Rachel L. Palmieri and Donna D. Ignatavicius
Care of Critically Ill Patients with Neurologic Problems
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
11. Perform a focused neurologic assessment of patients who are critically ill.
12. Assess the patient on fibrinolytic therapy for potential adverse effects.
13. Develop and evaluate an evidence-based plan of care for the patient with a stroke.
14. Assess patients for adverse responses to TBI, such as increased intracranial pressure (ICP).
15. Develop a plan of care for interventions to prevent increasing ICP.
16. Manage care for the patient experiencing increased ICP.
17. Develop a postoperative plan of care for the patient having a craniotomy.
18. Prevent and monitor for postoperative complications of a craniotomy.
20. Explain the primary focus for management of patients with a brain abscess.

http://evolve.elsevier.com/Iggy/
Animation: Subarachnoid Hemorrhage
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
Some neurologic problems can cause patients to become critically ill or die. Stroke, head injury, brain tumor, and brain abscess are examples that can lead to life-threatening increased intracranial pressure (ICP). Permanent neurologic dysfunction or death may be prevented by early recognition and aggressive management of this complication by the bedside staff nurse. Serious and severe neurologic problems cause varying degrees of impaired mobility, sensation, and cognition. These impairments may be temporary or permanent and mild or severe depending on the nature of the health problem.
Transient Ischemic Attack and Reversible Ischemic Neurologic Deficit
Ischemic strokes often follow warning signs such as a transient ischemic attack (TIA) (also called a silent stroke) or a reversible ischemic neurologic deficit (RIND) (Chart 47-1). Both warning signs cause temporary neurologic dysfunction resulting from a brief interruption in cerebral blood flow, possibly due to cerebral vasospasm or systemic arterial hypertension. The difference between a TIA and a RIND is the length of time the patient is symptomatic. A TIA lasts a few minutes to fewer than 24 hours, whereas RIND symptoms last longer than 24 hours but less than a week. Typically, symptoms of a TIA resolve within 30 to 60 minutes. It is not unusual for symptoms to resolve by the time the patient reaches the emergency department (ED). Both TIAs and RINDs may damage the brain tissue with repeated insults, as seen on magnetic resonance imaging (MRI) or computed tomography (CT). Multiple TIAs indicate a high stroke risk.
Upon admission to the ED, the patient is stabilized as necessary. A complete neurologic assessment is performed, and routine laboratory work, electrocardiogram, and CT scan are done. Patients older than 65 years and those with diabetes, symptoms lasting longer than 10 minutes, or motor or speech difficulties often are admitted. At discharge, the patient is usually placed on anticoagulant therapy (e.g., clopidogrel [Plavix]) unless medically contraindicated. As part of the discharge processes, ensure that the patient is aware of bleeding precautions and the actions to take should bleeding occur. Anticoagulant therapy is discussed in detail in Chapter 38 in the Venous Thromboembolism section. Reinforce the need to follow up with the health care provider and to complete any diagnostic tests requested on an ambulatory care basis.
Stroke (Brain Attack)
Pathophysiology
A stroke is caused by a change in the normal blood supply to the brain. The National Stroke Association uses the term brain attack to better describe a stroke. Both terms are used in clinical practice. Any stroke is a medical emergency that strikes suddenly, and it should be treated immediately to prevent neurologic deficit and permanent disability.
Stroke is the third leading cause of death in the United States and is considered a major disability worldwide. According to the Centers for Disease Control and Prevention, approximately 136,000 Americans die each year from stroke (Centers for Disease Control and Prevention [CDC], 2011).
Pathophysiologic Changes in the Brain
The brain cannot store oxygen or glucose and therefore must receive a constant flow of blood to provide these substances for normal function. In addition, blood flow is important for the removal of metabolic waste (e.g., carbon dioxide, lactic acid). If blood supply to any part of the brain is interrupted for more than a few minutes, cerebral tissue dies (infarction). The result is varying degrees of disability, depending on the location and amount of brain tissue affected. Brain metabolism and blood flow after a stroke are affected around the infarction as well as in the contralateral (opposite side) hemisphere. Effects of a stroke on the contralateral (nonaffected) side may be due to brain swelling and further changes in blood flow throughout the brain. As a result of brain swelling, patients may develop clinical manifestations of increasing intracranial pressure, a potentially life-threatening complication.
Types of Strokes
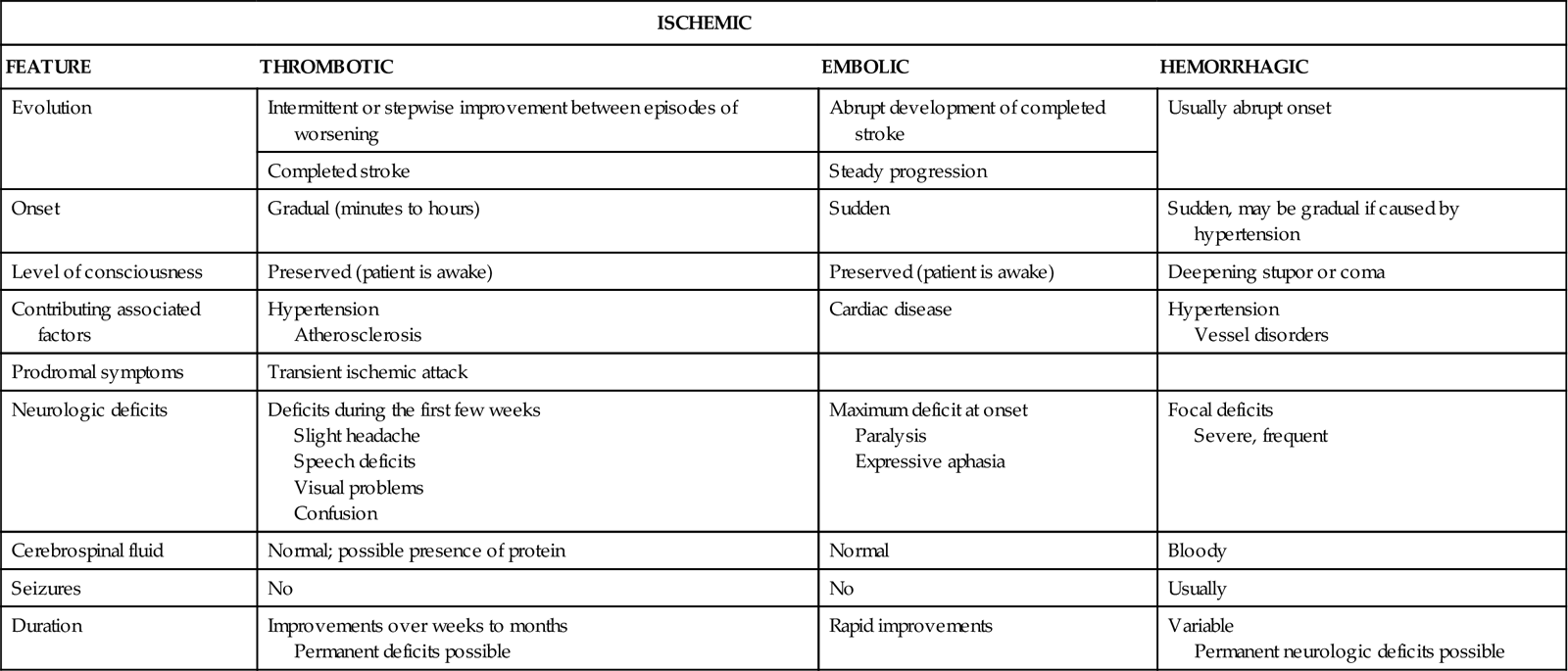
Strokes are generally classified as ischemic (occlusive) or hemorrhagic (Fig. 47-1). Acute ischemic strokes are either thrombotic or embolic in origin (Table 47-1). Most strokes are ischemic.
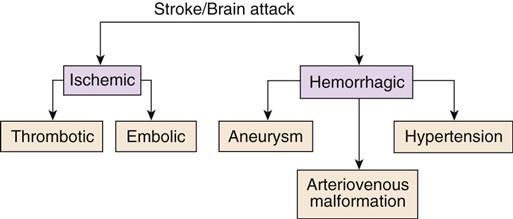
TABLE 47-1
DIFFERENTIAL FEATURES OF THE TYPES OF STROKE
| ISCHEMIC | |||
| FEATURE | THROMBOTIC | EMBOLIC | HEMORRHAGIC |
| Evolution | Intermittent or stepwise improvement between episodes of worsening | Abrupt development of completed stroke | Usually abrupt onset |
| Completed stroke | Steady progression | ||
| Onset | Gradual (minutes to hours) | Sudden | Sudden, may be gradual if caused by hypertension |
| Level of consciousness | Preserved (patient is awake) | Preserved (patient is awake) | Deepening stupor or coma |
| Contributing associated factors | Hypertension Atherosclerosis | Cardiac disease | Hypertension Vessel disorders |
| Prodromal symptoms | Transient ischemic attack | ||
| Neurologic deficits | Deficits during the first few weeks Slight headache Speech deficits Visual problems Confusion | Maximum deficit at onset Paralysis Expressive aphasia | Focal deficits Severe, frequent |
| Cerebrospinal fluid | Normal; possible presence of protein | Normal | Bloody |
| Seizures | No | No | Usually |
| Duration | Improvements over weeks to months Permanent deficits possible | Rapid improvements | Variable Permanent neurologic deficits possible |
Ischemic Stroke.
An acute ischemic stroke (AIS) is caused by the occlusion (blockage) of a cerebral artery by either a thrombus or an embolus. A stroke that is caused by a thrombus (clot) is referred to as a thrombotic stroke, whereas a stroke caused by an embolus (dislodged clot) is referred to as an embolic stroke.
Thrombotic Stroke.
Thrombotic strokes account for more than half of all strokes and are commonly associated with the development of atherosclerosis in either intracranial or extracranial arteries (usually the carotid arteries). Atherosclerosis is the process by which fatty plaques develop on the inner wall of the affected arterial vessel. Chapter 38 describes this health problem, including its pathophysiology, in more detail.
Rupture of one or more plaques exposes foam cells to clot-promoting elements in the blood. The end result is clot formation. If the clot is of sufficient size, it may interrupt blood flow to the brain tissue supplied by the vessel, causing an occlusive stroke. This process may occur over many years because collateral circulation to the involved area develops to compensate for the occlusion. The bifurcation (point of division) of the common carotid artery and the vertebral arteries at their junction with the basilar artery are the most common sites involved. Because of the gradual occlusion (blockage) of the arteries, thrombotic strokes tend to have a slow onset, evolving over minutes to hours.
Embolic Stroke.
An embolic stroke is caused by a thrombus or a group of thrombi that break off from one area of the body and travel to the cerebral arteries via the carotid artery or vertebrobasilar system. The usual source of emboli is the heart. Emboli can occur in patients with nonvalvular atria fibrillation, ischemic heart disease, rheumatic heart disease, mural thrombi after a myocardial infarction (MI), or insertion of a prosthetic heart valve. Another source of emboli may be plaque that breaks off from the carotid sinus or internal carotid artery. Emboli tend to become lodged in the smaller cerebral blood vessels at their point of bifurcation or where the lumen narrows.
The middle cerebral artery (MCA) is most commonly involved in an embolic stroke. As the emboli occlude the vessel, ischemia develops and the patient experiences the clinical manifestations of the stroke. However, the occlusion may be temporary if the embolus breaks into smaller fragments, enters smaller blood vessels, and is absorbed. For these reasons, embolic strokes are characterized by the sudden development and rapid occurrence of neurologic deficits. The symptoms may resolve over several hours or a few days. Conversion of an occlusive stroke to a hemorrhagic stroke may occur because the arterial vessel wall is also vulnerable to ischemic damage from blood supply interruption. Sudden hemodynamic stress may result in vessel rupture, causing bleeding directly within the brain tissue.
Hemorrhagic Stroke.
The second major classification of stroke is hemorrhagic stroke. In this type of stroke, vessel integrity is interrupted and bleeding occurs into the brain tissue or into the space surrounding the brain (usually intracerebral or subarachnoid).
Intracerebral hemorrhage (ICH) describes bleeding into the brain tissue generally resulting from severe hypertension. Elevated blood pressure (BP) leads to changes within the arterial wall that leave it likely to rupture. Damage to the brain occurs from bleeding, causing edema, distortion, and displacement, which are direct irritants to brain tissue. Hemorrhagic strokes occur more often with sudden, dramatic blood pressure elevations, such as those seen with cocaine abuse.
Subarachnoid hemorrhage (SAH) is much more common and results from bleeding into the subarachnoid space, the space between the pia mater and arachnoid layers of the meninges covering the brain. This type of bleeding is usually caused by a ruptured aneurysm or arteriovenous malformation (Mink & Miller, 2011b).
An aneurysm is an abnormal ballooning or blister along a normal artery, which usually develops in a weak spot on the artery wall, typically along the posterior circulation such as the basilar artery, vertebral artery, or the superior cerebral artery. Larger aneurysms are more likely to rupture than smaller ones.
Aneurysm rupture causes bleeding into the subarachnoid space, the ventricles, and/or intracerebral tissue. Vasospasm, a sudden and periodic constriction of a cerebral artery, often results from a cerebral hemorrhage due to an aneurysm rupture. Blood flow to distal areas of the brain supplied by the artery is markedly diminished, which leads to cerebral ischemia and infarction and further neurologic dysfunction.
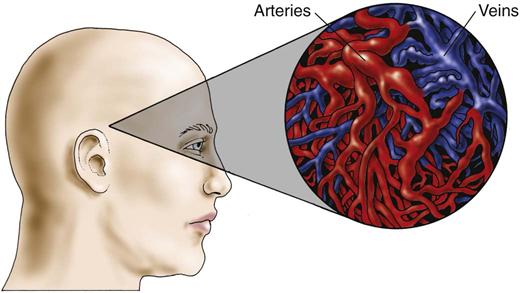
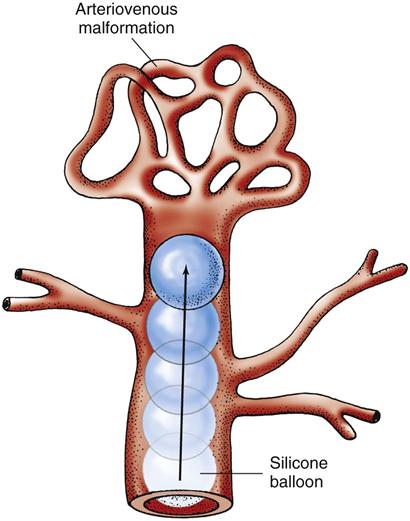
An arteriovenous malformation (AVM) is an uncommon abnormality that occurs during embryonic development. It is a tangled or spaghetti-like mass of malformed, thin-walled, dilated vessels (Fig. 47-2). The congenital absence of a capillary network forms an abnormal communication between the arterial and venous systems. The vessels may eventually rupture, causing bleeding into the subarachnoid space or into the intracerebral tissue, because normally the capillary network lowers the pressure between the arterial and venous systems. In the absence of the capillary network, the thin-walled veins are subjected to arterial pressure.
Etiology and Genetic Risk
Like that of many health problems, the causes of stroke are likely a combination of genetic and environmental risk factors. Major risk factors increase the likelihood of strokes and can be divided into those that can be modified and those that cannot (nonmodifiable factors). Many of these factors have a familial or genetic predisposition and are discussed elsewhere in this text. For example, first-order relative (mother, father, sister, brother) stroke risk increases with a strong family history of hypertension or atherosclerotic disease. Relatives of a patient with an aneurysm may be at higher risk for intracranial aneurysms and should consider diagnostic testing and follow-up.
Incidence/Prevalence
It is estimated that there are more than 4.7 million stroke survivors in the United States. About 730,000 strokes occur each year, but deaths have declined over the past 15 years. The number of strokes occurring in the younger adult population is increasing as a result of chronic IV drug abuse. Those using crack cocaine experience an increased incidence of stroke resulting from changes in the clotting mechanism caused by the drugs, spasm of cerebral vessels, or hemodynamic stress from the sudden increase in systolic blood pressure.
Some patients who have had strokes have another one within 1 year. Strokes tend to occur more often in the southern United States (“stroke belt”), which may be related to the larger older population, tobacco use, and obesity.
Although stroke symptoms can appear at any time of the day or night, researchers have found that there is a circadian pattern with a peak incidence between 6 AM and noon and the lowest incidence between midnight and 6 AM (Beal, 2010).
Health Promotion and Maintenance
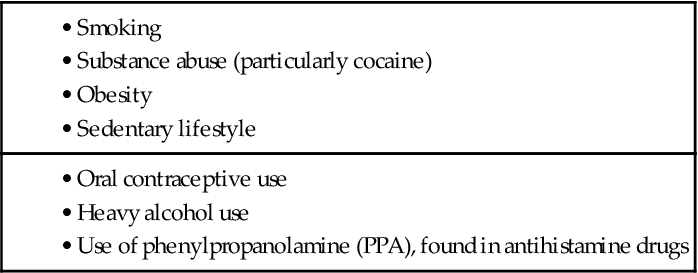
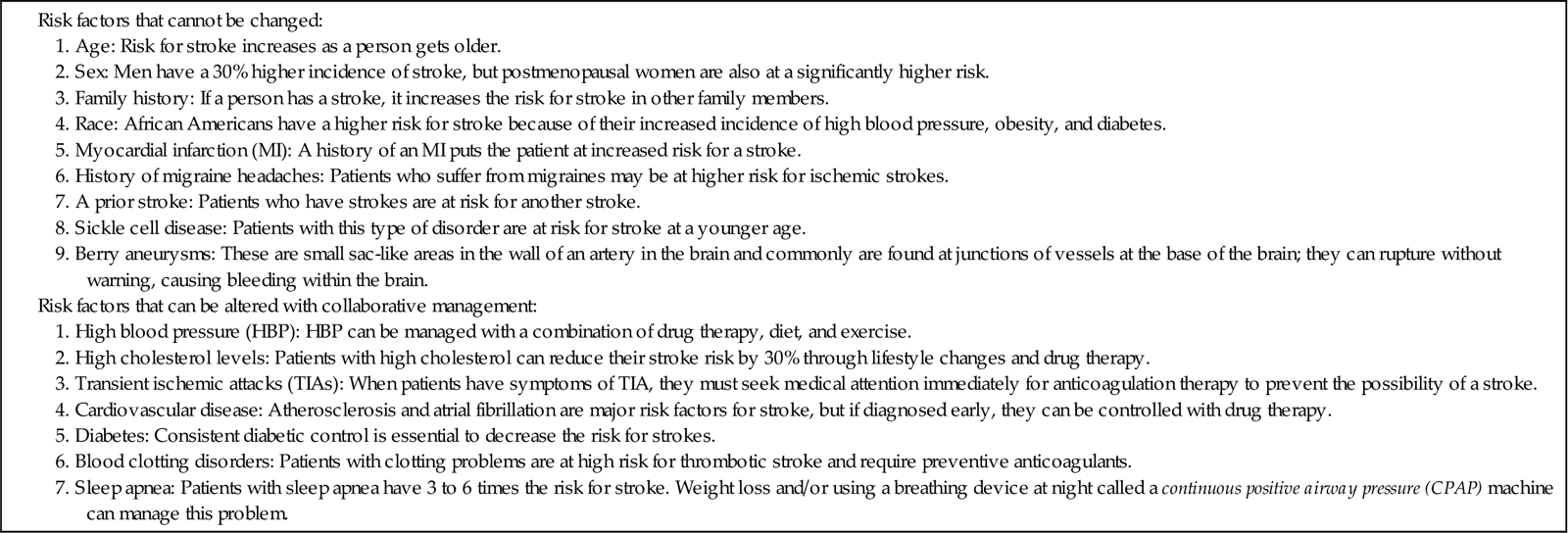
In 2007, the American Heart Association/American Stroke Association completed an exhaustive review of risk factors that contribute to stroke. These risk factors have been divided into three groups: risk factors that cannot be changed, risk factors that can be changed with medical treatment, and risk factors that can be changed by lifestyle modification.
People with predisposing health conditions should be aware that they could have a stroke unless they change their lifestyle habits (Chart 47-2). Teach them the importance of seeking professional health care and adhering to the recommended treatment plan. Also remind them that other risk factors contribute to health problems such a sedentary lifestyle and high-fat diet. Recommend a diet high in fruits and vegetables and low in saturated and trans fats. Light to moderate alcohol consumption may reduce the risk for stroke, but a higher consumption may increase it. Additional information about lifestyle modifications, such as weight control and smoking cessation, can be found elsewhere in this text. Table 47-2 lists common risk factors that cannot be changed (nonmodifiable) and those that may be altered with appropriate care management.
TABLE 47-2
Patient-Centered Collaborative Care
Assessment
History
An accurate history is important in the diagnosis of a stroke. The information obtained assists in identifying the area of the brain involved, as well as the cause.
If possible, obtain a history of the patient’s activity when the stroke began. Ischemic strokes often occur during sleep, whereas hemorrhagic strokes tend to occur during activity. Next ask the patient or a family member how the symptoms progressed. Be sure to document the history of the stroke’s onset. Symptoms of an embolic or hemorrhagic stroke tend to occur abruptly, whereas thrombotic strokes generally have a more gradual progression. Determine the severity of the symptoms, such as whether they worsened after the initial onset (hemorrhagic stroke) or began to improve (embolic stroke). It is important to determine whether the symptoms come and go, possibly indicating a transient ischemic attack (TIA) or a reversible ischemic neurologic deficit (RIND).
During the interview, observe the patient’s level of consciousness (LOC) and assess for indications of intellectual or memory impairments or difficulties with speech or hearing. Question the patient or family member about the presence of any sensory or motor changes, visual problems, problems with balance or gait, and changes in reading or writing abilities.
In addition, ask about the patient’s medical history with specific attention directed toward a history of head trauma, diabetes, hypertension, heart disease, anemia, and obesity. Obtain a list of current medications, including prescribed drugs, over-the-counter (OTC) drugs, herbal and nutritional supplements, and recreational (illicit) drugs. To complete the history, obtain data about the patient’s social history, including education, employment, travel, leisure activities, and personal habits (e.g., smoking, diet, exercise pattern, drug and alcohol use).
The patient with a cerebral aneurysm often reports the onset of a sudden, severe headache described as “the worst headache of my life.” Additional symptoms include nausea and vomiting, photophobia, cranial neuropathy, stiff neck, and change in mental status. There may also be a family history of aneurysms.
Physical Assessment/Clinical Manifestations
First responder personnel (e.g., paramedics, emergency medical technicians) perform an initial neurologic examination using well-established stroke assessment tools.
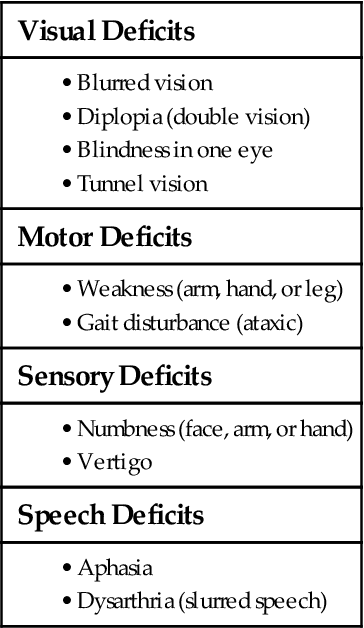
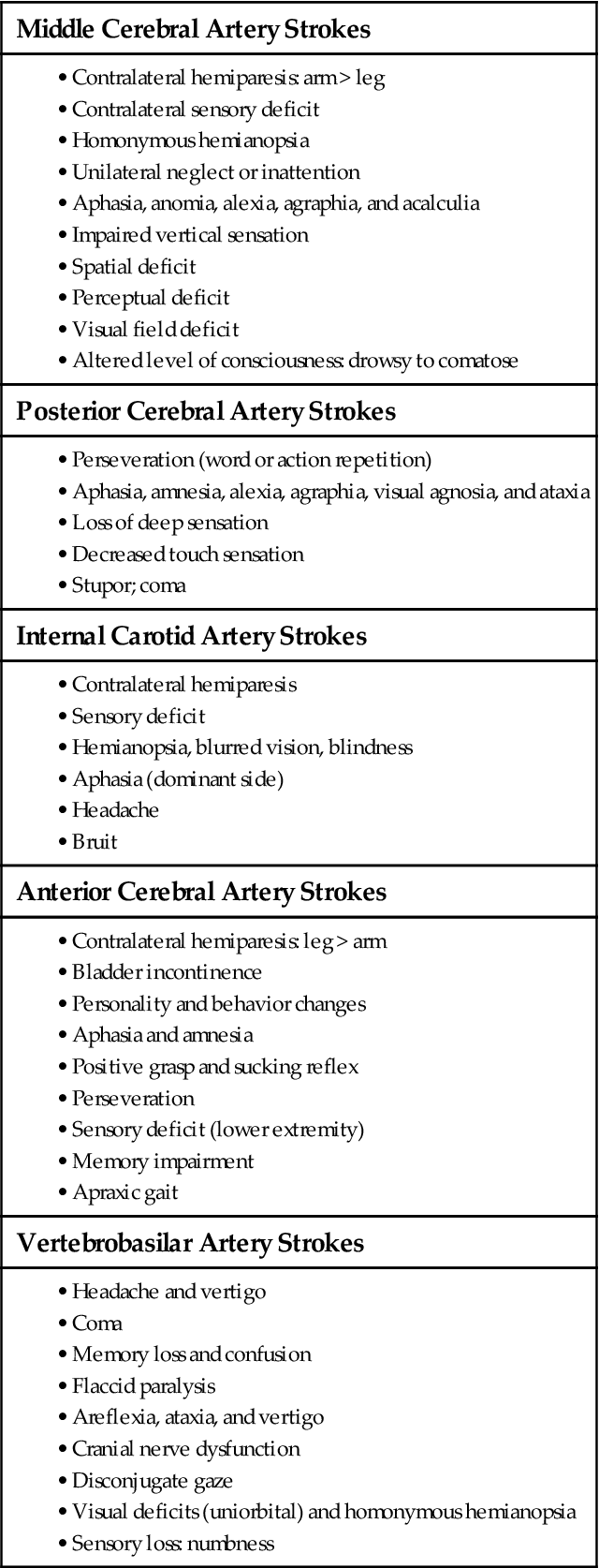
ED nurses perform a complete neurologic assessment on admission. The National Institutes of Health Stroke Scale (NIHSS) is a commonly used valid and reliable assessment tool that nurses complete as soon as possible after the patient arrives in the ED (Table 47-3). The NIHSS includes 11 areas of assessment and serves as the patient’s baseline (Mink & Miller, 2011a). The most important area to assess is the patient’s level of consciousness (LOC). Use the Glasgow Coma Scale (see Fig. 43-10 in Chapter 43 on p. 918) to frequently monitor for changes in LOC that could indicate increased intracranial pressure. Specific patient manifestations depend on the extent and location of the ischemia and the arteries involved (Chart 47-3).
TABLE 47-3
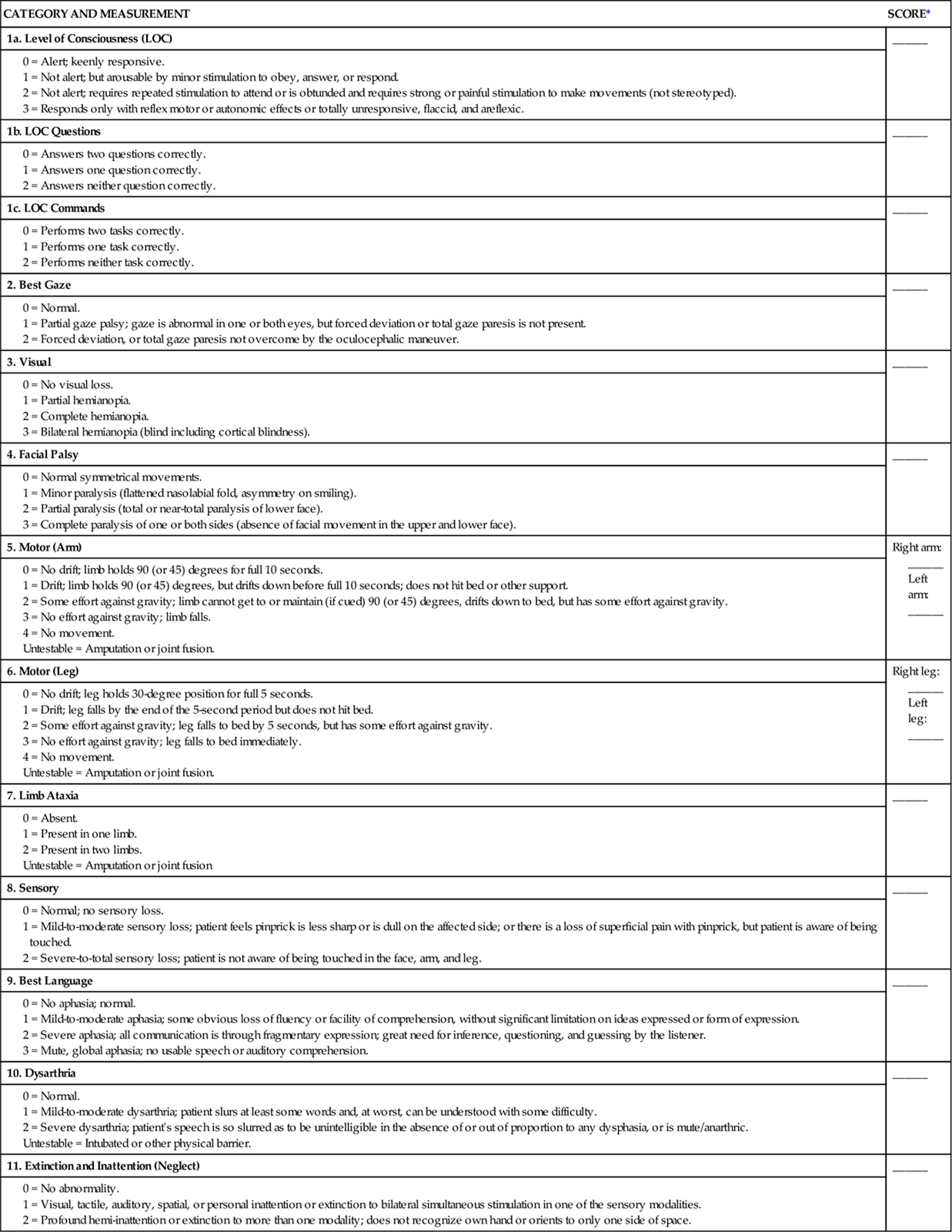
*The patient can have a score of 0 to 40, with 0 having no neurologic deficits and 40 being the most deficits.
Modified from National Institutes of Health Stroke Scale, 2003. www.ninds.nih.gov/doctors/NIH_stroke_scale.pdf.
Cognitive Changes.
The patient may have a variety of cognitive problems in addition to changes in LOC. LOC varies depending on the extent of increased intracranial pressure (ICP) caused by the stroke and on the location of the stroke. Assess for:
• Denial of the illness
• Spatial and proprioceptive (awareness of body position in space) dysfunction
• Impairment of memory, judgment, or problem-solving and decision-making abilities
• Decreased ability to concentrate and attend to tasks
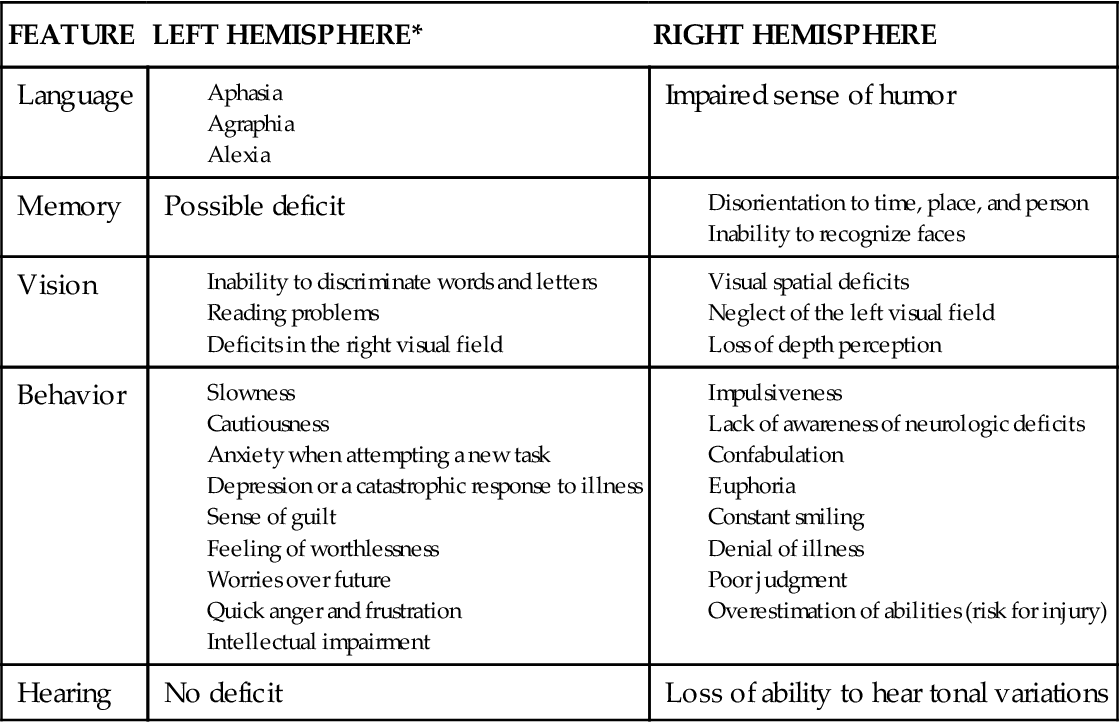
Dysfunction in one or more of these areas may be severe depending on the hemisphere involved (Chart 47-4).
The right cerebral hemisphere is more involved with visual and spatial awareness and proprioception (sense of body position). A person who has a stroke involving the right cerebral hemisphere is often unaware of any deficits and may be disoriented to time and place. Personality changes include impulsivity (poor impulse control) and poor judgment. The left cerebral hemisphere, the dominant hemisphere in all but about 15% to 20% of the population, is the center for language, mathematic skills, and analytic thinking. Therefore a left hemisphere stroke results in aphasia (inability to use or comprehend language), alexia or dyslexia (reading problems), agraphia (difficulty with writing), and acalculia (difficulty with mathematic calculation). A complete assessment of these problems is performed by a speech-language pathologist (SLP).
Motor Changes.
The motor examination provides information about which part of the brain is involved. A right hemiplegia (paralysis on one side of the body) or hemiparesis (weakness on one side of the body) indicates a stroke involving the left cerebral hemisphere because the motor nerve fibers cross in the medulla before entering the spinal cord and periphery. On the other hand, a left hemiplegia or hemiparesis indicates a stroke in the right cerebral hemisphere. If the brainstem or cerebellum is affected, the patient may experience hemiparesis or quadriparesis and ataxia (gait disturbance).
In collaboration with the physical therapist (PT) and occupational therapist (OT), assess the patient’s muscle tone. The patient with hypotonia, or flaccid paralysis, cannot overcome the forces of gravity, and the extremities tend to fall to the side. The extremities feel heavy, and muscle tone is inadequate for balance, equilibrium, or protective mechanisms. Hypertonia (spastic paralysis) tends to cause fixed positions or contractures of the involved extremities. Range of motion (ROM) of the joints is restricted, and shoulder subluxation may easily occur from either spasticity or flaccidity. Also assess proprioception, head and trunk control, balance, coordination, and gait. The patient who has had a stroke may also be unable to use an object correctly (agnosia) or carry out a purposeful motor activity or speech (apraxia).
Loss of neurologic control by the cerebral cortex causes a spastic (upper motor neuron) uninhibited bladder. Bowel function may also be affected. Assess the patient for incontinence (most common) or retention of urine and stool. Some patients have both problems.
Sensory Changes.
The sensory examination evaluates the patient’s response to touch and painful stimuli. In addition to diminished motor function, decreased sensation typically occurs on the affected side of the body.
Evaluate for indications of unilateral body neglect syndrome, which is particularly common with strokes in the right cerebral hemisphere. In this syndrome, the patient is unaware of the existence of his or her left or paralyzed side. The typical picture is that of the patient sitting in a wheelchair and leaning to the left with the arm caught in the wheelchair wheel. When questioned, the patient often states that everything is fine and believes that he or she is sitting up straight in the chair. The patient may wash or dress only one side of the body.
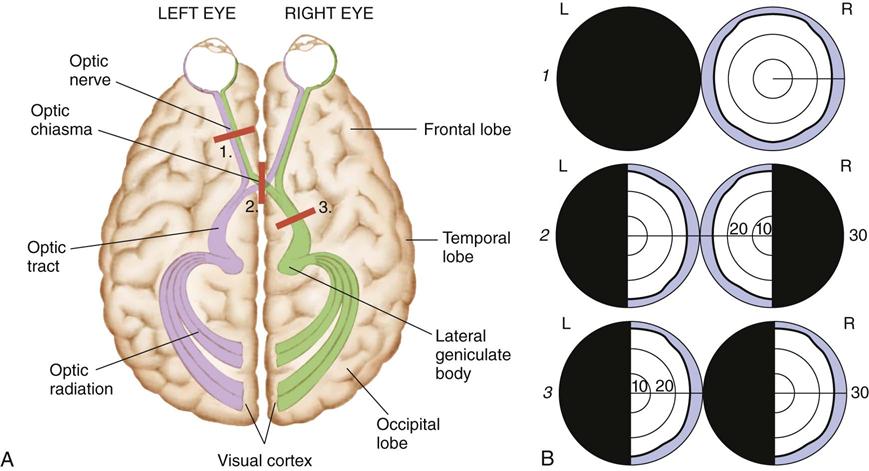
Another important part of the nursing assessment focuses on visual ability. Infarction or ischemia involving the carotid artery may cause pupil constriction or dilation, ptosis (eyelid drooping), visual field deficits, or pallor and petechiae of the conjunctiva. Amaurosis fugax, a brief episode of blindness in one eye, results from retinal ischemia caused by ophthalmic or carotid artery insufficiency. Hemianopsia, or blindness in half of the visual field, results from damage to the optic tract or occipital lobe. Usually this deficit occurs as homonymous hemianopsia, in which there is blindness in the same side of both eyes (Fig. 47-3). The patient with this condition must turn his or her head to scan the complete range of vision. Otherwise, he or she does not see half of the visual field. For example, the patient eats only half of a meal because that is the only portion seen. Patients with brainstem or cerebellar damage may have abnormal eye movements, such as nystagmus (involuntary movements of the eyes).
Cranial Nerve Function.
Assess the patient’s ability to chew, which reflects the function of cranial nerve (CN) V. Assessment of the patient’s ability to swallow reflects the function of CNs IX and X. In addition, note any facial paralysis or paresis (CN VII), absent gag reflex (CN IX), or impaired tongue movement (CN XII). The patient who has difficulty chewing or swallowing foods and liquids (dysphagia) is at risk for aspiration pneumonia and may become constipated or dehydrated from inadequate fluid intake.
Cardiovascular Assessment.
Patients with embolic strokes may have a heart murmur, dysrhythmias (most often atrial fibrillation), or hypertension. It is not unusual for the patient to be admitted to the hospital with a blood pressure greater than 180 to 200/110 to 120 mm Hg. Although a somewhat higher blood pressure (150/100 mm Hg) is needed to maintain cerebral perfusion after an acute ischemic stroke, pressures above this limit may lead to another stroke.
Psychosocial Assessment
The typical patient with a stroke is older than 60 years, is hypertensive, and has varying degrees of motor weakness and level of consciousness. Language and cognitive deficits, as well as behavior and memory problems, may also occur.
Assess the patient’s reaction to the illness, especially in relation to changes in body image, self-concept, and ability to perform ADLs. In collaboration with the patient’s family and friends, identify any problems with coping or personality changes.
Ask about the patient’s financial status and occupation, because they may be affected by the residual neurologic deficits of the stroke. Patients who do not have disability or health insurance may worry about how their family will cope financially with the disruption in their lives. Early involvement of social services, certified hospital chaplain, or psychological counseling may enhance coping skills.
Assess for emotional lability, especially if the frontal lobe of the brain has been affected. In such cases, the patient laughs and then cries unexpectedly for no apparent reason. Explain these uncontrollable emotions to the family or significant others so they do not feel responsible for these reactions.
Laboratory Assessment
Clinical history and presentation are usually enough to identify a stroke once it has occurred. No definitive laboratory tests confirm its diagnosis. Elevated hematocrit and hemoglobin levels are often associated with a severe or major stroke as the body attempts to compensate for lack of oxygen to the brain. An elevated white blood cell (WBC) count may indicate the presence of an infection, possibly subacute bacterial endocarditis, or a response to physiologic stress or inflammation. The health care provider typically requests a prothrombin time (PT) or international normalized ratio (INR) and a partial thromboplastin time (PTT) to establish baseline information in case anticoagulation therapy is started. These diagnostic tests may also provide supportive evidence that a hemorrhagic stroke has occurred.
Imaging Assessment
Brain imaging is the most important tool for confirming the diagnosis of a stroke. Computed tomography (CT) without contrast is the standard for initial diagnosis (Mink & Miller, 2011b). Cerebral aneurysms, if large enough, may also be identified. For a patient with an ischemic or occlusive stroke, the head CT is usually initially negative, indicating thrombotic or embolic stroke rather than intracerebral hemorrhage. After the first 24 hours, CT shows progressive changes of ischemia, infarction, and associated cerebral edema. This test is invaluable in establishing baseline information for future comparison in case the patient’s condition deteriorates. In addition, the scan enables the physician to identify pathologic changes that may mimic a stroke, such as a brain tumor or cerebral hematoma, both of which may be unrelated to cerebrovascular disease.
Magnetic resonance imaging demonstrates ischemic brain injury earlier than CT. Magnetic resonance angiography and multimodal techniques such as perfusion-weighted imaging enhance the sensitivity of the MRI to detect early changes in the brain, including confirming blood flow. Ultrasonography (carotid duplex scanning) and echocardiography help determine additional cardiovascular risks.
Other Diagnostic Assessment
To assist in the determination of a cardiac cause of a stroke, the health care provider may request a 12-lead electrocardiogram (ECG) and an evaluation of cardiac enzymes. As with other cardiovascular diseases, it is not unusual to find these changes on the ECG: inverted T wave, ST depression, and prolongation of the QT interval in the cardiac cycle.
Analysis
The priority problems for patients with a stroke are:
2. Impaired Swallowing related to neuromuscular impairment
4. Aphasia or dysarthria related to decreased circulation in the brain or facial muscle weakness
5. Urinary and/or Bowel Incontinence related to reflex bladder and bowel
6. Sensory changes related to altered neurologic reception, transmission, and perception
7. Unilateral body neglect syndrome related to disturbed perceptual abilities or hemianopsia
Planning and Implementation
Improving Cerebral Perfusion
Planning: Expected Outcomes.
The patient with a stroke is expected to have an adequate blood flow to the brain and through the cerebral blood vessels to maintain brain function and prevent further brain injury.
Interventions.
Interventions for patients experiencing strokes are determined primarily by the type and extent of the stroke. For patients having ischemic strokes, the standard of practice is to start two IV lines with non-dextrose isotonic saline (Summers et al., 2009). The immediate primary role of the nurse is to manage the patient receiving treatment and continuously assess for increasing intracranial pressure.
Nonsurgical Management.
Nursing interventions are initially aimed at monitoring for neurologic changes or complications associated with stroke and its treatment. The two major treatment modalities for patients with acute ischemic stroke are fibrinolytic therapy and endovascular interventions. If the thrombus is lodged in one of the carotid arteries, an endarterectomy may be performed. Regardless of the immediate management approach used, once the patient is stable, provide ongoing supportive care. Provide interventions to prevent and/or monitor for early signs of complications, such as hyperglycemia, urinary tract infection, and pneumonia. Implement interventions to prevent patient falls. These health problems are discussed in appropriate chapters in this textbook.
Fibrinolytic Therapy.
For select patients with ischemic strokes, early intervention with fibrinolytic therapy (“clot-busting drug”) is the standard of practice to improve blood flow to or through the brain. The success of fibrinolytic therapy from a stroke depends on the interval between the time the patient was last seen normal (LSN) and available treatment. It also depends on where the treatment is given. Hospitals with stroke centers or specialized stroke teams who care for numerous stroke patients have lower mortality rates than those hospitals that care for fewer of these patients (Bederson et al., 2009).
Intravenous (systemic) fibrinolytic therapy (also called thrombolytic therapy) for an acute ischemic stroke (AIS) dissolves the cerebral artery occlusion to re-establish blood flow and prevent cerebral infarction. Recombinant tissue plasminogen activator (rtPA [Retavase]) is the only drug approved at this point for the treatment of acute ischemic stroke. Thrombolytics activate plasminogen, which degrades the thrombus by breaking down fibrin. The most important factor in whether or not to give rtPA is the time LSN. The standard window for eligibility is 3 hours from time LSN. However, in 2009, the American Stroke Association recommended an expanded time interval from 3 to 4.5 hours for patients unless they fall into the following categories:
• Anticoagulation with an international normalized ratio less than or equal to 1.7
• Baseline National Institutes of Health Stroke Scale greater than 25
Fibrinolytic therapy is explained to the patient and/or family member, and informed consent is obtained. The dosage of the drug is based on the patient’s actual weight. Each hospital has strict protocols for mixing and administering rtPA and for monitoring the patient before and after rtPA administration.
Endovascular Interventions.
Endovascular procedures include intra-arterial thrombolysis using drug therapy and mechanical embolectomy (clot removal). Intra-arterial thrombolysis has the advantage of delivering the fibrinolytic agent directly into the thrombus within 6 hours of the stroke’s onset. It is particularly beneficial for some patients who have an occlusion of the middle cerebral artery or those who arrive in the ED after the window for rtPA. If the patient arrives in less than 8 hours, the interventional neuroradiologist may perform mechanical embolectomy using special instrumentation systems that can remove the clot by suction or other method (Mink & Miller, 2011a). Patients having either fibrinolytic therapy or endovascular interventions are admitted to the critical care setting for intensive collaborative monitoring.
Some patients may have worsening of their neurologic status starting within 24 to 48 hours after their stroke. A major complication is increased intracranial pressure (ICP) (Chart 47-6). Reassess patients every 1 to 4 hours (depending on severity of the condition) using the approved assessment tools.
Monitoring for Increased Intracranial Pressure.
The patient is most at risk for increased ICP resulting from edema during the first 24 to 48 hours after onset of the stroke.
Keep the head of the bed (HOB) elevated to between 25 and 30 degrees to prevent a decreased blood flow to the brain. The best HOB positioning has not yet been determined, and more studies are needed to determine best practice. Provide oxygen therapy to prevent hypoxia for patients with oxygen saturation less than 92% or those with a decreased LOC (Summers et al., 2009). Maintain the head in a midline, neutral position to help promote venous drainage from the brain. When severe hemiparesis is present, position the patient on his or her side to prevent aspiration and promote comfort.
In collaboration with other team members, avoid patient care activities that may increase ICP, especially if the patient has indications of cerebral edema. Avoid positioning the patient in extreme hip and neck flexion. Extreme hip flexion may increase intrathoracic pressure, which may make ICP more difficult to control. Extreme neck flexion interferes with venous drainage from the brain, also affecting ICP control.
Additional nursing considerations include avoiding the clustering of nursing procedures (e.g., giving a bath followed immediately by changing the bed linen) within a short time. This action is needed because the effect on ICP elevation is more dramatic when multiple activities are clustered within a narrow time period. Hyperoxygenating the patient before suctioning may also be appropriate to avoid even transient hypoxemia and resultant ICP elevation from dilation of cerebral arteries. Assess the necessity of suctioning because it increases ICP.
A quiet environment is particularly important for the patient experiencing a headache, which is common with an aneurysm or increased ICP. The patient may have photophobia (sensitivity to light). Therefore keep the room lights very low.
Monitor vital signs closely, at least every 1 to 2 hours. Notify the health care provider if the blood pressure exceeds acceptable levels. Generally, the health care provider allows the patient with acute ischemic stroke to be slightly hypertensive (a systolic blood pressure [SBP] between 140 and 150 mm Hg) to promote cerebral tissue perfusion. A higher blood pressure (above 180 mm Hg systolic and/or 110 mm Hg diastolic) could lead to a hemorrhagic stroke or rebleeding of an aneurysm (if present).
Evidence-based guidelines are not available for managing blood pressure in patients with hemorrhagic strokes, but for many patients, severe hypertension is the cause of their stroke (Mink & Miller, 2011b).
Carefully monitor the patient’s temperature because fever may cause increased ICP. Hypothermia may cause decreased cerebral perfusion. A complete discussion of the management of increased ICP, including drug therapy, is on p. 1027 under Interventions in the Traumatic Brain Injury section.
Patients admitted to a critical care unit are connected to a cardiac monitor and observed for dysrhythmias. The nurse performs a cardiac assessment, with particular attention directed toward auscultation of heart sounds to identify the presence of cardiac murmurs or atrial fibrillation (AF). Murmurs or AF may place the patient at increased risk for emboli. Close physical assessment for indications of hemodynamic stability is indicated. Invasive hemodynamic monitoring is often needed to monitor and evaluate physiologic stability and response to therapy.
Monitoring for Other Complications.
Monitor the patient with an aneurysm or arteriovenous malformation (AVM) for signs and symptoms of hydrocephalus and vasospasm. Hydrocephalus (increased cerebrospinal fluid [CSF] within the ventricular and subarachnoid spaces) may occur as a result of blood in the CSF. This prevents CSF from being reabsorbed properly by the arachnoid villi. Cerebral edema, which interferes with the flow of CSF out from the ventricular system, may also develop. Eventually the ventricles become enlarged. If hydrocephalus is left untreated, increased intracranial pressure (ICP) results. Observe for clinical manifestations of hydrocephalus, which are similar to those of ICP elevation, including a change in the LOC. Clinical findings may also include headache, pupil changes, seizures, poor coordination, gait disturbances (if ambulatory), and behavior changes.
Clinical manifestations of vasospasm may include decreased LOC, motor and reflex changes, and increased neurologic deficits (e.g., cranial nerve dysfunction, motor weakness, and aphasia). The symptoms may fluctuate with the occurrence and degree of vasospasm present.
Rebleeding or rupture is a common complication for the patient with an aneurysm or AVM. It may occur within 24 hours of the initial bleed or rupture and up to 7 to 10 days later. Assess for severe headache, nausea and vomiting, a decreased LOC, and additional neurologic deficits. Potential consequences of aneurysm rebleeding may be catastrophic.
Ongoing Drug Therapy.
Ongoing drug therapy depends on the type of stroke and the resulting neurologic dysfunction. In general, the purposes of drug therapy are to prevent further thrombotic episodes (anticoagulation) and to protect the neurons from hypoxia.
Although previously widely used, anticoagulants are controversial and are not considered current best practice by the American Stroke Association for acute ischemic strokes or for preventing future strokes (Adams et al., 2007). Sodium heparin and other anticoagulants, such as warfarin (Coumadin, Warfilone ![]() ), are high-alert drugs that can cause bleeding, including intracerebral hemorrhage.
), are high-alert drugs that can cause bleeding, including intracerebral hemorrhage.
However, an initial dose of 325 mg of enteric-coated or other form of aspirin (Ecotrin, Ancasal ![]() ) is recommended within 24 to 48 hours after stroke onset. Aspirin should not be given within 24 hours of rtPA administration. These drugs are antiplatelet drugs and prevent blood clotting by reducing platelet adhesiveness (clumping). They can cause bruising, hemorrhage, and liver disease over a long-term period. Teach the patient to report any unusual bruising or bleeding to the health care provider. The 2007 best practice guidelines for the treatment of acute ischemic stroke recommend against the use of clopidogrel (Plavix) alone or in combination with aspirin (Adams et al., 2007). However, many health care providers still prescribe them.
) is recommended within 24 to 48 hours after stroke onset. Aspirin should not be given within 24 hours of rtPA administration. These drugs are antiplatelet drugs and prevent blood clotting by reducing platelet adhesiveness (clumping). They can cause bruising, hemorrhage, and liver disease over a long-term period. Teach the patient to report any unusual bruising or bleeding to the health care provider. The 2007 best practice guidelines for the treatment of acute ischemic stroke recommend against the use of clopidogrel (Plavix) alone or in combination with aspirin (Adams et al., 2007). However, many health care providers still prescribe them.
To treat seizures, lorazepam (Ativan), a benzodiazepine, may be administered with close neurologic and cardiopulmonary monitoring. For long-term antiseizure therapy, the health care provider may also prescribe antiepileptic drugs (AEDs), such as phenytoin (Dilantin), gabapentin (Neurontin), or topiramate (Topamax). Neuroprotective drugs such as calcium channel blockers (e.g., nimodipine [Nimotop]) may be given to treat or prevent cerebral vasospasm after a subarachnoid hemorrhage. Vasospasm, which usually occurs between 4 and 14 days after the stroke, slows blood flow to the area and worsens ischemia. Calcium channel blockers work by relaxing the smooth muscles of the vessel wall and reducing the incidence and severity of the spasm. Neurologic functioning may improve, and further deterioration from ischemia is then prevented. In addition, these drugs dilate collateral vessels to ischemic areas of the brain. Although these neuroprotective and vasodilating drugs are sometimes used, the American Stroke Association does not recommend them (Adams et al., 2007). Stool softeners, analgesics for pain, and antianxiety drugs may also be prescribed as needed for symptom management. Stool softeners also prevent the Valsalva maneuver during defecation to prevent increased ICP.
Other Nonsurgical Interventions.
With the refinement of vascular stents, carotid artery angioplasty with stenting (CAS) is common to prevent or, in some cases, help manage an acute ischemic stroke. This interventional radiology procedure is usually done under moderate sedation. It may be performed by a cardiovascular surgeon or interventional radiologist.
A technique using a distal/embolic protection device has made this procedure very safe. The device is placed beyond the stenosis through a catheter inserted into the femoral artery (groin). The device catches any clot debris that breaks off during the CAS procedure. Placement of a carotid stent is performed to open a blockage in the carotid artery typically at the division of the common carotid artery into the internal and external carotid arteries. Throughout the procedure, the patient’s neurologic and cardiovascular status are assessed. CAS is less invasive, causes less blood loss, requires shorter hospital stays (overnight) and recovery time, and has fewer complications than a carotid endarterectomy. Postprocedure care is the same as that provided for a carotid endarterectomy (see Surgical Management on p. 1016).
A rare postprocedure complication, hyperperfusion syndrome, has a very high morbidity and mortality rate. This syndrome is thought to be the result of an impaired autoregulation of cerebral blood flow, which results from longstanding decreased cerebral perfusion pressure that occurs with carotid artery disease. The signs and symptoms include severe temporal headache, hypertension, seizures, and focal neurologic deficits. This syndrome may be associated with intracranial hemorrhage and may occur within 1 hour postprocedure up to 24 hours or even 1 week later (Oran & Oran, 2010).
The usual treatment of an arteriovenous malformation (AVM) uses interventional therapy to block abnormal arteries or veins and prevent bleeding from the vascular lesion. The same procedure may be performed to occlude the vessels surrounding an aneurysm. Under fluoroscopic guidance, the physician inserts a microcatheter into the carotid artery, typically using a femoral artery approach, and threads it to the vessel to be embolized. The physician then injects an embolic liquid agent to embolize the involved arteries (Fig. 47-4). When the liquid makes contact with the blood, it immediately hardens. Embolization is usually done before gamma knife or conventional surgery. (See later discussions of these procedures in this chapter.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree