the shortest and the longest intervals being greater than 0.12 second (three small blocks):
• Rate: Atrial and ventricular rates between 60 and 100 beats/min
• P waves: One P wave before each QRS complex; consistent configuration
• PR interval: Normal, constant
Sinus arrhythmias occasionally are due to nonrespiratory causes, such as digitalis or morphine. These drugs enhance vagal tone and cause decreased heart rate and irregularity unrelated to the respiratory cycle.
Dysrhythmias
Overview
Any disorder of the heartbeat is called a dysrhythmia. Historically, the term arrhythmia has been used in the literature. Although the terms are often used interchangeably, dysrhythmia is more accurate. Dysrhythmias result from:
• A disturbance in impulse formation (either from an abnormal rate or from an ectopic focus)
• A disturbance in impulse conduction (delays and blocks)
Although many dysrhythmias have no clinical manifestations, many others have serious consequences if not treated. A summary of key features is found in Chart 36-1.
Dysrhythmia Terminology
Tachydysrhythmias are heart rates greater than 100 beats per minute. They are a major concern in the adult patient with coronary artery disease (CAD). Coronary artery blood flow occurs mostly during diastole when the aortic valve is closed and is determined by diastolic time and blood pressure in the root of the aorta. Tachydysrhythmias are serious because they:
The patient with a tachydysrhythmia may have:
Tachydysrhythmias may also lead to heart failure. Presenting symptoms of heart failure may include dyspnea, lung crackles, distended neck veins, fatigue, and weakness (see Chapter 37).
Bradydysrhythmias occur when the heart rate is less than 60 beats per minute. These rhythms can also be significant because:
• Myocardial oxygen demand is reduced from the slow heart rate, which can be beneficial.
• Coronary perfusion time may be adequate because of a prolonged diastole, which is desirable.
Therefore the patient may tolerate the bradydysrhythmia well if the blood pressure is adequate. If the blood pressure is not adequate, symptomatic bradydysrhythmias may lead to myocardial ischemia or infarction, dysrhythmias, hypotension, and heart failure.
Premature complexes are early rhythm complexes. They occur when a cardiac cell or cell group, other than the sinoatrial (SA) node, becomes irritable and fires an impulse before the next sinus impulse is produced. The abnormal focus is called an ectopic focus and may be generated by atrial, junctional, or ventricular tissue. After the premature complex, there is a pause before the next normal complex, creating an irregularity in the rhythm. The patient with premature complexes may be unaware of them or may feel palpitations or a “skipping” of the heartbeat. If premature complexes, especially those that are ventricular, become more frequent, the patient may experience symptoms of decreased cardiac output.
Premature complexes may occur repetitively in a rhythmic fashion:
Such patterns may occur with atrial, junctional, or ventricular premature complexes. Patients may be unaware of the premature beats, or they may feel palpitations.
Classification of Dysrhythmias
Dysrhythmias are classified according to their site of origin. The sites include the SA node, atrial tissue, AV node, junctional tissue, and ventricular tissue. Dysrhythmias may be caused by a disturbance in impulse formation or by conduction delays or blocks. The incidence and the prevalence of dysrhythmias are not known because they usually result from an underlying condition, such as heart disease. This chapter is limited to the most common dysrhythmias and those that are potentially life threatening.
Sinus Dysrhythmias.
The sinus node is the pacemaker in all sinus dysrhythmias. Innervation from sympathetic and parasympathetic nerves is normally in balance to ensure a normal sinus rhythm (NSR). An imbalance increases or decreases the rate of SA node discharge either as a normal response to activity or physiologic changes or as a pathologic response to disease.
Sinus Tachycardia.
