Tammy Coffee
Care of Patients with Burns
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
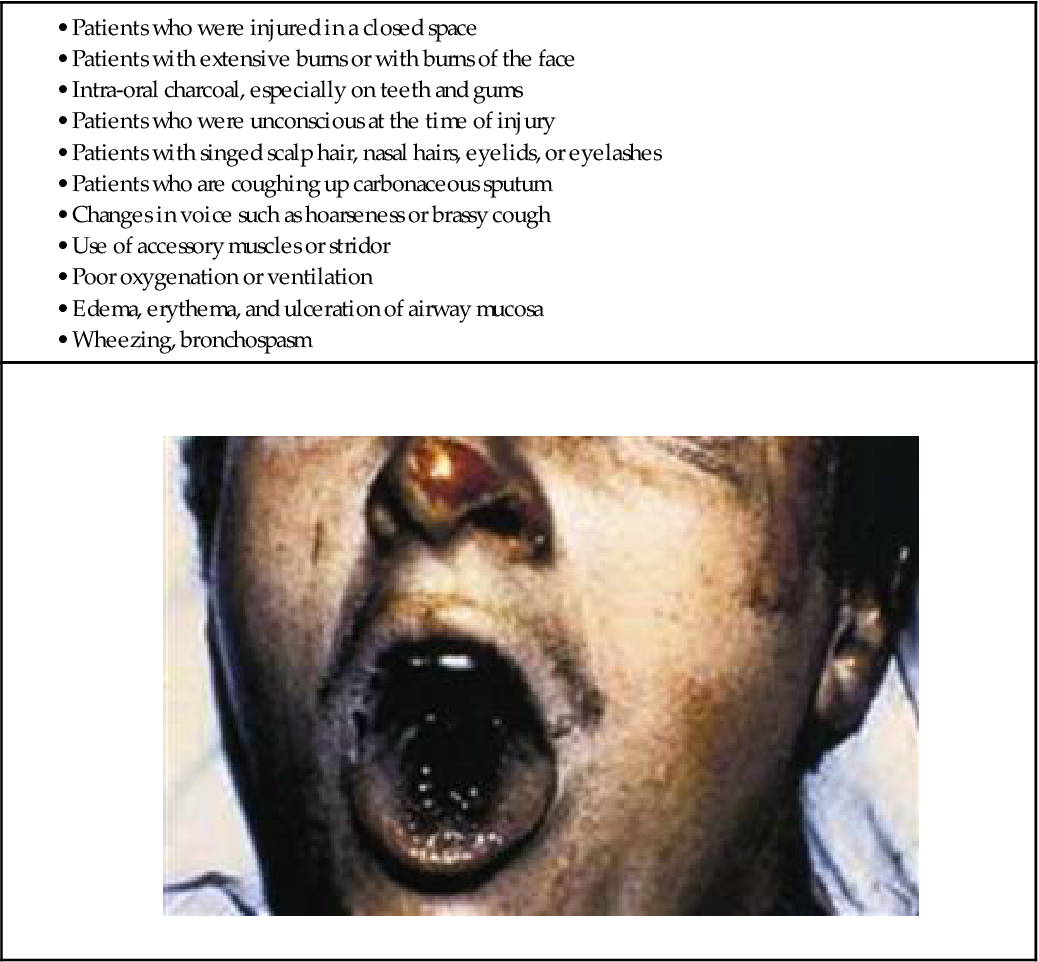
9 Identify burn patients at risk for inhalation injury.
10 Compare the manifestations of superficial, partial-thickness, and full-thickness burn injuries.
12 Prioritize nursing care for the patient during the resuscitation phase of burn injury.
14 Prioritize nursing care for the patient during the acute phase of burn injury.
16 Evaluate the patient’s wound healing during the acute phase of burn injury.
18 Describe the characteristics of infected burn wounds.
20 Coordinate nursing care for the patient during the rehabilitation phase of burn injury.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Clip: High- and Low-Pitched Crackles
Audio Clip: High- and Low-Pitched Wheezes
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
Patients who have burn injuries develop many physiologic, metabolic, and psychological changes. Burn injuries can range from a “sunburn” to major injuries involving all layers of the skin. When the skin is injured, inflammation and fluid loss change the function of most body systems. The burn patient needs comprehensive care for weeks to months to survive the injury, reduce complications, and return to his or her best functional status. A multidisciplinary team of health care providers is needed for best care and patient outcomes. Nurses coordinate the activities of the many professionals involved in providing the best care to burn patients.
Introduction to the Burn Problem
Pathophysiology of Burn Injury
The tissue destruction caused by a burn injury leads to many local and systemic problems. Such problems include fluid and protein losses, sepsis, and changes in metabolic, endocrine, respiratory, cardiac, hematologic, and immune functioning. The extent of local and systemic problems is related to age, general health, extent of injury, depth of injury, and the specific body area injured. Even after healing, the burn injury may cause late complications such as contracture formation and scarring. Therefore the prevention of infection and closure of the burn wound are vitally important. A lack of or delay in wound healing is a key factor for all systemic problems and a major cause of disability and death among patients who are burned.
Skin Changes Resulting from Burn Injury
Anatomic Changes.
The skin is the largest organ of the body (see Chapter 26). Each of its two major layers, the epidermis and the dermis, has several sublayers. The epidermis, the outer layer of skin, is a layer of stratified epithelial cells about 0.15 mm thick (somewhat thinner in older adults). This layer can grow back after a burn injury because the epidermal cells surrounding sweat and oil glands and hair follicles extend into dermal tissue and regrow to heal partial-thickness wounds. Together, the sweat and oil glands and the hair follicles are the dermal appendages. The depth of the dermal appendages varies in different body areas. The sweat and oil glands in the palm of the hand and the sole of the foot, for example, extend deep into the dermis. This allows for healing of deep burns in these areas. The epidermis has no blood vessels. Nutrients to this layer diffuse from the second layer of skin, the dermis.
The dermis is thicker than the epidermis and is made up of collagen, fibrous connective tissue, and elastic fibers. Within the dermis are the blood vessels, sensory nerves, hair follicles, lymph vessels, sebaceous glands, and sweat glands.
When burn injury occurs, skin can regrow as long as parts of the dermis are present. When the entire layer of dermis is burned, all epithelial cells and dermal appendages are destroyed and the skin can no longer restore itself. The subcutaneous tissue lies below the dermis and varies in thickness. The basement membrane, a thin, noncellular protein surface, separates the dermis from the subcutaneous tissue layer. With deep burns, the subcutaneous tissues may be damaged, leaving bones, tendons, and muscles exposed.
Functional Changes.
The skin has many functions (see Table 26-1 in Chapter 26). It is a protective barrier against injury and microbial invasion. Burns break this barrier, greatly increasing the risk for infection.
The skin also helps maintain the delicate fluid and electrolyte balance essential for life. After a burn injury, massive fluid loss occurs through evaporation. Evaporation through burn-injured skin occurs four times as rapidly as through intact skin. The rate of evaporation is in proportion to the total body surface area (TBSA) burned and the depth of injury.
The skin is an excretory organ through sweating. Full-thickness burns destroy the sweat glands, reducing excretory ability.
The sensations of pain, pressure, temperature, and touch are triggered on the skin in normal daily activities, which allows a person to react to changes in the environment. All burn injuries are painful. With partial-thickness burns, nerve endings are exposed, increasing sensitivity and pain. With full-thickness burns, nerve endings are completely destroyed. At first these wounds may not transmit sensation except at wound edges when a sharp stimulus is applied. Despite this destruction, patients often have dull or pressure-type of pain in these areas.
Skin exposed to sunlight activates vitamin D. Partial-thickness burns reduce the activation of vitamin D, and this function is lost completely in full-thickness burns.
The internal body temperature remains within a narrow range (about 84.2° to 109.4° F [29° to 43° C]) compared with the wide temperature changes in the external environment. Several processes normally adjust changes in external temperature to maintain the narrow normal range of internal body temperature. Circulating blood both provides and dissipates heat efficiently. When heat is applied to the skin, the temperature of the layer under the dermis rises rapidly. As soon as the heat source is removed, compensatory processes quickly return the area to a normal temperature. If the heat source is not removed or if it is applied at a rate that exceeds the skin’s capacity to dissipate it, cells are destroyed.
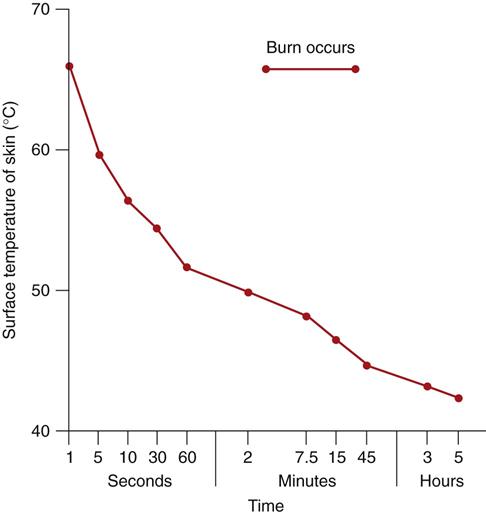
The skin can tolerate temperatures up to 104° F (40° C) without injury. At temperatures of 158° F (70° C) and above, cell destruction is so rapid that even brief exposure damages the skin and tissue below the skin. Fig. 28-1 shows the relationship between temperature and exposure time for burn injury.
Physical identity is partly determined by the skin’s cosmetic quality, which contributes to each person’s unique appearance. A patient who sustains a major burn is likely to develop a reduced self-image and other psychosocial problems as a result of a change in appearance.
Depth of Burn Injury.
The severity of a burn is determined by how much of the body surface area is involved and the depth of the burn. The degree of tissue damage is related to the agent causing the burn and to the temperature of the heat source, as well as to how long the skin is exposed to it.
Differences in skin thickness in various parts of the body also affect burn depth. In areas where the skin is thin (e.g., eyelids, ears, nose, genitalia, tops of the hands and feet, fingers, and toes), a short exposure to high temperatures causes a deep burn injury. The skin is thinner in older adults (Touhy & Jett, 2010), which increases their risk for greater burn severity, even at lower temperatures of shorter duration.
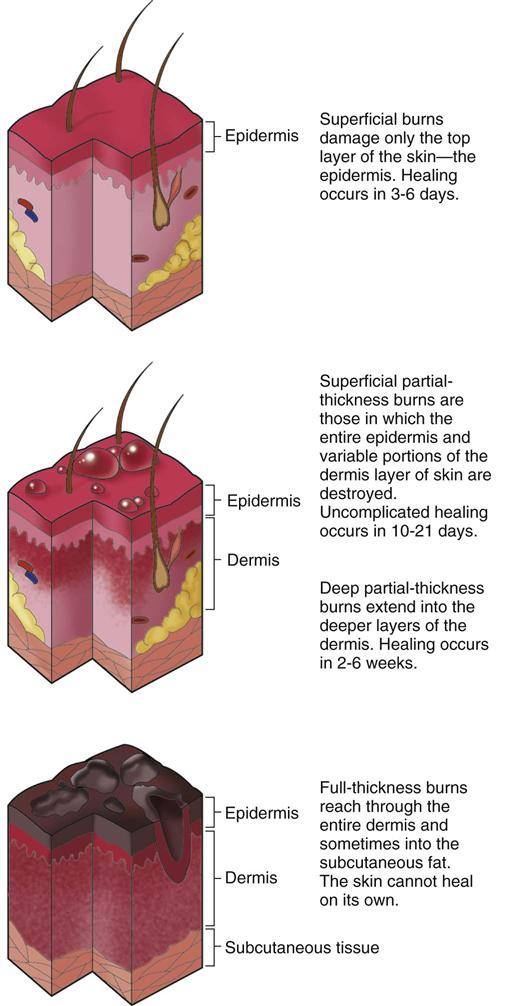
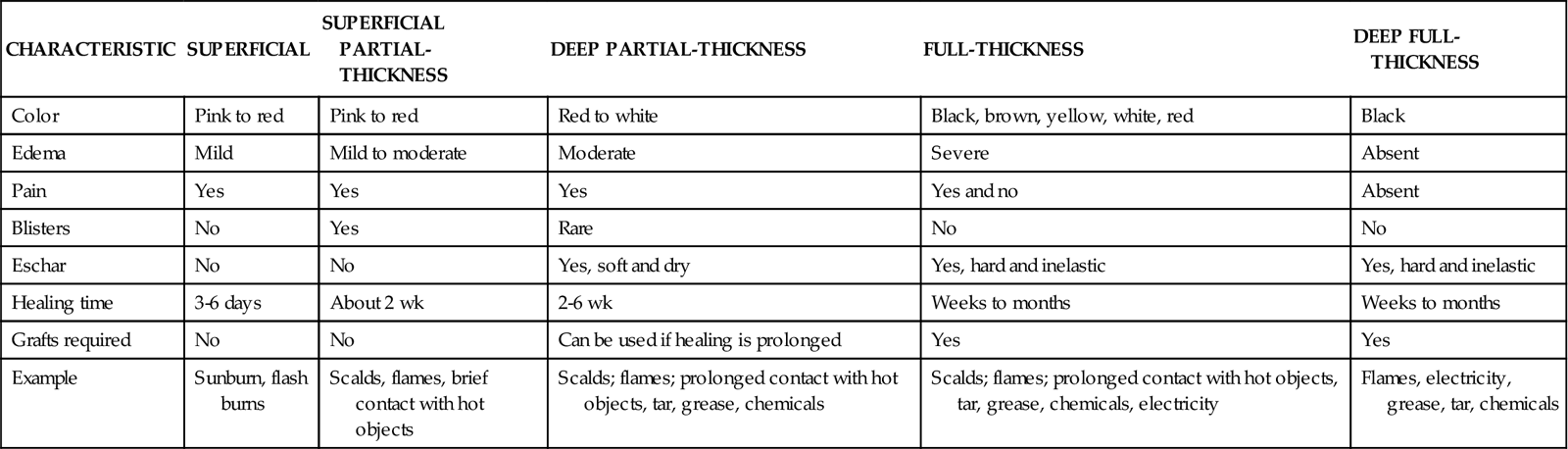
Burn wounds are classified as superficial-thickness wounds, partial-thickness wounds, full-thickness wounds, and deep full-thickness wounds. The partial-thickness wounds are further divided into superficial and deep subgroups (McCance et al, 2010). Table 28-1 lists the clinical differences of these burns.
