Robin Chard
Care of Intraoperative Patients
Learning Outcomes
Safe and Effective Care Environment
1 Use appropriate patient identifiers when administering drugs or marking surgical sites.
2 Verify that the patient has given informed consent for the surgical procedure.
3 Examine individual patient factors for potential threats to safety, especially for older adults.
4 Differentiate the roles and responsibilities of intraoperative personnel.
6 Explain correct technique to apply and remove surgical attire.
7 Understand the nurse’s role in monitoring all OR personnel for possible breaks in sterile technique.
Psychosocial Integrity
Physiological Integrity
12 Assess patients for specific problems related to positioning during surgical procedures.
14 Coordinate appropriate care for the patient with malignant hyperthermia.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
The intraoperative period begins when the patient enters the surgical suite and ends at the time of transfer to the postanesthesia recovery area, same-day surgery unit, or the intensive care unit. The main concerns of perioperative nurses are the safety and advocacy for the patient during surgery. Nursing observations and actions can prevent, reduce, control, and manage many hazards. Once in the operating room (OR), the patient is at risk for infection, impaired skin integrity, increased anxiety, altered body temperature, and injury related to positioning and other hazards. The surgical phase is filled with unfamiliar experiences and uncertain outcomes. Nursing care during this period is critical because the patient’s physical needs, spiritual needs, comfort, safety, dignity, and psychological status depend on the perioperative nurse. Specific procedures and policies may differ among agencies but should all reflect the perioperative standards and recommended practices as published by the Association of periOperative Registered Nurses (AORN) (2010a). Perioperative nurses practice within a specific, patient-focused model that incorporates professional practice with attainable, measurable outcomes.
Overview
Members of the Surgical Team
The surgical team consists of the surgeon, one or more surgical assistants, the anesthesia provider, and the OR nursing staff. Perioperative, or OR, nurses include the holding area nurse, circulating nurse, scrub nurse or a non-nurse “scrub person,” and specialty nurse. The number of assistants, circulating nurses, and scrub nurses depends on the complexity and projected length of the surgical procedure. For some minor procedures, only a circulating nurse and scrub person may be needed in addition to the surgeon. More complex procedures may require additional nursing staff to either circulate or scrub.
Surgeon and Surgical Assistant
The surgeon is a physician who assumes responsibility for the surgical procedure and any surgical judgments about the patient. The surgical assistant might be another surgeon (or physician, such as a resident or intern) or an advanced practice nurse, physician assistant, certified registered nurse first assistant (CRNFA), or surgical technologist. Under the direction of the surgeon and within the legal scope of practice for each state, the assistant may hold retractors, suction the wound (to improve viewing of the operative site), cut tissue, suture, and dress wounds.
Anesthesia Providers
The anesthesiologist is a physician who specializes in giving anesthetic agents. A certified registered nurse anesthetist (CRNA) is a registered nurse with additional education and credentials who delivers anesthetic agents under the supervision of an anesthesiologist, surgeon, dentist, or podiatrist. The anesthesia provider gives anesthetic drugs to induce and maintain anesthesia and delivers other drugs as needed to support the patient during surgery.
The anesthesia provider monitors the patient during surgery by assessing and monitoring:
Depending on the patient’s needs, anesthesia personnel give IV fluids, including blood and blood products.
Perioperative Nursing Staff
Perioperative, or OR, staff have several roles during surgery, depending on their education, experience, skill, and job responsibilities. Regardless of their role, the OR nurse uses clinical decision-making skills, develops a plan of nursing care, and coordinates care delivery to patients and their family members.
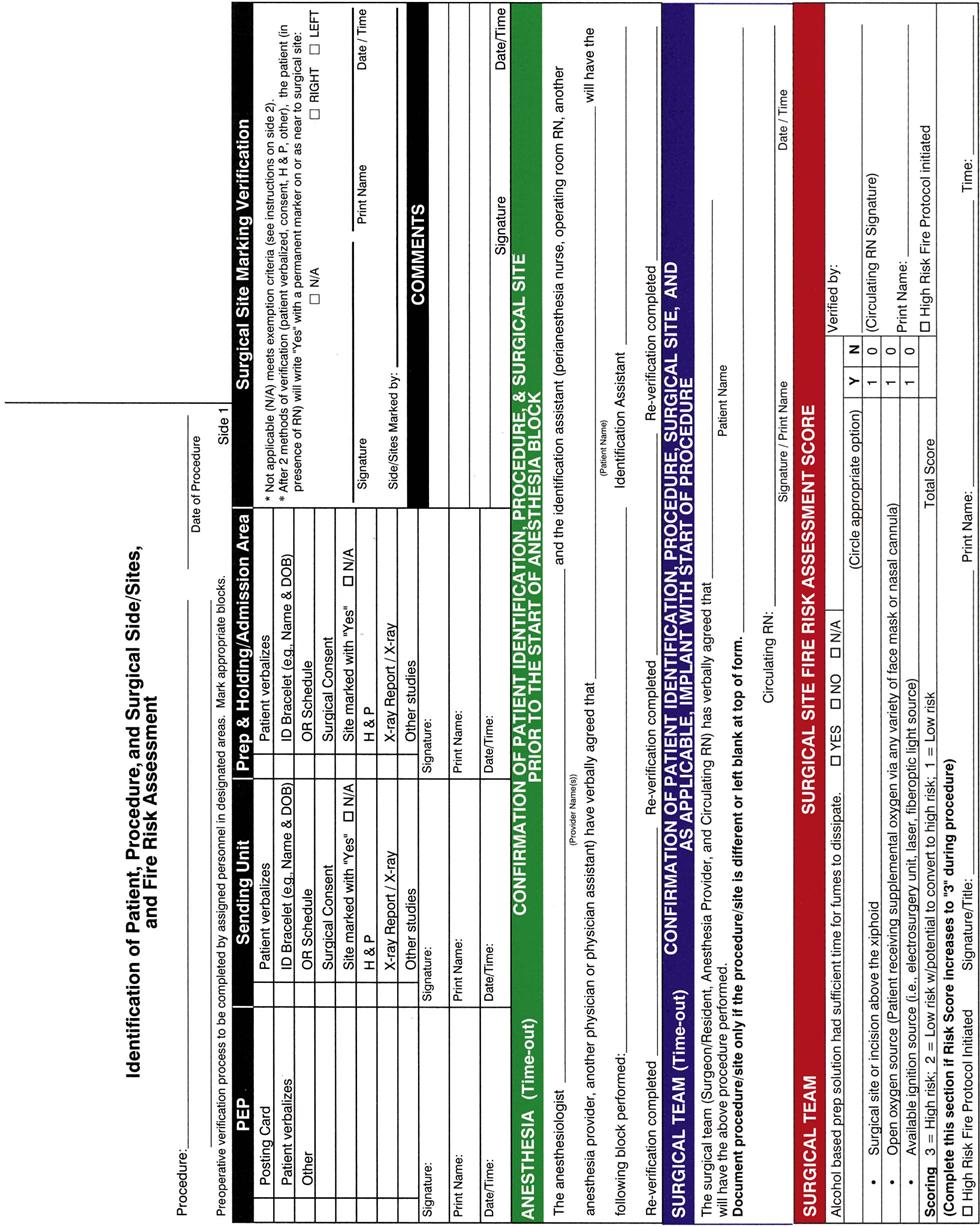
Holding area nurses work in those operating suites that have a presurgical holding area next to the main ORs. The patient waits in this area until the OR is ready. The holding area nurse coordinates and manages the care while the patient is in this area. Responsibilities include greeting the patient on arrival, reviewing the medical record and preoperative checklist, verifying that the operative consent forms are signed, and documenting the risk assessment (Fig. 17-1). This nurse also assesses the patient’s physical and emotional status, gives emotional support, answers questions, and provides additional education as needed.
The holding area is busy, with many staff members performing different procedures before surgery (e.g., starting IV lines, inserting epidural catheters). The holding area nurse promotes an atmosphere of comfort, privacy, and confidentiality. Depending on the facility’s policy, family members may wait with the patient.
Circulating nurses or “circulators” are registered nurses who coordinate, oversee, and are involved in the patient’s nursing care in the OR. The circulating nurse’s actions are vital to the smooth flow of events before, during, and after surgery. He or she is responsible for coordinating all activities within that particular OR. The circulator sets up the OR and ensures that supplies, including blood products and diagnostic support, are available as needed. All anticipated equipment is gathered and inspected by the circulator to make certain that it is safe and functional before the surgery. Depending on the procedure and position required, the circulator makes up the operating bed (OR table) with gel pads (to prevent pressure ulcers), safety straps and armboards (for patient positioning), and either heating pads under the sheets or disposable warming blankets placed over the patient as indicated (to prevent hypothermia) (Weirich, 2008).
If there is no holding area nurse, the circulator assumes the responsibilities of that nursing role as well. Even when there is a holding area nurse, The Joint Commission’s National Patient Safety Goals (NPSGs) require that the circulator also greets the patient and reviews findings with the holding area nurse.
Once the patient is ready to be moved into the OR, the circulating nurse, along with the OR team, assists the patient in transferring to the operating bed. The nurse positions the patient, protecting bony areas with extra padding while providing comfort and reassurance. While observing the patient, the circulating nurse also assists the anesthesia provider with the induction of anesthesia by positioning the patient and applying cricoid pressure, when requested. The circulator then may assist with additional positioning, insert a Foley catheter if needed, apply the grounding pad, test equipment, and “prep” (scrub) the surgical site before the patient is draped with sterile drapes.
Throughout the surgery, the circulating nurse:
• Protects the patient’s privacy
• Ensures the patient’s safety
• Monitors traffic in the room
• Assesses the amount of urine and blood loss
• Reports findings to the surgeon and anesthesia provider
• Ensures that the surgical team maintain sterile technique and a sterile field
• Anticipates the patient’s and surgical team’s needs, providing supplies and equipment
Depending on facility policy, the circulating nurse may record drugs, blood, and blood components given. (This also may be a function of the anesthesia provider.)
Before the procedure is over, the circulating nurse completes documentation in the OR and nursing records, including the presence of drains or catheters, the length of the surgery, and a count of all sponges, “sharps” (needles, blades), and instruments. He or she notifies the postanesthesia care unit (PACU) of the patient’s estimated time of arrival and any special needs.
Scrub nurses or scrub persons set up the sterile table (Fig. 17-2), drape the patient, and hand sterile supplies, sterile equipment, and instruments to the surgeon and the assistant. Knowledge of the surgical procedure allows the scrub person to anticipate which instruments and types of sutures the surgeon will need. Anticipating these needs reduces the duration of anesthesia for the patient. In addition, the surgeon’s anxiety and tension are reduced when the scrub nurse or person is familiar with the procedure and can anticipate and respond accordingly. Throughout the surgical procedure, the scrub person (with the circulating nurse) maintains an accurate count of sponges, sharps, and instruments and amounts of irrigation fluid and drugs used.

A specially trained person who is not a nurse may perform the scrub role. Such people are called operating room technicians (ORTs) or surgical technologists. Often certified surgical technologists (CSTs) are used in the OR.
Specialty nurses may be in charge of a particular type of surgical specialty (e.g., orthopedic, cardiac, ophthalmologic) and are responsible for nursing care specific to patients needing that type of surgery. The specialty nurse assesses, maintains, and recommends equipment, instruments, and supplies used in that specialty.
If the facility uses laser technology, a nurse specially trained in the use, care, and maintenance of the laser is needed. He or she may be called a laser specialty nurse or a laser nurse coordinator. (Laser is an acronym for light amplification by the stimulated emission of radiation.) A laser gives off a high-powered beam of light that cuts tissue more cleanly than do scalpel blades. This process creates intense heat, rapidly clots blood vessels or tissue, and turns target tissue (e.g., a tumor) into vapor. All personnel must observe safety measures (e.g., wear eye shields, read door signs) during laser procedures to prevent injury to the patient and staff (AORN, 2010h).
Preparation of the Surgical Suite and Team Safety
The patient is unable to protect himself or herself during surgery; protection is provided by all members of the surgical team. The OR layout helps prevent infection by reducing contaminants through air exchanges in the room, maintaining recommended temperature and humidity levels, and limiting the traffic and activities in the OR. Safety straps are used for the patient, and the operating bed is locked in place. Blankets or warming units are used to prevent hypothermia, and interventions are used to prevent skin breakdown.
The nurse ensures electrical safety through proper placement of grounding pads and use of electrical equipment that meets safety standards. All equipment used during surgery must be functional and in proper working condition as determined by the safety procedure of that facility. Equipment is cleaned and, when required, sterilized so that it can be used as a part of the procedure. The scrub and circulating nurses together ensure a correct count of surgical instruments, sharps, and sponges. Counts are performed before the procedure, during the procedure as items are added or at the time personnel are relieved from that assignment, at closure of the first layer of the surgical wound, and immediately before complete skin closure (AORN, 2010l; Jackson & Brady, 2008).
Fire prevention and prevention of complications from the use of hazardous or toxic substances are concerns of all OR personnel. Ignition sources, oxidizers, and fuels are present in the OR and increase the risk for fires. Such events are rare but can occur during any kind of procedure. A cool room temperature (between 68° and 73° F [20° and 23° C]) with low humidity (20% to 60%) is optimal. The nurse is aware of emergency measures to take in the event of a fire or spill.
Layout
The surgical suite is located out of the mainstream of the hospital and near the PACU and support services (e.g., blood bank, pathology, and laboratory departments). Traffic flow is patterned to reduce contamination from outside the suite. Within the suite, clean and contaminated areas are separate. The surgical area is divided into three zones—unrestricted, semirestricted, and restricted—to ensure proper movement of patients and personnel.
The size of a surgical suite depends on the size and surgical capabilities of the facility. Most suites contain staff areas as well as areas related to patient care, surgery, and surgical support. Staff areas include locker rooms and staff lounges. Patient care areas include an admission or preoperative holding area and operating rooms. Surgical support areas include a number of ORs, cabinets for sterile supplies, separate utility rooms for clean and soiled equipment, and a clean linen room.
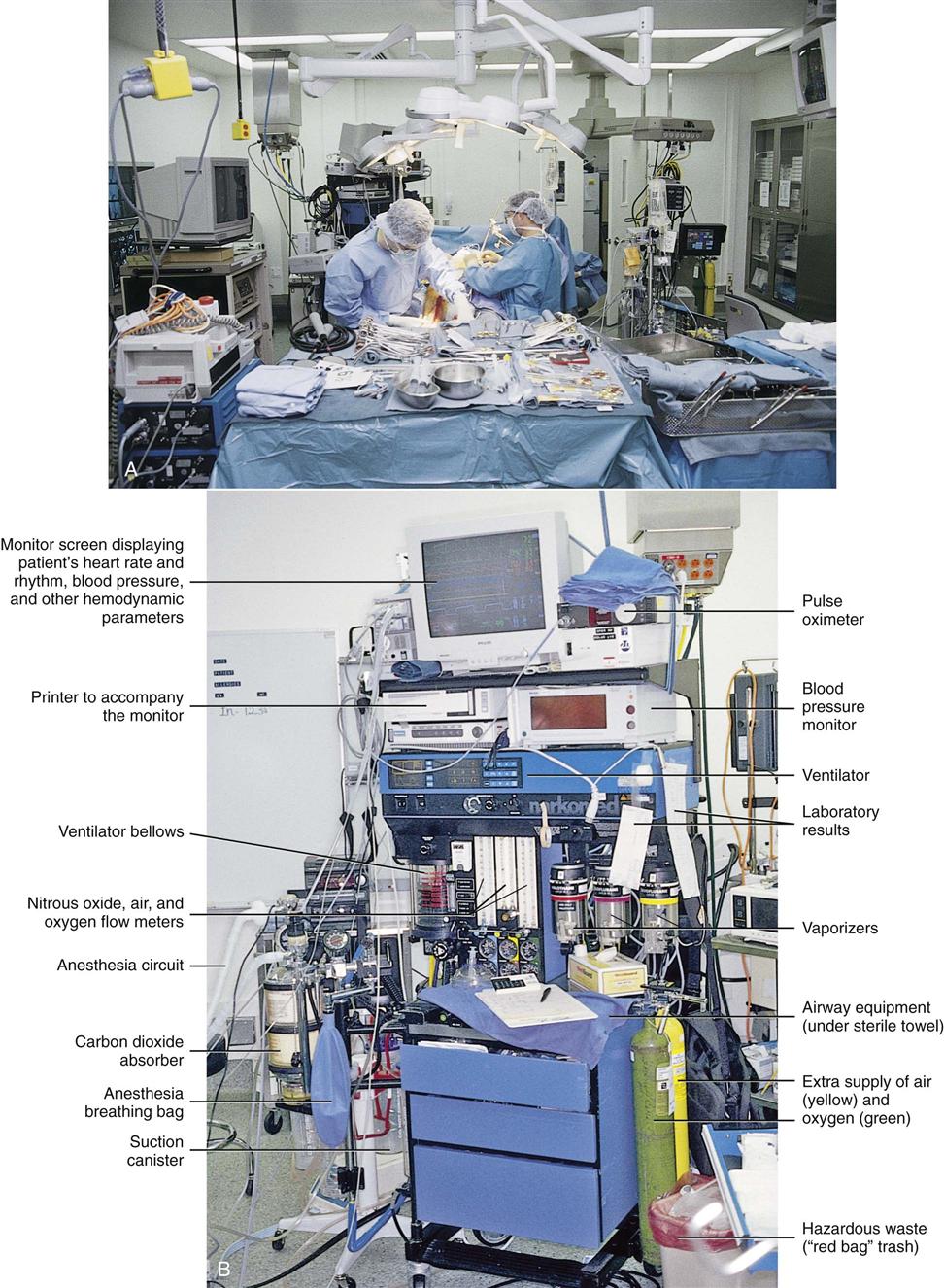
Fig. 17-3 shows a typical OR. The exact number of tables and equipment used in a room is based on the needs of each patient. A communication system links the OR and the main desk of the surgical suite. The system includes an intercom with separate systems for routine and emergency calls.
New OR designs use computers with the surgical equipment, lights, OR bed, and communications. These “hi-tech” rooms are similar to traditional ORs with the addition of computer equipment and panels. They are larger and more efficient for the surgical team with voice-activated commands operating some equipment that used to require manual operation.
Minimally Invasive and Robotic Surgery
Minimally invasive surgery (MIS) is now a common practice. Once used only for minor procedures and joint surgery, MIS is the preferred technique for many types of surgery, including cholecystectomy, cardiac surgery, splenectomy, and spinal surgery. It is even being used for cancer surgeries, such as the removal of a lung lobe (lobectomy) or even the entire lung (pneumonectomy) and colectomy. Research has verified many benefits of MIS, including reduced surgery time for some surgeries, smaller incisions, reduced blood loss, faster recovery time, and less pain and other discomfort after surgery.
MIS involves making one or more small incisions in the area of the surgery and placing an endoscope through the opening. An endoscope is a tube that allows viewing and manipulation of internal body areas (Fig. 17-4). Some endoscopes also magnify the view. These instruments may be rigid, semirigid, or flexible. Some have light sources, whereas others require that a separate light source be inserted into the surgical area. Endoscopes have different names and shapes for different surgical purposes. For example, laparoscopes are used for abdominal surgery, arthroscopes are used for joint surgery, and ureteroscopes are used for urinary tract surgery.
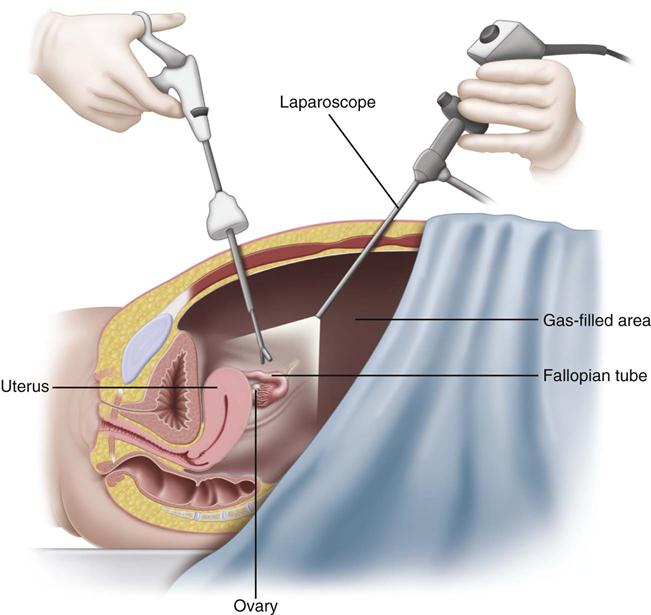
At one time, endoscopes were used only for examination and obtaining small specimens for biopsy. Now, these instruments can be used by surgeons for organ removal, reconstruction, blood vessel grafting, and many other procedures. Cutting, suturing, stapling, cautery, and laser surgery can all be performed through or with endoscopes. An important part of MIS for abdominal surgery, pelvic surgery, and surgery in some other body cavity areas is injecting gas or air into the cavity before the surgery to separate organs and improve visualization. This injection is known as insufflation and may contribute to complications and patient discomfort. It is one factor that is considered when deciding whether to perform a procedure by traditional “open” surgery or by endoscopy.
Patient preparation for endoscopic surgery is much the same as the preparation for the same procedure when performed by open surgical methods, especially for abdominal surgery. An endoscopic surgical procedure has a chance for becoming an open surgical procedure depending on what patient-related or procedure-related variables are discovered or develop during the surgery.
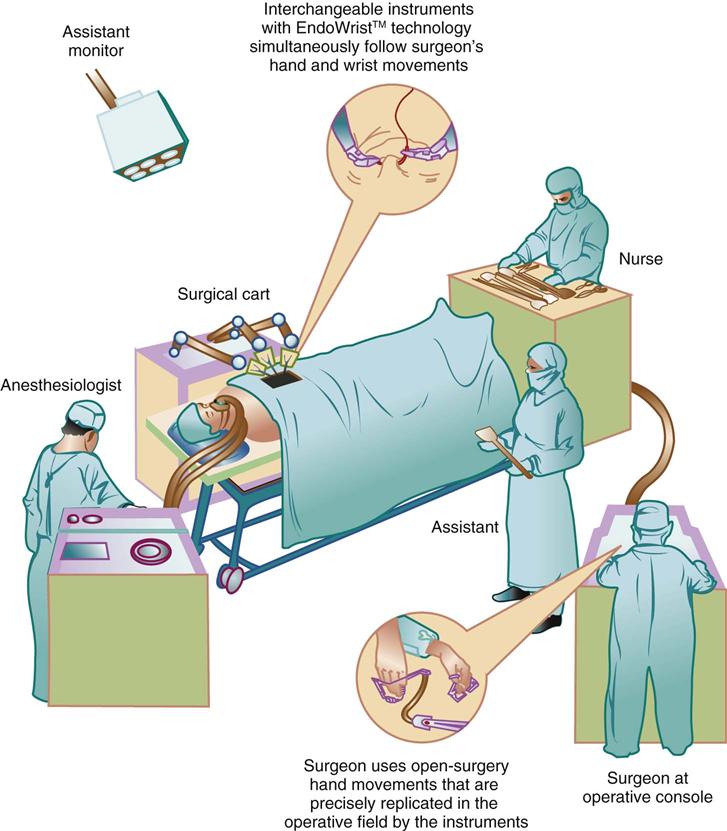
Robotic technology is drastically changing how surgery is performed and how the OR is organized. Robotic surgery takes minimally invasive surgery to a new level. Many gynecologic, urologic, and cardiovascular procedures are being performed by using robotics. The robotic system consists of several components (Fig. 17-5). These include a console, surgical arm cart, and video cart. Initially, the surgeon inserts the required instruments and positions the articulating arms; he or she then breaks scrub and performs the surgery while sitting at the console. A three-dimensional (3-D) view of the patient’s anatomy provides the surgeon with precise control and dexterity. The vision cart holds the monitors, cameras, and recorder equipment. This new technology requires a perioperative robotics nurse specialist who provides education for patients and family and training for members of the surgical team.
Mechanical trauma and thermal injury are two categories of injury that a patient can incur during MIS and robotic surgery (Ulmer, 2010). One limitation for both minimally invasive surgery and robotic surgery is the cost of special equipment and OR setting. In addition, surgeons require lengthy training and practice periods to become proficient in even one procedure performed using these endoscopic methods (Birch et al., 2007).
Health and Hygiene of the Surgical Team
People are a source of bacteria in the surgical setting. Everyone has bacteria on the skin and the hair and in the airways. Because these organisms can be transmitted to the patient, special health standards and dress are needed. Every surgical setting has policies and procedures for personnel and attire. Health standards require that all members of the surgical team and other support personnel in the surgical suite be free of communicable diseases. No one who has an open wound, cold, or any infection should participate in surgery.
Good personal hygiene helps prevent and control infection, as does frequent handwashing. Jewelry carries many organisms and should be minimal. All personnel must wash their hands between touching patients and performing procedures and more often when indicated. Hands of surgical personnel may be cultured on a regular basis to determine the potential for nosocomial (hospital-acquired) infections and to identify sources of pathogens. Further interventions or cultures are needed if quality reports (e.g., through the facility’s quality improvement program) indicate a problem. Routine cultures are usually obtained every 3 to 6 months. Surgical attire and the surgical scrub help prevent contaminations.
Surgical Attire
All members of the surgical team and all OR personnel must wear scrub attire while in the surgical suite. Scrub attire is provided by the hospital and is clean, not sterile. It is worn to reduce contamination from home and areas outside of the surgical setting. Basic surgical attire is a shirt and pants, a cap or hood (Fig. 17-6), and shoe coverings. Staff change into clean surgical attire in the OR suite locker rooms, not at home (AORN, 2010o). All members of the surgical team must cover their hair, including any facial hair.
In addition to basic attire, everyone must wear protective attire. This includes a mask, eyewear, gloves, gown, and shoe covers. Everyone who enters an OR where a sterile field is present must wear a mask. Surgical team members who are scrubbed and at the patient’s bedside during the surgery must also wear a sterile fluid-resistant gown, sterile gloves, and eye protectors, or face shields. Team members who are not scrubbed (e.g., anesthesia provider, circulating nurse) may wear cover scrub jackets that are snapped or buttoned closed (to prevent shedding of organisms from bare arms) and eyewear, as warranted.
Surgical Scrub
The surgeon, all assistants, and the scrub nurse perform a surgical scrub after putting on a mask and before putting on the sterile gown and gloves (Fig. 17-7). The scrub does not make the hands and forearms sterile. When the scrub is performed correctly, it reduces the number of organisms from the hands, arms, and nails. Rings, watches, and bracelets are removed before scrubbing because they may harbor organisms. Fingernails are kept short, clean, and healthy. Artificial nails are not worn because they too can harbor organisms.
A broad-spectrum, surgical antimicrobial solution is used for the surgical scrub. Plain or antimicrobial soap is used for washing hands immediately before the surgical scrub. Vigorous rubbing that creates friction is used from the fingertips to the elbow. The scrub continues for 3 to 5 minutes, followed by a rinse. During the rinse, hands and arms are positioned so that water runs off, rather than up or down, the arms (AORN, 2010p). After scrubbing, personnel enter the OR with their hands held higher than the elbows and thoroughly dry their hands and forearms with a sterile towel. This person is then assisted into a sterile gown (“gowning”) and puts on sterile gloves (“gloving”). Newer, alcohol-based surgical scrub agents may or may not require the use of water. Operating room personnel wash and dry their hands with soap and water before applying the agent to their hands and forearms, rubbing thoroughly until dry.
Gowns, gloves, and materials used at the operative field must be sterile. These items are changed between surgical procedures and as they become contaminated. The areas of the surgical gown considered sterile are the front of the gown from the chest to the level of the sterile field. The entire sleeves of the gown are considered sterile from 2 inches above the elbow to the cuff. The back of the gown is not considered sterile because it cannot be consistently seen by the wearer. Only when they are properly scrubbed and attired do members of the surgical team handle sterile drapes and equipment.
Anesthesia
The word anesthesia means “negative sensation.” Anesthesia delivery is a precise science. It requires the skill of an anesthesiologist, a certified registered nurse anesthetist (CRNA) working under the direction of an anesthesiologist or another physician, or an anesthesiologist assistant (AA—similar to a physician assistant) working under the direction of an anesthesiologist.
Anesthesia is an induced state of partial or total loss of sensation, occurring with or without loss of consciousness. The purpose of anesthesia is to block nerve impulse transmission, suppress reflexes, promote muscle relaxation, and, in some cases, achieve a controlled level of unconsciousness. Anesthesia providers use a separate anesthesia record for documentation.
Usually the anesthesia provider selects the type of anesthesia to be used after consulting with the patient and surgeon and after considering specific patient-related factors. The nurse and patient communicate patient preferences and fears about anesthesia to the anesthesia provider. Patient health problems are major factors in the selection and dose of anesthetic. Selection is also influenced by:
• Type and duration of the procedure
• Area of the body having surgery
• Safety issues to reduce injury, such as airway management
• Whether the procedure is an emergency
• Options for management of pain after surgery
• How long it has been since the patient ate, had any liquids, or had any drugs
• Patient position needed for the surgical procedure
• Whether the patient must be alert enough to follow instructions during surgery
• The patient’s previous responses and reactions to anesthesia
The physical status of a patient is ranked according to a classification system developed by the American Society of Anesthesiologists (ASA). The anesthesiologist assesses the patient and assigns him or her to one of six categories based on current health and the presence of diseases and disorders. The categories rank patients in a range from a totally healthy patient (P1 ranking) to a patient who is brain dead (P6 ranking) (Johnson, 2011). This system is used to estimate potential risks during surgery and patient outcomes.
Anesthesia delivery begins with selecting and giving preoperative drugs (see Chapter 16). The nurse must know the actions of commonly used drugs and their effects during and after surgery. Anesthetic agents affect many systems and can worsen other health problems, increasing the patient’s need for care. For example, most anesthetics are metabolized by the liver and excreted by the kidneys. Liver or kidney impairment increases anesthetic effects and the risk for toxicity. In addition, interactions may occur between the anesthetics and other drugs the patient has received.
Anesthesia can be induced in many ways (Table 17-1). The most common forms of anesthesia used in North America include general, regional, and local anesthesia. Hypnosis or hypnoanesthesia (which induces a passive, trancelike state), cryothermia (use of cold [e.g., ice] to reduce the surface temperature of the surgical site), and acupuncture are used less often.
TABLE 17-1
ADVANTAGES AND DISADVANTAGES OF VARIOUS TYPES OF ANESTHESIA
| TYPE | ADVANTAGES | DISADVANTAGES |
| General | ||
| Inhalation | ||
| Intravenous | Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| |