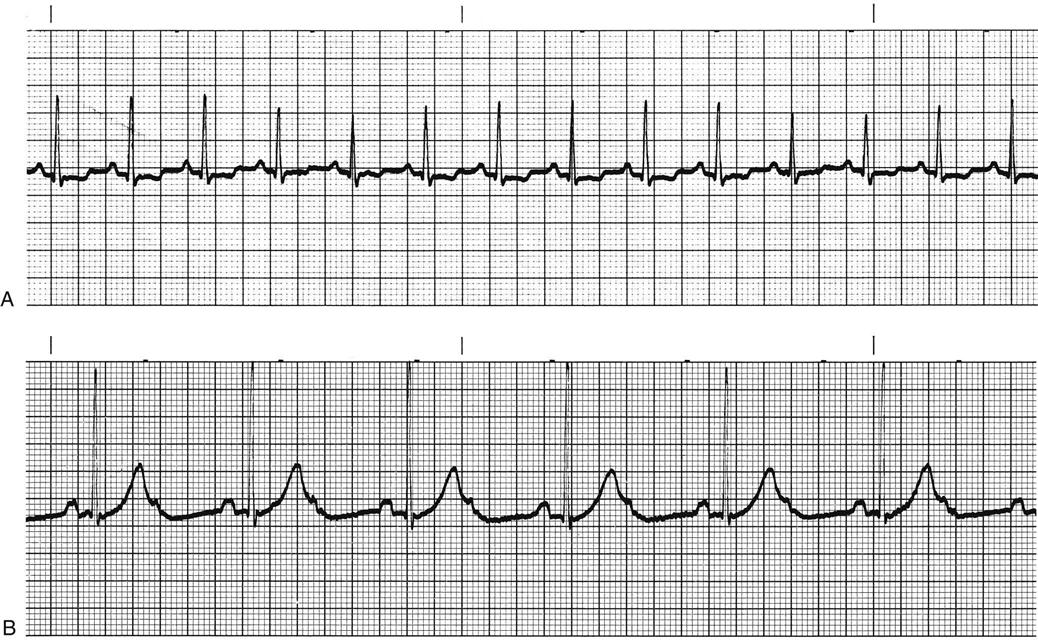
Sympathetic nervous system stimulation or vagal (parasympathetic) inhibition results in an increased rate of SA node discharge, which increases the heart rate. When the rate of SA node discharge is more than 100 beats per minute, the rhythm is called sinus tachycardia (Fig. 36-8, A). Sinus tachycardia, with temporary heart rates of 200 to 220 beats per minute, may be normal in infants and children. The rate gradually decreases until age 10 years. From age 10 years to adulthood, the heart rate normally does not exceed 100 beats per minute except in response to activity, and then usually does not exceed 160 beats per minute. Rarely does the heart rate reach 180 beats per minute.
Sinus tachycardia initially increases cardiac output and blood pressure. However, continued increases in heart rate decrease coronary perfusion time, diastolic filling time, and coronary perfusion pressure while increasing myocardial oxygen demand.
Increased sympathetic stimulation is a normal response to physical activity but may also be caused by anxiety, pain, stress, fear, fever, anemia, hypoxemia, hyperthyroidism, and pulmonary embolism. Drugs such as epinephrine, atropine, caffeine, alcohol, nicotine, aminophylline, and thyroid medications may also increase the heart rate. In some cases, sinus tachycardia is a compensatory response to decreased cardiac output or blood pressure, as occurs in hypovolemic shock, myocardial infarction (MI), infection, and heart failure.
The patient may be asymptomatic except for an increased pulse rate. However, if the rhythm is not well tolerated, he or she may have symptoms.
The desired outcome is to decrease the heart rate to normal levels by treating the underlying cause. Teach the patient to remain on bedrest if the tachycardia is causing hypotension or weakness.
Sinus Bradycardia.
Excessive vagal (parasympathetic) stimulation to the heart causes a decreased rate of sinus node discharge. It may result from carotid sinus massage, vomiting, suctioning, Valsalva maneuvers (e.g., bearing down for a bowel movement or gagging), ocular pressure, or pain. Increased parasympathetic stimuli may also result from hypoxia, inferior wall MI, and the administration of drugs such as beta-adrenergic blocking agents, calcium channel blockers, and digitalis.
The stimuli slow the heart rate and decrease the speed of conduction through the heart. When the sinus node discharge rate is less than 60 beats/min, the rhythm is called sinus bradycardia (Fig. 36-8, B). Sinus bradycardia increases coronary perfusion time, but it may decrease coronary perfusion pressure. However, myocardial oxygen demand is decreased. Well-conditioned athletes who are bradycardic have a hypereffective heart, in which the strong heart muscle provides an adequate stroke volume and a low heart rate to achieve a normal cardiac output.
The patient with sinus bradycardia may be asymptomatic except for the decreased pulse rate. At times, however, the rhythm may not be well tolerated. Assess the patient for:
If the patient has any of these symptoms and the underlying cause cannot be determined, the treatment is to administer drug therapy, increase intravascular volume via IV fluids, and apply oxygen. If the heart rate does not increase sufficiently, pacing may be needed to increase the heart rate.
Atrial Dysrhythmias.
With atrial dysrhythmias, the focus of impulse generation shifts away from the sinus node to the atrial tissues. The shift changes the axis (direction) of atrial depolarization, resulting in a P-wave shape that differs from normal P waves. The most common atrial dysrhythmias are:
Premature Atrial Complexes.
A premature atrial complex (PAC) occurs when atrial tissue becomes irritable. This ectopic focus fires an impulse before the next sinus impulse is due. The premature P wave may not always be clearly visible because it can be hidden in the preceding T wave. Examine the T wave closely for any change in shape, and compare with other T waves. A PAC is usually followed by a pause.
The causes of atrial irritability include:
• Stress
• Fatigue
• Anxiety
• Caffeine, nicotine, or alcohol
• Drugs such as epinephrine, sympathomimetics, amphetamines, digitalis, or anesthetic agents
PACs may also result from myocardial ischemia, hypermetabolic states, electrolyte imbalance, or atrial stretch. Atrial stretch can result from congestive heart failure, valvular disease, and pulmonary hypertension with cor pulmonale.
The patient usually has no symptoms except for possible heart palpitations. No intervention is needed except to treat causes such as heart failure. If PACs occur frequently, they may lead to more serious atrial tachydysrhythmias and therefore may need treatment. Administration of prescribed antidysrhythmic drugs may be necessary. Teach the patient measures to manage stress and substances to avoid, such as caffeine and alcohol, that are known to increase atrial irritability.
Supraventricular Tachycardia.
Supraventricular tachycardia (SVT) involves the rapid stimulation of atrial tissue at a rate of 100 to 280 beats/min in adults. During SVT, P waves may not be visible, especially if there is a 1 : 1 conduction with rapid rates, because the P waves are embedded in the preceding T wave. SVT may occur in healthy young people, especially women.
SVT is usually due to a re-entry mechanism in which one impulse circulates repeatedly throughout the atrial pathway, re-stimulating the atrial tissue at a rapid rate. The term paroxysmal supraventricular tachycardia (PSVT) is used when the rhythm is intermittent. It is initiated suddenly by a premature complex such as a PAC and terminated suddenly with or without intervention.
The clinical manifestations depend on the duration of the SVT and the rate of the ventricular response. In patients with a sustained rapid ventricular response, assess for palpitations, chest pain, weakness, fatigue, shortness of breath, nervousness, anxiety, hypotension, and syncope. Cardiovascular deterioration may occur if the rate does not sustain adequate blood pressure. In that case, SVT can result in angina, heart failure, and cardiogenic shock. With a nonsustained or slower ventricular response, the patient may be asymptomatic except for occasional palpitations.
If SVT occurs in a healthy person and stops on its own, no intervention may be needed other than eliminating identified causes. If it continues, the patient should be studied in the electrophysiology study (EPS) laboratory. The preferred treatment for recurrent SVT is radiofrequency catheter ablation, described later in this chapter. In sustained SVT with a rapid ventricular response, the desired outcomes of treatment are to decrease the ventricular response, convert the dysrhythmia to a sinus rhythm, and treat the cause. Chart 36-2 lists drugs that may be used for SVT.
 mo before full clinical effects are apparent.
mo before full clinical effects are apparent.