TABLE 28-1
| CHARACTERISTIC | SUPERFICIAL | SUPERFICIAL PARTIAL-THICKNESS | DEEP PARTIAL-THICKNESS | FULL-THICKNESS | DEEP FULL-THICKNESS |
| Color | Pink to red | Pink to red | Red to white | Black, brown, yellow, white, red | Black |
| Edema | Mild | Mild to moderate | Moderate | Severe | Absent |
| Pain | Yes | Yes | Yes | Yes and no | Absent |
| Blisters | No | Yes | Rare | No | No |
| Eschar | No | No | Yes, soft and dry | Yes, hard and inelastic | Yes, hard and inelastic |
| Healing time | 3-6 days | About 2 wk | 2-6 wk | Weeks to months | Weeks to months |
| Grafts required | No | No | Can be used if healing is prolonged | Yes | Yes |
| Example | Sunburn, flash burns | Scalds, flames, brief contact with hot objects | Scalds; flames; prolonged contact with hot objects, tar, grease, chemicals | Scalds; flames; prolonged contact with hot objects, tar, grease, chemicals, electricity | Flames, electricity, grease, tar, chemicals |
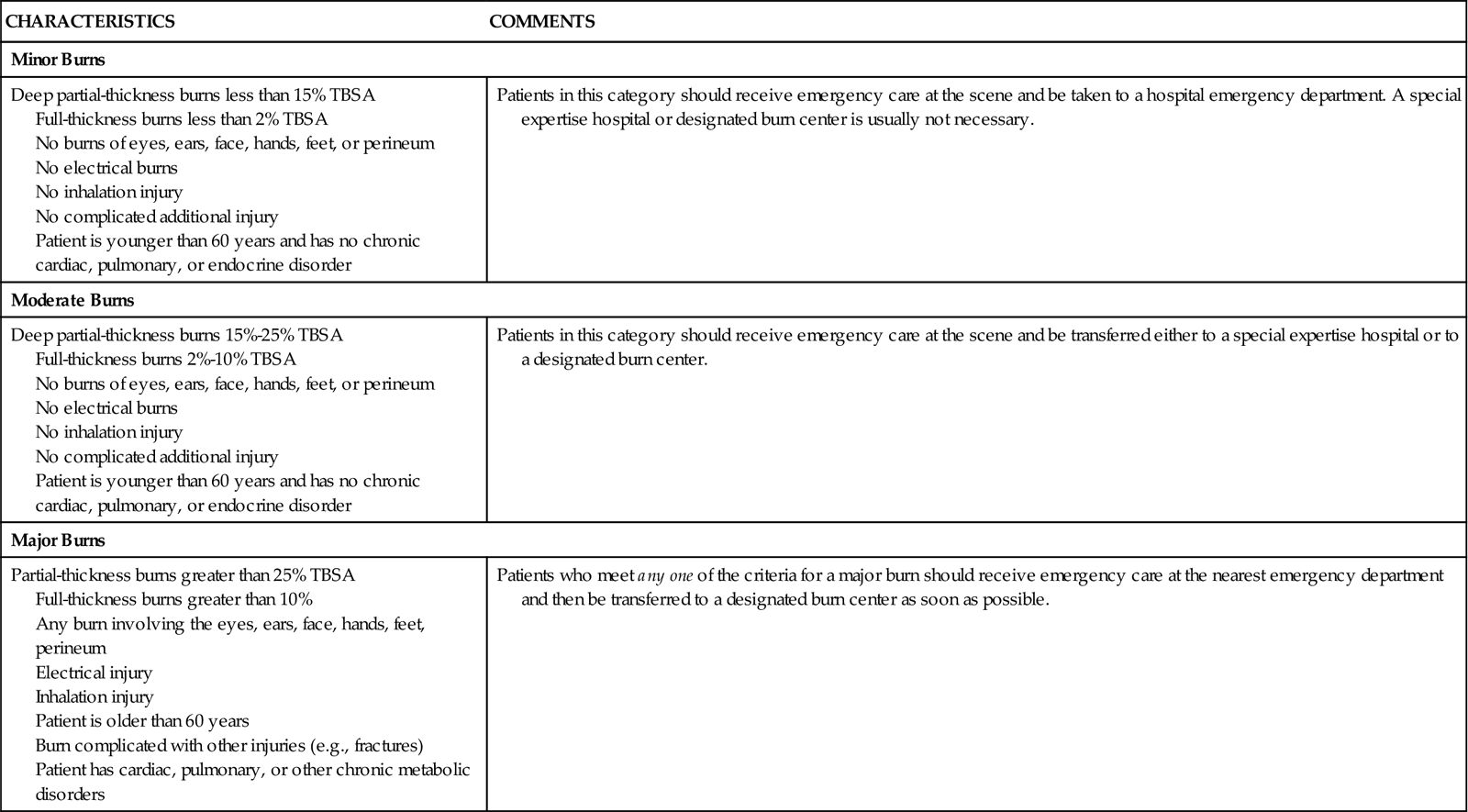
The American Burn Association (ABA) describes burns as minor, moderate, or major depending on the depth, extent, and location of injury (Table 28-2). Fig. 28-2 shows the tissue layers involved with different depths of injury.
TABLE 28-2
CLASSIFICATION OF BURN INJURY AND BURN CENTER REFERRAL CRITERIA
| CHARACTERISTICS | COMMENTS |
| Minor Burns | |
| Deep partial-thickness burns less than 15% TBSA Full-thickness burns less than 2% TBSA No burns of eyes, ears, face, hands, feet, or perineum No electrical burns No inhalation injury No complicated additional injury Patient is younger than 60 years and has no chronic cardiac, pulmonary, or endocrine disorder | Patients in this category should receive emergency care at the scene and be taken to a hospital emergency department. A special expertise hospital or designated burn center is usually not necessary. |
| Moderate Burns | |
| Deep partial-thickness burns 15%-25% TBSA Full-thickness burns 2%-10% TBSA No burns of eyes, ears, face, hands, feet, or perineum No electrical burns No inhalation injury No complicated additional injury Patient is younger than 60 years and has no chronic cardiac, pulmonary, or endocrine disorder | Patients in this category should receive emergency care at the scene and be transferred either to a special expertise hospital or to a designated burn center. |
| Major Burns | |
| Partial-thickness burns greater than 25% TBSA Full-thickness burns greater than 10% Any burn involving the eyes, ears, face, hands, feet, perineum Electrical injury Inhalation injury Patient is older than 60 years Burn complicated with other injuries (e.g., fractures) Patient has cardiac, pulmonary, or other chronic metabolic disorders | Patients who meet any one of the criteria for a major burn should receive emergency care at the nearest emergency department and then be transferred to a designated burn center as soon as possible. |
Superficial-Thickness Wounds.
Of all burn types, superficial-thickness wounds have the least damage because the epidermis is the only part of the skin that is injured. The epithelial cells and basement membrane, needed for total regrowth, remain present.
Superficial-thickness wounds are caused by prolonged exposure to low-intensity heat (e.g., sunburn) or short (flash) exposure to high-intensity heat. Redness with mild edema, pain, and increased sensitivity to heat occurs as a result. Desquamation (peeling of dead skin) occurs for 2 to 3 days after the burn. The area heals rapidly in 3 to 6 days without a scar or other complication.
Partial-Thickness Wounds.
A partial-thickness wound involves the entire epidermis and varying depths of the dermis. Depending on the amount of dermal tissue damaged, partial-thickness wounds are further subdivided into superficial partial-thickness and deep partial-thickness injuries.
Superficial partial-thickness wounds are caused by injury to the upper third of the dermis, leaving a good blood supply. These wounds are red and moist and blanch (lighten) when pressure is applied (Fig. 28-3). The small vessels bringing blood to this area are injured, resulting in the leakage of large amounts of plasma, which in turn lifts off the heat-destroyed epidermis, causing blister formation. The blisters continue to increase in size after the burn as cell and protein breakdown occur. Small blisters are often left intact if they are not located over a joint. Large blisters usually are opened and débrided to promote healing.
Superficial partial-thickness wounds increase pain sensation. Nerve endings are exposed, and any stimulation (touch or temperature change) causes intense pain. With standard care, these burns heal in 10 to 21 days with no scar but some minor pigment changes may occur.
Deep partial-thickness wounds extend deeper into the skin dermis, and fewer healthy cells remain. Blisters usually do not form because the dead tissue layer is thick, sticks to the underlying dermis, and does not readily lift off the surface. The wound surface is red and dry with white areas in deeper parts (dry because fewer blood vessels are patent). When pressure is applied to the burn, it blanches slowly or not at all (Fig. 28-4). Edema is moderate, and pain is less than with superficial burns because more of the nerve endings have been destroyed.
Blood flow to these areas is reduced by blood vessel constriction. Progression to deeper injury can occur from hypoxia and ischemia. Adequate hydration, nutrients, and oxygen are needed for regrowth of skin cells and prevention of conversion to deeper burns. These wounds can convert to full-thickness wounds when tissue damage increases with infection, hypoxia, or ischemia. Deep partial-thickness wounds generally heal in 3 to 6 weeks, but scar formation results. Surgical intervention with skin grafting can reduce healing time.
Full-Thickness Wounds.
A full-thickness wound occurs with destruction of the entire epidermis and dermis, leaving no skin cells to repopulate (Fig. 28-5). This wound does not regrow, and areas not closed by wound contraction (see Chapter 27) require grafting.
The full-thickness burn has a hard, dry, leathery eschar that forms from coagulated particles of destroyed dermis. The eschar is dead tissue; it must slough off or be removed from the wound before healing can occur. These thick particles often stick to the lower tissue layer by collagen fibers, which make eschar removal difficult. Edema is severe under the eschar in a full-thickness wound. When the injury is circumferential (completely surrounds an extremity or the chest), blood flow and chest movement for breathing may be reduced by tight eschar. Escharotomies (incisions through the eschar) or fasciotomies (incisions through eschar and fascia) may be needed to relieve pressure and allow normal blood flow and breathing (see p. 527 of the Surgical Management discussion in the Preventing Hypovolemic Shock and Inadequate Oxygenation section).
A full-thickness burn wound may be waxy white, deep red, yellow, brown, or black. Thrombosed vessels may be visible beneath the surface of the burn. These dermal blood vessels are heat coagulated, causing the burned tissue to be avascular (without a blood supply). Sensation is reduced or absent in these areas because of nerve ending destruction. Healing time depends on establishing a good blood supply in the injured areas. This process can range from weeks to months.
Deep Full-Thickness Wounds.
Deep full-thickness wounds extend beyond the skin into underlying fascia and tissues. These deep injuries damage muscle, bone, and tendons and leave them exposed. These burns occur with flame, electrical, or chemical injuries. The wound is blackened and depressed, and sensation is completely absent (Fig. 28-6). All full-thickness burns need early excision and grafting. Grafting decreases pain and length of stay and hastens recovery. Amputation may be needed when an extremity is involved.
Vascular Changes Resulting from Burn Injury
Circulatory disruption occurs at the burn site immediately after injury. Blood vessels to the burned skin are occluded, and blood flow is reduced or stopped. Damaged macrophages within the tissues release chemicals that at first cause blood vessel constriction. Blood vessel thrombosis may occur, causing necrosis, which can lead to deeper injuries in these areas.
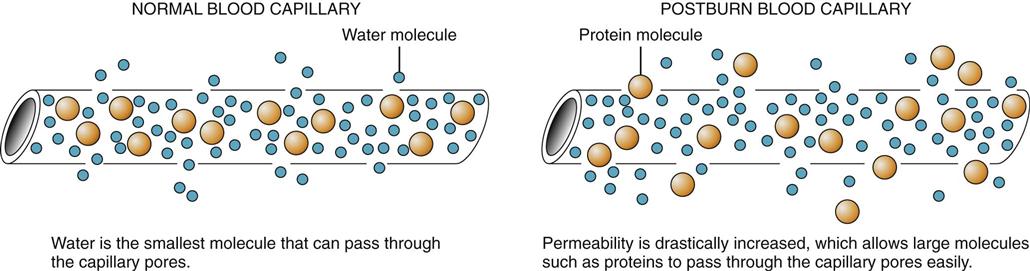
Fluid shift occurs after initial vasoconstriction as a result of blood vessels near the burn dilating and leaking fluid into the interstitial space (Fig. 28-7). This fluid shift, also known as third spacing or capillary leak syndrome, is a continuous leak of plasma from the vascular space into the interstitial space. The loss of plasma fluids and proteins decreases blood volume and blood pressure. Leakage of fluid and electrolytes from the vascular space continues, causing extensive edema, even in areas that were not burned. Fluid shift, with excessive weight gain, occurs in the first 12 hours after the burn and can continue for 24 to 36 hours.
The amount of fluid shifted depends on the extent and severity of injury. Capillary leak occurs in both burned and unburned areas when tissue damage is extensive (i.e., more than 20% to 30% total body surface area [TBSA]). Edema develops as plasma and electrolytes escape into the interstitial space. The proteins now in the interstitial space increase the movement of fluids out from the vascular space.
Profound imbalances of fluid, electrolytes, and acid-base occur as a result of the fluid shift and cell damage. These imbalances often include hypovolemia, metabolic acidosis, hyperkalemia (high blood potassium level), and hyponatremia (low blood sodium level). Hyperkalemia occurs as a result of direct cell injury that releases large amounts of cellular potassium. Sodium is retained by the body as a result of the endocrine response to stress. Aldosterone secretion increases, leading to increased sodium reabsorption by the kidney. This sodium, however, quickly passes into the interstitial spaces of the burned area with the fluid shift. Thus, despite the increased amount of sodium in the body, most of the sodium is trapped in the interstitial space and a sodium deficit occurs in the blood. Hemoconcentration (elevated blood osmolarity, hematocrit, and hemoglobin) develops from vascular dehydration. This problem increases blood viscosity, reducing flow through small vessels and increasing tissue hypoxia.
Fluid remobilization starts at about 24 hours after injury, when the capillary leak stops. The diuretic stage begins at about 48 to 72 hours after the burn injury as capillary membrane integrity returns and edema fluid shifts from the interstitial spaces into the intravascular space. Blood volume increases, leading to increased kidney blood flow and diuresis unless kidney damage has occurred. Body weight returns to normal over the next few days as edema subsides.
During this phase, hyponatremia develops because of increased kidney sodium excretion and the loss of sodium from wounds. Hypokalemia (low blood potassium level) results from potassium moving back into the cells and also being excreted in urine. Anemia often develops as a result of hemodilution, but it is generally not severe enough to require blood transfusions. Transfusions are needed if the patient’s hematocrit is less than 20% to 25% and the patient has manifestations of hypoxia. Transfusions are given only when absolutely necessary. Protein continues to be lost from the wounds. Metabolic acidosis is possible because of the loss of bicarbonate in the urine and the increased fat metabolism that occurs because of decreased carbohydrate intake.
Cardiac Changes Resulting from Burn Injury
Heart rate increases and cardiac output decreases because of the initial fluid shifts and hypovolemia that occur after a burn injury. Cardiac output may remain low until 18 to 36 hours after the burn injury. Cardiac output increases with fluid resuscitation and reaches normal levels before plasma volume is restored completely. Proper fluid resuscitation and support with oxygen prevent further complications.
Pulmonary Changes Resulting from Burn Injury
Direct injury to the lung from contact with flames rarely occurs. Rather, respiratory problems are caused by superheated air, steam, toxic fumes, or smoke. Such problems are a major cause of death in patients with burns and are most likely to occur when the burn takes place indoors. Respiratory failure with burn injuries can result from airway edema during fluid resuscitation, pulmonary capillary leak, chest burns that restrict chest movement, and carbon monoxide poisoning.
Respiratory damage from an inhalation injury can occur in the upper and major airways and the lung tissue (Cancio et al., 2007). The upper airway is affected when inhaled smoke or irritants cause edema and obstruct the trachea. Irritants coming in contact with the upper airway often cause a reflex closure of the vocal cords. This protective reflex reduces the entry of smoke and toxic gases into the lungs. Heat can reach the upper airway, causing an inflammatory response that leads to edema of the mouth and throat with the potential of airway obstruction.
The chemicals and toxic gases that are produced during combustion cause more airway injury than does the heat. The ciliated membranes lining the trachea normally trap bacteria and foreign materials. Smoke and combustion products slow this activity, which allows foreign particles to enter the bronchi. The lining of the trachea and bronchi may slough 48 to 72 hours after injury, enter the airway, narrow the tracheal lumen, and obstruct the lower airways.
Lung tissue injuries result from toxic irritant damage to the alveoli and capillaries. Leaking capillaries cause alveolar edema. This edema can occur immediately or as late as 1 week after the injury. The fluid that diffuses into the lung tissue spaces contains proteins that form fibrinous membranes and lead to respiratory distress. Progressive pulmonary failure develops, leading to acute pulmonary insufficiency and infection.
Gastrointestinal Changes Resulting from Burn Injury
The fluid shifts and decreased cardiac output that occur after injury divert blood flow to the brain, heart, and liver. As a result, the GI tract has decreased blood flow. Gastric mucosal integrity and motility are impaired. The sympathetic nervous system stress response increases secretion of epinephrine and norepinephrine, which inhibit GI motility and further reduce blood flow to the area. Peristalsis decreases, and a paralytic ileus may develop. Secretions and gases collect in the intestines and stomach, causing abdominal distention.
Curling’s ulcer (acute gastroduodenal ulcer that occurs with the stress of severe injury) may develop within 24 hours after a severe burn injury because of reduced GI blood flow and mucosal damage (McCance et al., 2010). The mucus lining the stomach normally is a barrier to the hydrogen ions secreted into the stomach contents. With decreased gastric mucus production, this barrier is disrupted and hydrogen ion production is increased and ulcers may develop as a result. However, this complication is now less common because of the use of H2 histamine blockers, proton pump inhibitors, drugs that protect GI tissues, and early enteral feeding.
Metabolic Changes Resulting from Burn Injury
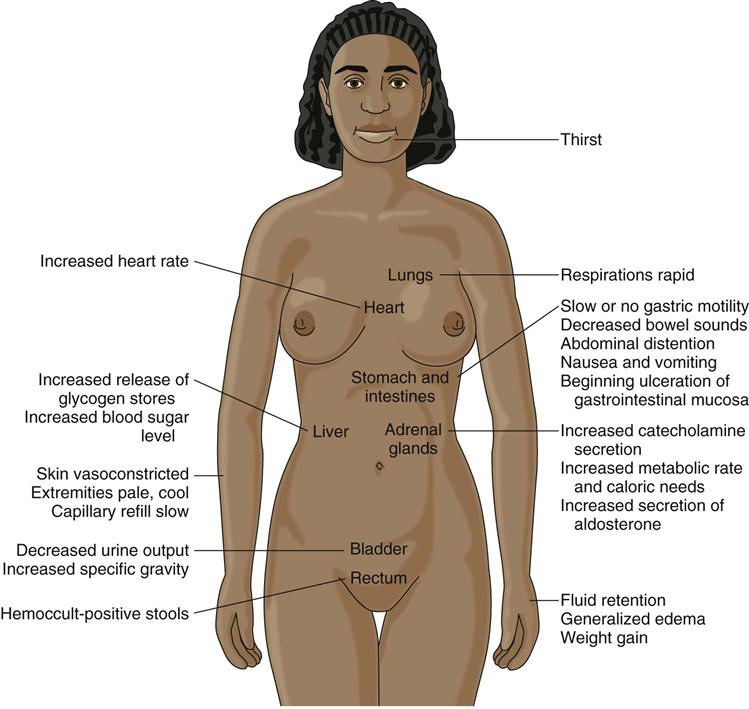
A serious burn injury greatly increases metabolism by increasing secretion of catecholamines, antidiuretic hormone, aldosterone, and cortisol. With this hypermetabolism, the patient’s oxygen use and calorie needs are high.
The catecholamines activate the stress response. The increased production (and loss) of heat breaks down protein and fat (a process called catabolism), rapidly uses glucose and calories, and increases urine nitrogen loss. The heat and water lost from the burn also increase metabolic and catabolic rates, which increase calorie needs. Depending on the extent of injury, the patient’s calorie needs double or triple normal energy needs. These increased rates peak 4 to 12 days after the burn and can remain elevated for months until all wounds are closed.
The hypermetabolic condition also increases core body temperature. The patient loses heat through the burned areas because the barrier is lost. Core body temperature increases as a response to the adjustment in temperature regulation by the hypothalamus. A central body temperature control change occurs to adapt to the hypermetabolic state, resulting in the development of a low-grade fever. This change is a “resetting” of the body’s normal temperature-control system to a higher baseline body temperature.
Immunologic Changes Resulting from Burn Injury
Burn injury disrupts or destroys the protective barrier of the skin, increasing the risk for infection. The injury activates the inflammatory response and often suppresses all types of immune functions. Topical and systemic antibiotics, general anesthesia, blood transfusion, and the stress of surgery further reduce immune function.
Compensatory Responses to Burn Injury
Any tissue injury is a stressor and can disrupt homeostasis. Two compensatory (adaptive) responses have immediate benefit: the inflammatory response and the sympathetic nervous system stress response. Together these responses cause changes that result in many of the manifestations seen in the first 2 to 3 days after a burn injury.
Inflammatory compensation can be helpful by triggering healing in the injured tissues. It also is responsible for some of the serious problems that occur with the fluid shift. Inflammatory compensation causes blood vessels to leak fluid into the interstitial space and white blood cells to release chemicals that trigger local tissue reactions. These responses cause the massive fluid shift, edema, and hypovolemia that are seen in the resuscitation phase (first 24 to 48 hours) after a burn injury. The extent of the inflammatory response depends on the burn severity. Chapter 19 explains the inflammatory responses in detail.
Inflammatory compensation is immediately helpful to the body when injury occurs. These actions are intended to function on a local and short-term basis. When these actions are widespread or persistent, they can cause severe tissue damage.
Sympathetic nervous system compensation is the stress response that occurs when any physical or psychological stressors are present. Changes caused by sympathetic compensation are most evident in the cardiovascular, respiratory, and GI systems. Fig. 28-8 shows the results of sympathetic nervous system stimulation.
Etiology of Burn Injury
Burn injuries are caused by dry heat (flame), moist heat (scald), contact with hot surfaces, chemicals, electricity, and ionizing radiation. The cause of the injury affects both the prognosis and the treatment.
Dry heat injuries are caused by open flame. The most common flame injuries occur in house fires and explosions. Ignited clothing from an open flame accounts for most of the injuries. Explosions usually result in flash burns because they produce a brief exposure to very high temperatures.
Moist heat (scald) injuries are caused by contact with hot liquids or steam. Scald injuries are more common among older adults than among younger adults. Hot liquid spills usually burn the upper, front areas of the body. Immersion scald injuries usually involve the lower body.
Contact burns occur when hot metal, tar, or grease contacts the skin, often leading to a full-thickness injury. Hot metal injuries occur when a body part contacts a hot surface, such as a space heater or iron. They also can occur in industrial settings from molten metals. Tar and asphalt temperatures usually are greater than 400° F, and deep injuries occur within seconds when the skin is immersed in or splashed with them. Hot grease injuries from cooking are usually deep because of the high temperature of the grease.
Chemical burns occur as a result of accidents in homes or industry. They can also be the result of a deliberate assault. Injury occurs when chemicals directly contact the skin and epithelial tissues or are ingested. The severity of the injury depends on the duration of contact, the concentration of the chemical, the amount of tissue exposed, and the action of the chemical.
Alkalis found in oven cleaners, fertilizers, drain cleaners, and heavy industrial cleaners damage the tissues by causing the skin and its proteins to liquefy. This allows for deeper spread of the chemical and more severe burns. Acids found in bathroom cleaners, rust removers, chemicals for swimming pools, and industrial drain cleaners damage tissue by coagulating cells and skin proteins, which can limit the depth of tissue damage. Organic compounds are found in chemical disinfectants and gasoline and cause damage because they are fat soluble and are easily absorbed through the skin. Once absorbed, they have toxic effects on the kidneys and liver.
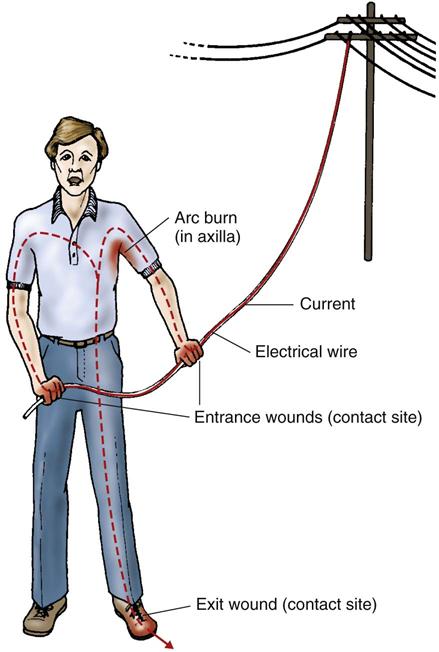
Electrical injuries are burns occurring when an electrical current enters the body (Fig. 28-9). These injuries have been called the “grand masquerader” of burns because the surface injuries may look small but the associated internal injuries can be huge. Tissue injury from electrical trauma results from electrical energy being converted to heat energy. The extent of injury depends on the type of current, the pathway of flow, the local tissue resistance, and the duration of contact. The skin is the most resistant organ; the greatest resistance is in the epidermis of the skin. At high voltages, the difference in tissue resistance is not important. Although various underlying tissues have different resistance to current flow, once skin resistance is overcome, the body acts as a conductor and current flows throughout the involved body part. Bone has a very high resistance because of its density. Current will flow along the surface of the bone, and the heat generated damages the attached muscle. As a result, deep muscle injury may be present even when superficial muscles appear normal or uninjured.
The longer the electricity is in contact with the body, the greater the damage. The duration of contact is increased by tetanic contractions of the strong flexor muscles in the forearm, which can prevent the person from releasing the electrical source.
It is difficult to know the exact path a current takes in the body. The course of flow is defined by the locations of the “contact sites,” which are the entrance and exit wounds (Fig. 28-10). At first, the wounds may not be obvious. The path of the injury may involve many internal organs between the two contact sites.
Burn injuries from electricity can occur in one of three ways: thermal burns, flash burns, or true electrical injury. Thermal burns occur when clothes ignite from heat or flames produced by electrical sparks. External burn injuries can occur when the electrical current jumps, or “arcs,” between two body surfaces. These injuries usually are severe and deep. True electrical injury occurs when direct contact is made with an electrical source. Internal damage results, and the injuries can be devastating. Damage starts on the inside and goes out; deep-tissue destruction may not be apparent immediately after injury. Organs in the path of the current may become ischemic and necrotic.
Radiation injuries occur when people are exposed to large doses of radioactive material. The most common type of tissue injury from radiation exposure occurs with therapeutic radiation. This injury is usually minor and rarely causes extensive skin damage.
Radiation exposure is more serious in industrial settings where radioactive energy is produced or radioactive isotopes are used. Injury severity depends on the type of radiation, distance from the source, duration of exposure, absorbed dose, and depth of penetration into the body. Chapter 24 discusses potential tissue damage from alpha, beta, and gamma radiation.
Incidence/Prevalence of Burn Injury
Fires and burns are the fifth most common cause of unintentional injury deaths in the United States and the third leading cause of fatal home injuries (American Burn Association, 2010). Although the number of fatalities and injuries caused by residential fires has declined gradually over the past several decades, many residential fire-related deaths remain preventable and continue to pose a significant public health problem.
An estimated 4000 fire and burn deaths occur each year from all sources of burn injury (American Burn Association, 2010). Most deaths occur at the scene of the incident or during transport.
The number of deaths from burn injuries decreases with appropriate intervention. Factors that increase the risk for death include age older than 60 years, a burn greater than 40% TBSA, and the presence of an inhalation injury. When a patient has all three of these factors, the risk for death is very high. Better outcomes from burn injuries occur because of vigorous fluid resuscitation, early burn wound excision, improved critical care monitoring, early enteral nutrition, antibiotics, and the use of specialized burn centers.
Health Promotion and Maintenance
Minor burns are common, and prevention involves planning and awareness. Teach all people to assess how hot the water is before bathing, showering, or immersing a body part in it. Hot water tanks should be set below 140° F. Reinforce the use of potholders when taking food from conventional or microwave ovens. Stress the importance of never adding a flammable substance (e.g., gasoline, kerosine, alcohol, lighter fluid, charcoal starter) to an open flame. Suggest the use of sunscreen agents and protective clothing to avoid sunburn.
House fires also are common and lead to severe burns and death. Teach people to reduce the risk for house fires by never smoking in bed, avoiding smoking when drinking alcohol or taking drugs that induce sleep, and keeping matches and lighters out of the reach of children or anyone who is cognitively impaired. If space heaters must be used, stress the importance of keeping clothing, bedding, and other flammable objects away from them. Remind people to keep the screens and doors closed on the fronts of fireplaces and to have chimneys swept each year to prevent creosote buildup. Also remind patients using home oxygen not to smoke or have open flames in a room where oxygen is in use (Edelman et al., 2008).
Leaving a burning building is critical to prevent injury or death. Teach all people to use home smoke detectors and carbon monoxide detectors and to ensure that the detectors are in good working order. The number of detectors needed depends on the size of the home. Recommendations are that each bedroom has a separate smoke detector, there should be at least one detector in the hallway of each story, and at least one detector is needed for the kitchen, each stairwell, and each home entrance. Teach everyone to develop a planned escape route with alternatives for when a main route is blocked by fire. Reinforce that no one should ever re-enter a burning building to retrieve belongings.
Resuscitation Phase of Burn Injury
Overview
Events within the first hour after injury can make the difference between life and death for the patient with a burn injury. Immediate care focuses on maintaining an open airway, ensuring adequate breathing and circulation, limiting the extent of injury, and maintaining the function of vital organs. Chart 28-1 outlines the emergency management of a burn injury.
The resuscitation phase is the first phase of a burn injury. It begins at the onset of injury and continues for about 24 to 48 hours. During this phase, the injury is evaluated and the immediate problems of fluid loss, edema, and reduced blood flow are assessed. The priorities for management during this period are to (1) secure the airway, (2) support circulation by fluid replacement, (3) keep the patient comfortable with analgesics, (4) prevent infection through careful wound care, (5) maintain body temperature, and (6) provide emotional support.
Patient-Centered Collaborative Care
Assessment
History
Knowledge of circumstances surrounding the burn injury is valuable in the management of a burn victim. If possible, obtain information directly from the patient. If this is not possible, ask family members or witnesses to the event. Ask about the circumstances of the injury, the time and place of injury, and the source and cause of injury. Asked detailed questions about how the burn occurred and the events occurring from the time of injury until help arrived. Also obtain demographic data, health history (including pre-existing illness), drug use, any additional injuries, and pain information (Brown-Guttovz, 2011).
Demographic data include age, weight, and height. The rate of serious complications and death from burn injuries is increased among adults older than 50 years. Chart 28-2 lists the age-related differences in older adults’ responses to a burn injury. The patient’s preburn weight is used to calculate fluid rates, energy requirements, and drug doses. This weight is the dry weight, because it represents the patient’s weight before edema begins to form. Calculations based on a weight obtained after fluid replacement is started are not accurate because of water-induced weight gain. Height is important in determining total body surface area (TBSA), which is used to calculate nutritional needs.
A health history, including any pre-existing illnesses, must be known for appropriate treatment. Obtain specific information about the patient’s history of cardiac or kidney problems, chronic alcoholism, substance abuse, and diabetes mellitus; any of these problems influence fluid resuscitation. The physiologic stress of a burn can make a mild disease process develop more symptoms or worsen an active process. Obtain a drug history that includes allergies, current drugs, and immunization status from the patient or family. Determine the dose and time the last drug was taken. Ask whether the patient smokes or drinks alcohol daily; these factors influence treatment and responses.
Other injuries may occur at the time of the burn. The most common causes of additional injuries are falls and motor vehicle crashes. Such injuries increase the risk for complications or death. Determine whether additional injuries such as fractures, chest injuries, and abdominal trauma are causing pain or discomfort.
Physical Assessment/Clinical Manifestations
Physical assessment findings in the resuscitation phase differ greatly from findings later in the course of the injury. Use a systematic approach to ensure that no problem is missed. Assessment of the respiratory system is most critical to prevent life-threatening complications.
Respiratory Assessment.
Patients with major burn injuries and those with inhalation injury are at risk for respiratory problems. Respiratory manifestations common with a burn injury are listed in Table 28-3. Thus continuous airway assessment is a nursing priority (Brown-Guttovz, 2011).
TABLE 28-3
FACTORS DETERMINING INHALATION INJURY OR AIRWAY OBSTRUCTION
Direct Airway Injury.
The degree of inhalation damage depends on the fire source, temperature, environment, and types of toxic gases generated. Ask about the source of the fire, duration of exposure, and whether the fire was in an enclosed space. Inspect the mouth, nose, and pharynx. Burns of the lips, face, ears, neck, eyelids, eyebrows, and eyelashes are strong indicators that an inhalation injury may be present. Burns inside the mouth and singed nasal hairs also indicate possible inhalation injury. Black particles of carbon in the nose, mouth, and sputum and edema of the nasal septum indicate smoke inhalation, as does a “smoky” smell to the patient’s breath.
A change in respiratory pattern may indicate a pulmonary injury. The patient may:
• Drool or have difficulty swallowing
• Produce sounds on exhalation that include audible wheezes, crowing, and stridor
Any of these changes may mean the patient is about to lose his or her airway.
Upper airway edema and inhalation injury are most common in the trachea and mainstem bronchi. Auscultation of these areas may reveal wheezes, which indicate partial obstruction. Patients with severe inhalation injuries may have such rapid obstruction that, within a short time, they cannot force air through the narrowed airways. As a result, the wheezing sounds disappear. This finding indicates impending airway obstruction and demands immediate intubation. Many patients are intubated when an inhalation injury is suspected rather than waiting until obstruction makes endotracheal or nasotracheal intubation difficult or impossible.
Carbon Monoxide Poisoning.
Carbon monoxide (CO) is one of the leading causes of death from a fire. It is a colorless, odorless, tasteless gas released in the process of combustion. Inhalation injury is a risk for carbon monoxide poisoning.
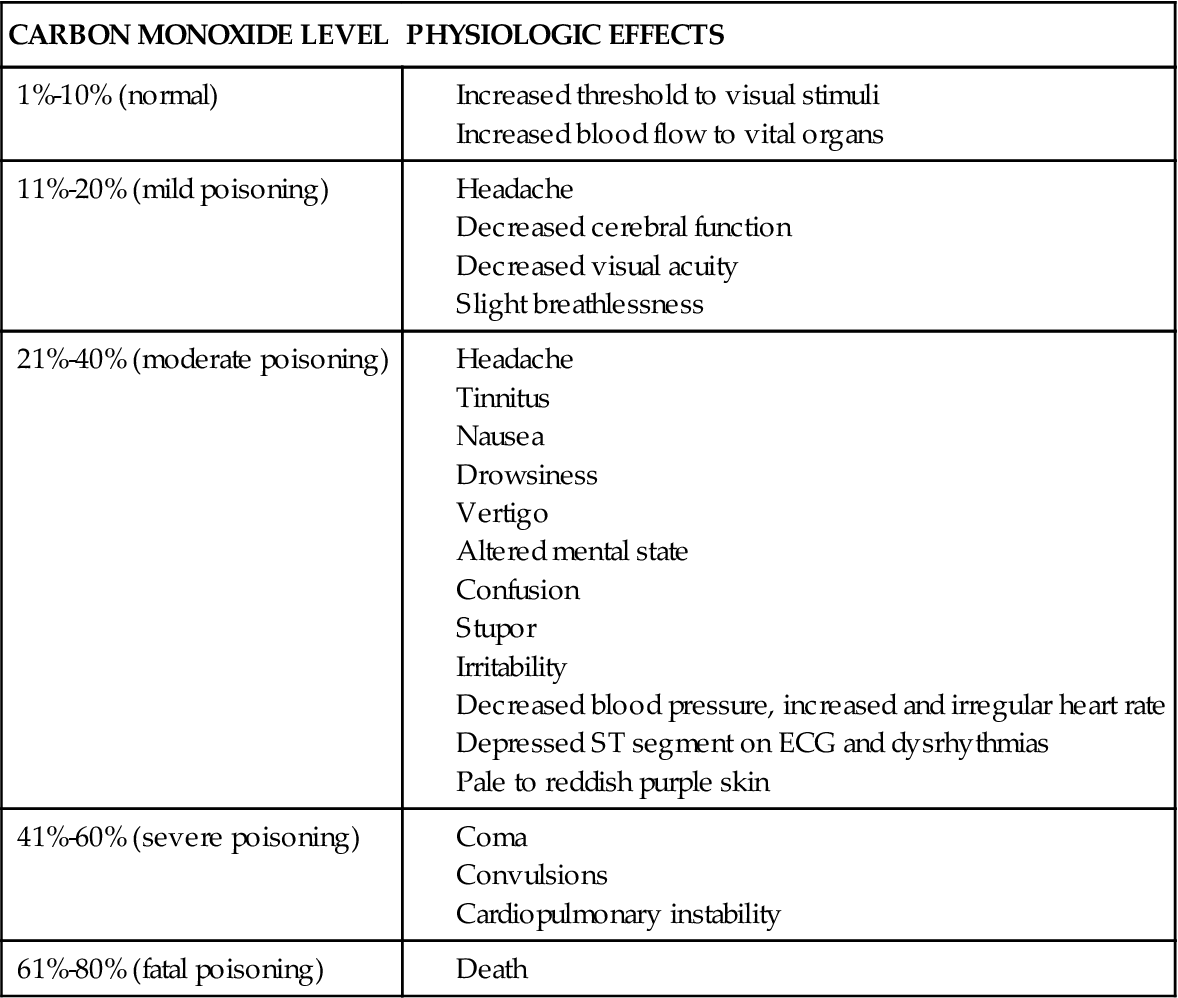
CO is rapidly transported across the lung membrane and binds tightly to hemoglobin in place of oxygen to form carboxyhemoglobin (CoHb). CO also causes the oxyhemoglobin dissociation curve to shift to the left, which impairs oxygen unloading at the tissue level. This shift results in reduced oxygen delivery because 98% of the oxygen supplied to the tissues comes bound to hemoglobin. Even though the oxygen-carrying capacity of the hemoglobin is reduced, the blood gas value of partial pressure of arterial oxygen (Pao2) is normal (Laing, 2010). The vasodilating action of carbon monoxide causes the “cherry red” color (or at least the absence of cyanosis) in these patients. Manifestations vary with the concentration of CoHb. Table 28-4 lists the effects of carbon monoxide poisoning.
TABLE 28-4
PHYSIOLOGIC EFFECTS OF CARBON MONOXIDE POISONING
| CARBON MONOXIDE LEVEL | PHYSIOLOGIC EFFECTS |
| 1%-10% (normal) | |
| 11%-20% (mild poisoning) | |
| 21%-40% (moderate poisoning) | |
| 41%-60% (severe poisoning) | |
| 61%-80% (fatal poisoning) |
Thermal (Heat) Injury.
Except for steam inhalation, aspiration of scalding liquid, or explosion of flammable gases under pressure, thermal burns to the respiratory tract are usually limited to the upper airway above the glottis (nasopharynx, oropharynx, and larynx). Heat damage of the pharynx is often severe enough to produce edema and upper airway obstruction, especially epiglottitis. The problem can occur any time during resuscitation. In the unresuscitated patient, supraglottic edema may be delayed because of the dehydration that occurs with hypovolemia. During fluid resuscitation, however, the tissues rehydrate and then swell. When it is known that the upper airways were exposed to heat, intubation may be performed as an early intervention before obstruction occurs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree