Donna D. Ignatavicius
Care of Male Patients with Reproductive Problems
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
7 Perform a focused physical assessment of the man’s reproductive system.
10 Incorporate complementary and alternative therapies into the patient’s plan of care.
11 Discuss treatment options for prostate cancer with patients, partners, and/or families.
12 Provide preoperative teaching for patients having a radical prostatectomy.
14 Identify adverse effects of radiation therapy for reproductive cancers.
15 Develop a community-based plan of care for a man with prostate cancer.
16 Describe the options for treating erectile dysfunction.
17 Discuss cultural considerations related to male reproductive problems.
18 Develop a plan of care for a patient with testicular cancer, including fertility issues.
19 Compare the assessment and treatment for hydrocele, spermatocele, and varicocele.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
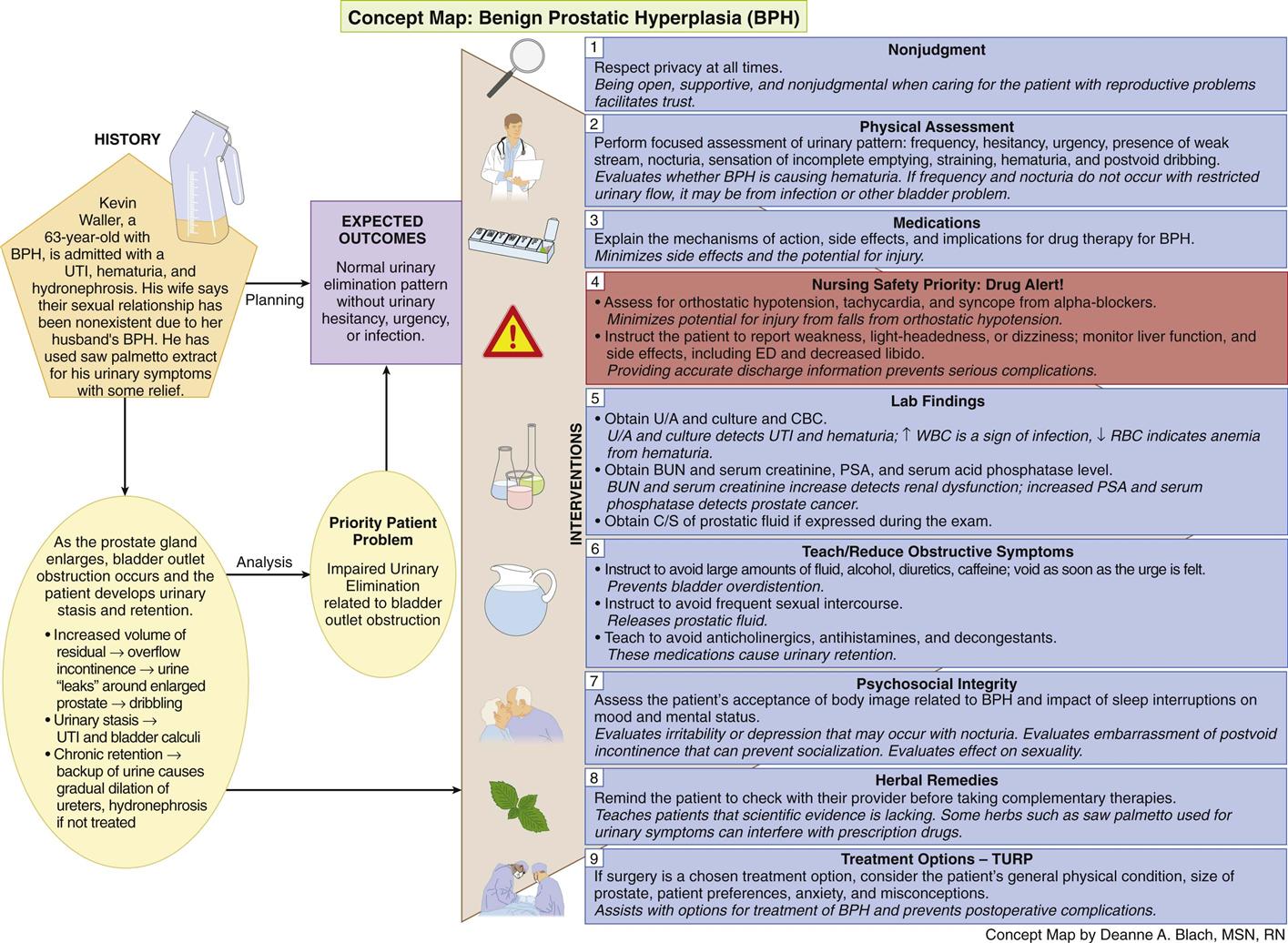
Concept Map: Benign Prostatic Hyperplasia (BPH)
Key Points
Review Questions for the NCLEX® Examination
Male reproductive problems can range from short-term infections to long-term health care problems that may require end-of-life care. Any health issue that affects the male reproductive system can affect the human need for sexuality. For example, some patients have surgeries that damage essential nerves that are needed to have an erection. Others have disorders that psychologically prevent the patient from engaging in his usual sexual activity.
The role of the nurse and other health care team members is to be open, supportive, and nonjudgmental when caring for men with reproductive problems. Respect the man’s privacy at all times.
Benign Prostatic Hyperplasia
Pathophysiology
Benign prostatic hyperplasia (BPH) is a very common health problem, but the exact cause is unclear. It is likely the result of a combination of aging and the influence of androgens that are present in prostate tissue, such as dihydrotestosterone (DHT) (McCance et al., 2010). With aging and increased DHT levels, the glandular units in the prostate undergo nodular tissue hyperplasia (an increase in the number of cells). This altered tissue promotes local inflammation by attracting cytokines and other substances (McCance et al., 2010).
As the prostate gland enlarges, it extends upward into the bladder and inward, causing bladder outlet obstruction (Fig. 75-1). In response, the urinary system is affected in several ways. First, the detrusor (bladder) muscle thickens to help urine push past the enlarged prostate gland (McCance et al., 2010). In spite of the bladder muscle change, the patient has increased residual urine (stasis) and chronic urinary retention. The increased volume of residual urine often causes overflow urinary incontinence, in which the urine “leaks” around the enlarged prostate causing dribbling. Urinary stasis can also result in urinary tract infections and bladder calculi (stones).
In a few patients, the prostate becomes very large and the man cannot void (acute urinary retention [AUR]). The patient with this problem requires emergent care. In other patients, chronic urinary retention may result in a backup of urine and cause a gradual dilation of the ureters (hydroureter) and kidneys (hydronephrosis) if BPH is not treated. These problems can lead to chronic kidney disease as described in Chapter 71.
Patient-Centered Collaborative Care
Assessment
History
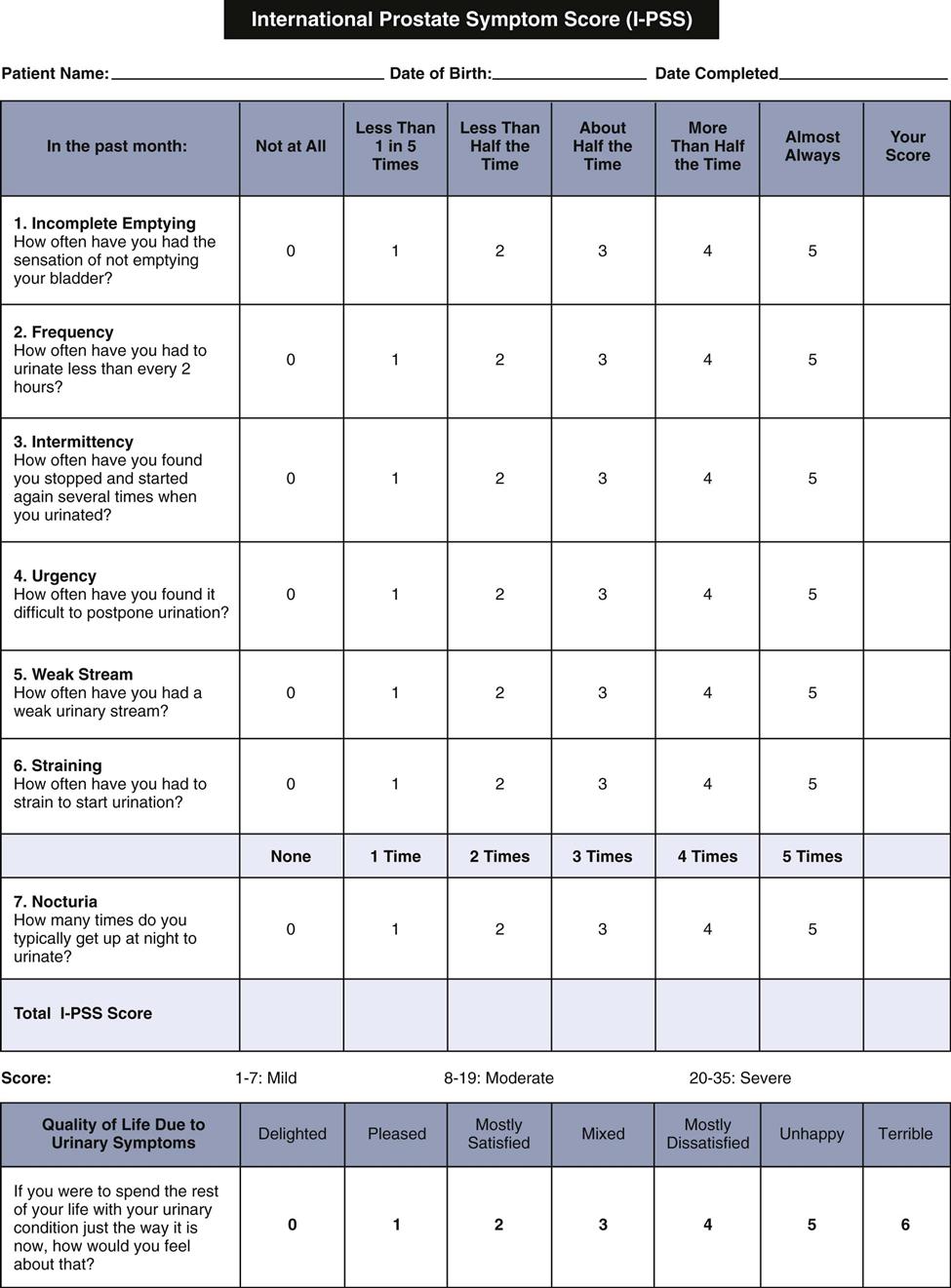
When taking a history, several standardized assessment tools are used to help the health care provider determine the severity of lower urinary tract symptoms (LUTS) associated with prostatic enlargement. One of the most commonly used assessments is the International Prostate Symptom Score (I-PSS), which incorporates the American Urological Association Symptom Index (AUA-SI) (Fig. 75-2) as questions 1 through 7. The additional question included on the I-PSS is the effect of the patient’s urinary symptoms on quality of life. Most patients complete the questions as a self-administered tool because it is available in many languages. If the patient is illiterate or does not feel like reading the questions, the nurse or health care provider can ask them. Be sure that older men wear their glasses or contact lenses, if needed.
Physical Assessment/Clinical Manifestations
Ask about the patient’s current urinary pattern. Assess for urinary frequency and urgency. Determine the number of times the patient awakens during the night to void (nocturia). Other symptoms of LUTS include:
• Difficulty in starting (hesitancy) and continuing urination
• Reduced force and size of the urinary stream (“weak” stream)
• Sensation of incomplete bladder emptying
• Straining to begin urination
If frequency and nocturia do not occur with restricted urinary flow, the patient may have an infection or other bladder problem. Ask whether the patient has had hematuria (blood in the urine) when starting the urine stream or at the end of voiding. BPH is a common cause of hematuria in older men.
The advanced practice nurse or other health care provider examines the patient for physical changes of the prostate gland. Remind the patient to void before the physical examination. Inspect and palpate the abdomen for a distended bladder. The health care provider may percuss the bladder. If the patient has a sense of urgency when gentle pressure is applied, the bladder may be distended. Obese patients are best assessed by percussion or bedside ultrasound bladder scanner rather than by inspection or palpation.
Prepare the patient for the prostate gland examination. Tell him that he may feel the urge to urinate as the prostate is palpated. Because the prostate is close to the rectal wall, it is easily examined by digital rectal examination (DRE). Help the patient bend over the examination table or assume a side-lying fetal position, whichever is the easiest position for him. The health care provider examines the prostate for size and consistency. BPH presents as a uniform, elastic, nontender enlargement, whereas cancer of the prostate gland feels like a stony-hard nodule. Advise the patient that after the prostate gland is palpated, it may be massaged to obtain a fluid sample for examination to rule out prostatitis (inflammation and possible infection of the prostate), a common problem that can occur with BPH. If the patient has bacterial prostatitis, he is treated with broad-spectrum antibiotic therapy for at least 30 days to prevent the spread of infection (McCance et al., 2010).
Psychosocial Assessment
Patients who have nocturia and other LUTS may be irritable or depressed as a result of interrupted sleep and annoying visits to the bathroom. Assess the effect of sleep interruptions on the patient’s mood and mental status.
Post-void dribbling and overflow incontinence may cause embarrassment and prevent the patient from socializing or leaving his home. For some patients, this social isolation can affect quality of life and lead to clinical depression and/or severe anxiety. Johnson et al. (2010) found a strong correlation between depression and BPH in older men. Depressed patients were three times more likely to have severe symptoms.
Laboratory Assessment
A urinalysis and culture are typically obtained to diagnose urinary tract infection and microscopic hematuria. If infection is present, the urinalysis measures the number of white blood cells (WBCs).
Other laboratory studies that may be performed include:
Other Diagnostic Assessment
Imaging studies that are typically performed are transabdominal ultrasound and transrectal ultrasound (TRUS). The patient having a TRUS lies on his side while the transducer is inserted into the rectum for viewing the prostate and surrounding structures. A tissue biopsy may also be done if the health care provider is uncertain whether the prostatic problem is benign or malignant.
In some cases, the physician uses a cystoscope to view the interior of the bladder, the bladder neck, and the urethra. This examination is used to study the presence and effect of bladder neck obstruction. The procedure is usually done in an ambulatory care setting. See Chapter 69 for a detailed description of cystoscopy and the nursing care needed for patients having this procedure.
Residual urine may be determined by bladder ultrasound immediately after the patient voids. As an alternative, because the patient voids before cystoscopy, residual urine may be measured when the cystoscope is inserted. Urodynamic pressure-flow studies may help diagnose and grade bladder outlet obstruction and detrusor muscle function.
Analysis
The priority problem for the patient with benign prostatic hyperplasia (BPH) is Impaired Urinary Elimination related to bladder outlet obstruction.
Planning and Implementation
Improving Urinary Elimination
Planning: Expected Outcomes.
The patient with BPH is expected to have a normal urinary elimination pattern without urinary hesitancy, urgency, or infection.
Interventions.
Patients with symptomatic BPH are first treated with nonsurgical interventions, such as drug therapy. The Concept Map on p. 1634 shows nursing assessment and collaborative interventions for the patient with BPH.
Nonsurgical Management.
Drug therapy is a popular option for treating BPH. For patients with AUR or for those who do not respond or cannot tolerate drug therapy, noninvasive procedures or surgery is the treatment of choice.
Drug Therapy.
Drugs from two major categories may be used alone, but most commonly they are given in combination. The health care provider usually prescribes a 5-alpha reductase inhibitor (5-ARI) as first-line drug therapy. Examples of these drugs are finasteride (Proscar) and dutasteride (Avodart). Normally, testosterone is converted to DHT in the prostate gland by the enzyme 5-alpha reductase. By taking an enzyme-inhibiting agent, the patient’s DHT levels decrease, which results in reducing the enlarged prostate.
The alpha-adrenergic receptors in prostatic smooth muscle enable the prostate gland to respond to alpha-1 selective blocking agents, such as tamsulosin (Flomax), alfuzosin (Uroxatral), doxazosin (Cardura, Cardura-1 ![]() ), terazosin (Hytrin), and silodosin (Rapaflo). Tamsulosin is also available as an over-the-counter (OTC) drug. These drugs relax smooth muscles in the prostate gland, creating less urinary resistance and improved urinary flow. They also cause peripheral vasodilation and reduced peripheral vascular resistance.
), terazosin (Hytrin), and silodosin (Rapaflo). Tamsulosin is also available as an over-the-counter (OTC) drug. These drugs relax smooth muscles in the prostate gland, creating less urinary resistance and improved urinary flow. They also cause peripheral vasodilation and reduced peripheral vascular resistance.
The most effective drug therapy approach for many patients is a combination of a 5-ARI drug and an alpha-1 selective blocking agent. A commonly prescribed drug regimen is finasteride and doxazosin. Newer drugs, such as Jalyn, provide a combination of dutasteride and tamsulosin in a once-a-day capsule.
Other drugs may be helpful in managing specific urinary symptoms. For example, low-dose oral desmopressin, a synthetic antidiuretic analog, has been used successfully for nocturia (Wang et al., 2011). Drugs being tested for their effectiveness in treating BPH include bisphosphonates, ezetimibe (Zetia), Botox, and Nymox.
Complementary and Alternative Therapies.
Although many men use Serenoa repens (saw palmetto extract), a plant extract, to help manage the urinary symptoms associated with BPH, studies on the effectiveness of this herb have not shown that it is effective (Tackland et al., 2009). Teach patients who want to try these herbs and other natural substances that scientific evidence to prove they are useful is lacking. However, if they choose to take them, remind them to check with their health care provider before taking any OTC natural substance. Some herbs interfere with prescription drugs the patient may be taking for other health problems. Side effects, such as abdominal pain, nausea, and vomiting, are mild, reversible, and infrequent (Agbabiaka et al., 2009).
Other Nonsurgical Interventions.
Other interventions that may reduce obstructive symptoms include those that cause the release of prostatic fluid such as frequent sexual intercourse. This approach is helpful for the man whose obstructive symptoms result from an enlarged prostate with a large amount of retained prostatic fluid.
Teach patients with BPH to avoid drinking large amounts of fluid in a short time; to avoid alcohol, diuretics, and caffeine; and to void as soon as they feel the urge. These measures are aimed at preventing overdistention of the bladder, which may result in loss of detrusor muscle tone. Teach patients to avoid any drugs that can cause urinary retention, especially anticholinergics, antihistamines, and decongestants. Emphasize the importance of telling any health care provider about the diagnosis of BPH so that these drugs are not prescribed.
If drug therapy or other measures are not helpful in relieving urinary symptoms, several noninvasive techniques are available to destroy excess prostate tissue using a variety of heat methods (thermotherapy). These procedures are often done in a physician’s office or another ambulatory care setting. Examples include:
• Transurethral needle ablation (TUNA) (low radiofrequency energy shrinks the prostate)
• Transurethral microwave therapy (TUMT) (high temperatures heat and destroy excess tissue)
Prostatic stents may be placed into the urethra to maintain permanent patency after a procedure for destroying or removing prostatic tissue. All of these highly technical treatments use local or regional anesthesia and do not require an indwelling urinary catheter. They are also associated with less risk for complications such as intraoperative bleeding and erectile dysfunction when compared with traditional surgical approaches. Patients can return to their usual activities in a day or two.
Surgical Management.
For patients who are not candidates for nonsurgical management or do not want to take drugs or have other treatment options, surgery may be performed. The gold standard continues to be a transurethral resection of the prostate (TURP) in which the enlarged portion of the prostate is removed through an endoscopic instrument. The newer holmium laser enucleation of the prostate (HoLEP) procedure is a minimally invasive surgical technique that is gaining popularity. For a few men, an open prostatectomy (entire prostate removal) may be performed (see discussion of Surgical Management on p. 1639 in the Prostate Cancer section). Some or all of these criteria indicate the need for surgery:
• Acute urinary retention (AUR)
• Chronic urinary tract infections secondary to residual urine in the bladder
Preoperative Care.
When planning surgical interventions, the patient’s general physical condition, the size of the prostate gland, and the man’s preferences are considered. The patient may have many fears and misconceptions about prostate surgery, such as believing that automatic loss of sexual functioning or permanent incontinence will occur. Assess the patient’s anxiety, correct any misconceptions about the surgery, and provide accurate information to him and his family. Regardless of the type of surgery to be performed, provide information about anesthesia (see Chapter 17). The patient may have other medical problems that increase the risk for complications of general anesthesia and may be advised to have regional anesthesia. Epidural and spinal anesthesia are the most common types of anesthesia used for a TURP. Because the patient is awake, it is easier to assess for hyponatremia (low serum sodium), fluid overload, and water intoxication, which can result from large bladder irrigations.
After a TURP, all patients have an indwelling urethral catheter for at least a day. Be sure that they know that they will feel the urge to void while the catheter is in place. Tell the patient that he will likely have traction on the catheter that may cause discomfort. However, reassure him that analgesics will be prescribed to relieve his pain. Explain that it is normal for the urine to be blood-tinged after surgery. Small blood clots and tissue debris may pass while the catheter is in place and immediately after it is removed.
Operative Procedures.
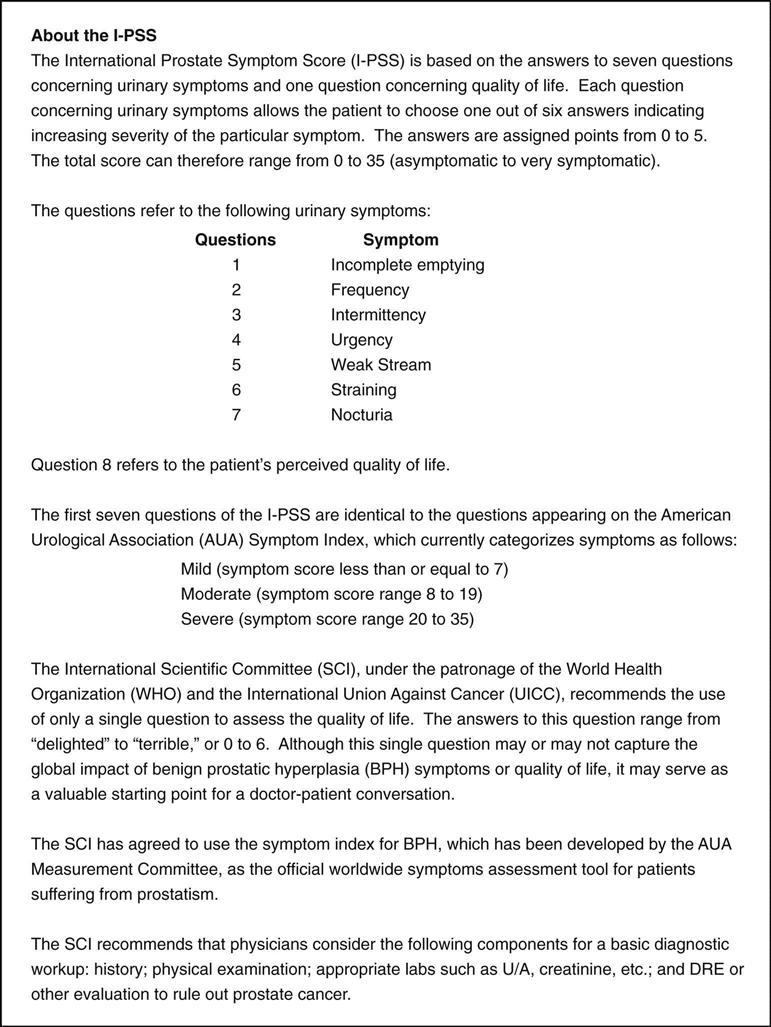
The traditional TURP is a “closed” surgery. To perform the procedure, the surgeon inserts a resectoscope (an instrument similar to a cystoscope, but with a cutting and cauterizing loop) through the urethra (Fig. 75-3). The enlarged portion of the prostate gland is then removed in small pieces (prostate chips). A similar procedure is the transurethral incision of the prostate (TUIP), in which small cuts are made into the prostate to relieve pressure on the urethra. This alternate technique is used for smaller prostates. To prevent bleeding and excess clotting, a fibrinolytic inhibitor like tranexamic acid (Cyklokapron) may be used during surgery.
The disadvantage of a TURP is that, because only small pieces of the gland are removed, remaining prostate tissue may continue to grow and cause urinary obstruction, requiring additional TURPs. Also, urethral trauma from the resectoscope with resulting urethral strictures is possible.
In many large medical centers around the world, specialists can perform newer surgical treatments, such as the holmium laser enucleation of the prostate (HoLEP) (Eltabey et al., 2010). For this procedure, the surgeon uses the laser to remove the obstructive prostatic tissue and push it into the bladder for removal and seals all blood vessels. Very little blood is lost during the short procedure and is therefore safe for patients taking anticoagulants.
Postoperative Care.
After both the TURP and HoLEP procedures, a urinary catheter is placed into the bladder. Traction is often applied on the catheter for the patient having a TURP by pulling it taut and taping it to the patient’s abdomen or thigh. If the catheter is taped to the patient’s thigh, instruct him to keep his leg straight. The patient having the HoLEP procedure has a urinary catheter overnight, but the patient with a TURP has a catheter in place for several days. In some cases, the patient is discharged with the catheter in place.
Remind the patient that because of the urinary catheter’s large diameter and the pressure of the retention balloon on the internal sphincter of the bladder, he will feel the urge to void continuously. This is a normal sensation, not a surgical complication. Advise the patient not to try to void around the catheter, which causes the bladder muscles to contract and may result in painful spasms. Chart 75-1 summarizes the nursing care for patients having a TURP.
When the urinary catheter is removed, the patient may experience burning on urination and some urinary frequency, dribbling, and leakage. Reassure him that these symptoms are normal and will decrease. The patient may also pass small clots and tissue debris for several days after the TURP. Instruct him to increase fluid intake to at least 2000 to 2500 mL daily, which helps decrease dysuria and keep the urine clear. An older patient who has renal disease or who is at risk for heart failure may not be able to tolerate this much fluid. By the time of discharge (usually 2 to 3 days after surgery), he should be voiding 150 to 200 mL of clear yellow urine every 3 to 4 hours. By discharge, pain is minimal and analgesics may not be required.
Observe for other possible but uncommon complications of TURP, such as infection and incontinence. Teach the patient that sexual function should not be affected after surgery but that retrograde ejaculation is possible. In this case, most of the semen flows backwards into the bladder so only a small amount will be ejaculated from the penis.
Community-Based Care
The patient with benign prostatic hyperplasia (BPH) is typically managed at home. Patients who have surgery are also discharged to their home or other setting from where they were admitted. Some patients, especially those who have had a TURP, may have temporary loss of control of urination or a dribbling of the urine. Reassure the patient that these symptoms are almost always temporary and will resolve. Assist the patient and his family in finding ways to keep his clothing dry until sphincter control returns. Instruct him to contract and relax his sphincter frequently to re-establish urinary control (Kegel exercises). External urinary (condom) catheters are not used except in extreme cases because they may give the patient a false sense of security and delay urinary control.
Patients having the HoLEP procedure typically stay in the hospital overnight and usually have no urinary symptoms after surgery. This procedure may soon replace the TURP as the gold standard for surgical management of the patient with BPH.
Prostate Cancer
Pathophysiology
Prostate cancer is one of the most common types of cancer in men in the world. Men older than 65 years have the greatest risk for the disease. In the United States, it affects African-American men more commonly than Euro-American men and at an earlier age. The exact cause for this difference is not known.
Testosterone and dihydrotestosterone (DHT) are the major androgens (male hormones) in the adult male. Testosterone is produced by the testis and circulates in the blood. DHT is a testosterone derivative in the prostate gland. In some patients, the prostate grows very rapidly, leading to noncancerous high-grade prostatic intraepithelial neoplasia (PIN). Patients with PIN are at a higher risk for developing prostate cancer than men who do not have that growth pattern.
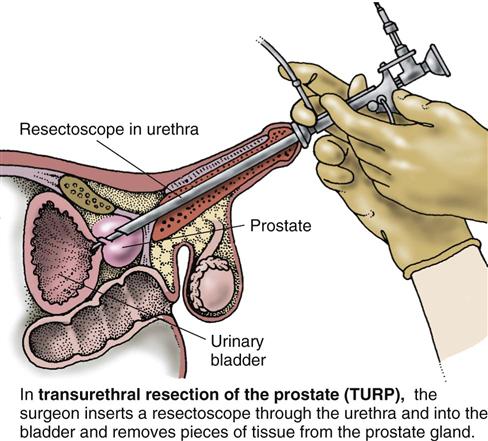
Many prostate tumors are androgen sensitive (McCance et al., 2010). Most are adenocarcinomas and arise from epithelial cells located in the posterior lobe or outer portion of the gland (Fig. 75-4).
Of all malignancies, prostate cancer is one of the slowest growing, and it metastasizes (spreads) in a predictable pattern. Common sites of metastasis are the nearby lymph nodes, bones, lungs, and liver (McCance et al., 2010). The bones of the pelvis, sacrum, and lumbar spine are most often affected. Chapter 23 describes staging categories of localized and advanced cancers.
Prostate cancer is likely caused by a number of factors, including androgens. Dietary factors, such as eating a diet high in animal fat (e.g., red meat) and complex carbohydrates or having a low fiber intake, increase the risk for prostate cancer. Men who have had a vasectomy or those who were exposed to environmental toxins, such as arsenic, may also be at increased risk for the disease (Held-Warmkessel, 2008; McCance et al., 2010).
Health Promotion and Maintenance
Teach men about the most recent American Cancer Society (ACS) guidelines for prostate cancer screening and early detection (ACS, 2011). The current recommendations are that men should make an informed decision about whether to have prostate cancer screening. Starting at the age of 50, men should discuss the options of having prostate-specific antigen testing with their health care provider. Men at a higher risk for prostate cancer, including African Americans or men who have a first-degree relative with prostate cancer before the age of 65, should have this discussion at age 45. Men who have multiple first-degree relatives with prostate cancer at an early age should discuss screening at age 40.
Although a family history of prostate cancer cannot be changed, certain nutritional habits can be altered to possibly decrease the risk for the disease. First, teach men to eat a healthy, balanced diet, including decreasing animal fat (e.g., red meat). Instead of red meat, remind them to eat more fish and other foods high in omega-3 fatty acids because they are thought to be helpful in preventing cancer. Also reinforce the need to increase fruits, vegetables, soy, and high-fiber foods.
Patient-Centered Collaborative Care
Assessment
History
Assess the patient’s age, race/ethnicity, and family history of prostate cancer. Ask about his nutritional habits, especially focusing on the intake of red meat, fish, and fruits and vegetables. Assess whether the patient has any problems with urination. Take a drug history to determine if he is taking any medication that could affect voiding. The first symptoms that the man may report are related to bladder outlet obstruction, such as difficulty in starting urination, frequent bladder infections, and urinary retention. Ask about urinary frequency, hematuria (blood in the urine), and nocturia (voiding during the night). Ask if he has had any pain during intercourse, especially when ejaculating. Inquire if the patient has had or currently has any other pain (particularly bone pain), a symptom associated with advanced prostate cancer. Ask him if he has had any recent unexpected weight loss.
Take a sexual history for recent changes in desire or function. Ask about current or previous sexually transmitted diseases, penile discharge, or scrotal pain or swelling.
Physical Assessment/Clinical Manifestations
Most early cancers are diagnosed while the patient is having a routine physical examination or is being treated for benign prostatic hyperplasia (BPH). Gross blood in the urine (hematuria) is a common clinical manifestation of late prostate cancer. Assess for pain in the pelvis, spine, hips, or ribs. Complete a thorough pain assessment. Palpate for swollen lymph nodes, especially in the groin areas. Pain and swollen nodes also indicate advanced disease that has spread. Take and record the patient’s weight because unexpected weight loss is also common when the disease is advanced.
Prepare the patient for a digital rectal examination (DRE). On rectal examination, a prostate that is found to be stony hard and with palpable irregularities or indurations is suspected to be malignant.
Psychosocial Assessment
A diagnosis of any type of cancer causes fear and anxiety for most people. Some men, particularly African Americans, develop the disease in their 40s and 50s when they are perhaps planning their retirements, putting their children through college, and/or enjoying their middle years. Assess the reaction of the patient to the diagnosis, and observe how his family reacts to the illness. Men may describe their feelings as shock, fear, anger, and “roller coaster” (Wallace & Storms, 2007). Expect that patients will go through the grieving process and may be in denial or depressed. Determine what support systems they have, such as spiritual leaders or community group support, to help them through diagnosis, treatment, and recovery.
One of the biggest concerns for the man may be his ability for sexual function after cancer treatment. Tell him that function will depend on the type of treatment he has. Most surgical techniques used today do not involve cutting the perineal nerves that are needed for an erection. A dry climax may occur if the prostate is removed because it produces most of the fluid in the ejaculate. Refer the patient to his surgeon (urologist), sex therapist, or intimacy counselor if available.
Laboratory Assessment
Prostate-specific antigen (PSA) is a glycoprotein produced by the prostate. PSA analysis is used as a screening test for prostate cancer. If the test is performed, it should be drawn before the DRE because the examination can cause an increase in PSA due to prostate irritation.
The normal blood level of PSA in men younger than 50 years is less than 2.5 ng/mL. PSA levels increase to as high as 6.5 ng/mL when men reach their 70s. African-American men have a slighter higher normal value, but the reason for this difference is not known. Because other prostate problems also increase the PSA level, it is not specifically diagnostic for cancer. The level associated with prostate cancer, however, is usually much higher than those occurring with problems such as prostatitis and benign prostatic hyperplasia (Pagana & Pagana, 2010).
An elevated PSA level should decrease a few days after a prostatectomy for cancer. An increase in the PSA level several weeks after surgery usually indicates that the disease has recurred.
Because PSA is not absolutely specific to prostate cancer, another test, early prostate cancer antigen (EPCA-2), may be a serum marker for prostate cancer. It can detect changes in the prostate gland early and is a very sensitive test. EPCA-2 may also eliminate the need to perform a biopsy of prostate tissue.
Other Diagnostic Assessment
After assessments by DRE and PSA, most patients have a transrectal ultrasound (TRUS) of the prostate in an ambulatory care or imaging setting. The practitioner inserts a small probe into the rectum and obtains a view of the prostate using sound waves. If prostate cancer is suspected, a biopsy is usually performed to obtain an accurate diagnosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree