Metatarsals fuse.
Head fuses with shaft.
Essentially the skeleton is composed of two frameworks: the axial skeleton and the appendicular skeleton.
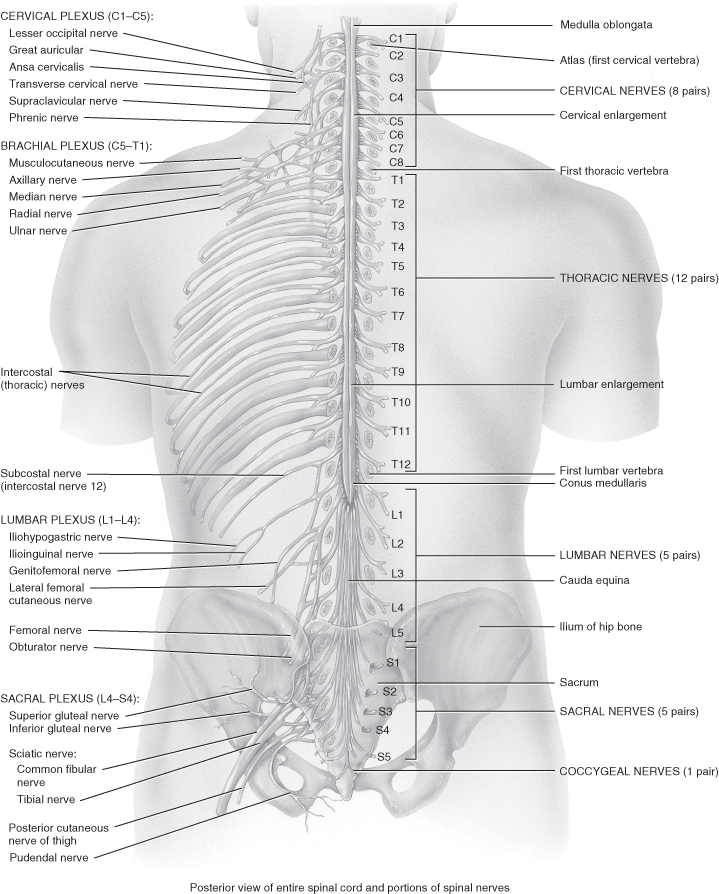
The axial skeleton consists of the ribs, sternum, vertebral column and skull. The skull and vertebral column house and protect complex vulnerable structures such as the spinal cord but permit exit and origins of the spinal nerves (see Figure 9.1). The appendicular skeleton consists of the bones that make up the upper and lower limbs and the bones referred to as girdles (the pectoral and pelvic girdles) which attach the limbs to the axial skeleton.
Figure 9.1 The spinal cord and the spinal nerves.
From Tortora, G.J. and Derrickson, B.H. (2009) Principles of Anatomy and Physiology, 12th edn. Reproduced with permission from John Wiley and Sons, Inc.
Fracture Classification and Bone Healing Following Injury
Despite the remarkable strength and indeed plasticity in young children, their bones are susceptible to fracture. Currey and Butler (1975) found immature bone to be weaker in bending strength but able to absorb more energy prior to fracture. During childhood most fractures result from trauma that twists or smashes the bones (e.g. sports injuries, road traffic accidents, falls and non-accidental injuries).
Fractures can be classified initially as:
- Position of the bone ends after fracture, i.e. non-displaced or displaced fracture.
- Completeness of the break, i.e. incomplete or complete.
- Orientation of the break relative to the long axis of the bone, i.e. linear or transverse.
- Whether or not the bone penetrates the skin resulting in an open fracture (Marieb and Hoehn 2010).
Fractures can also be described in terms of location of the fractures and the type of break, for example, fragmented, spiral, compression, depressed, greenstick or epiphyseal.
In simple terms a fracture is usually treated by reduction, realignment and immobilisation. Healing times are usually about 6–8 weeks in adolescence but may be quicker in younger children. Immobilisation following closed reduction usually involves application of a cast to maintain the corrected position, non-weight-bearing activities for lower limb injuries, or open reduction whereby the bone ends are surgically reduced with pins, wires or application of an external fixator.
Bone Healing Stages
Haematoma Formation
When a bone breaks, blood vessels in the bone and periosteum and perhaps in the surrounding tissues are torn and haemorrhage. As a result, a haematoma forms at the fracture site. Soon bones cells deprived of nutrition die and tissue at the site becomes swollen, painful and inflamed.
Fibrocartilaginous Callus Formation
Within a few days a soft callus forms. Capillaries grow into the haematoma and phagocytic cells invade the area and begin cleaning up the debris. Meanwhile fibroblasts and osteoblasts invade the fracture site. The fibroblast begins by producing collagen fibres which span the break and connect the broken bone ends, some differentiate into chondroblasts which secrete cartilage matrix. Osteoblasts then begin forming spongy bone. This results in the formation of a fibrocartilaginous callus that splints the bone.
Bony Callus Formation
Within a week new bone trabeculae begin to appear in the fibrocartilaginous callus and gradually converts it to a bony (hard) callus of spongy bone. Bony callus formation continues until a firm union is formed about 2 months later.
Bone Remodelling
This begins during bony callus formation and continues for several months after the bony callus is remodelled. Excess material is removed and compact bone is laid down to construct the shaft walls. The final structure resembles that of the original unbroken bony regions because it responds to the same mechanical stressors.
Musculoskeletal Trauma
Reasons for trauma depend on age, mobility and risk-taking. Trauma is the leading cause of death in children >1 year of age in the developed world and unintentional injury ranks as the leading cause of death between 1 and 34 years. Fatality rates are higher for children when compared with adults who have similar injuries. Motor vehicle collisions and falls account for the majority of multiple trauma (Barry et al. 2010) and most paediatric trauma is regarded as blunt trauma (Leonard et al. 2011).
Birthing injuries, such as shoulder dystocia and fractures, are rare, however they will need to be suspected and considered if there is deformity, impaired movement or if the infant seems in pain following birth. The under 5 year olds are at greater risk of non-accidental injury (NAI) and falls, and health protection campaigns have been launched to warn parents of small children of the dangers of open windows.
Injuries in pre-teenage years and adolescents result from more risk-taking behaviours. Road traffic accidents (RTA) cause the more serious injuries, but general activities such as sports, trampolines and falls are the most common.
Initial Assessment When a Child Has Traumatic Injury
The paediatric approach to trauma is to prioritise and treat life-threatening events. This will involve undertaking a primary survey to identify and treat these injuries. This will initially take place at the scene of the incident and will be undertaken again once the child arrives in the Emergency Department.
Primary Survey
Secondary Survey
Once the primary survey is complete and the child is stable, the secondary survey will be performed to inform ongoing management. On occasion, due to the severity of the child’s injuries, this may be performed in the intensive care environment. A good, clear history is vital, for example, the mechanism of injury, preceding events and AMPLE may be used to clarify events:
Investigations Required
Laboratory studies (full blood count, urea and electrolytes, blood glucose, coagulation, blood type cross-match) and radiological studies (cervical spine, chest, pelvis) that were not undertaken during the initial resuscitation should now be performed and a definitive management plan made. The identification and treatment of musculoskeletal injury at this time is already in progress; indeed, the first part of the initial assessment is airway with C-spine immobilisation. The secondary survey is a top to toe, front to back assessment where recognition of the severity of the injury may be identified and appropriate interventions undertaken. It is at this point that the value of positioning, splinting of injuries and pain management comes into play.
On arrival on intensive care it is vital that a correct, relevant and accurate history of events and interventions is documented and communicated effectively to the medical and nursing staff. Handover of the patient is a vital link in this chain of planning and providing care in the intensive care environment. Thorough, clear documentation and checklists may aid this communication. More recently, simulated events within the relevant clinical environment have been used to improve this process. For example, the simulated event of an admission from A&E to the PICU may be used. Many different specialities are involved in the immediate care of a paediatric trauma casualty: Emergency Department staff, paediatricians, surgical teams, orthopaedic teams and radiology.
The number of specialities involved could in itself result in a breakdown of communication and information transfer. These events are quite rare and teams need to work well together. By simulating this event the teams can get to know each other and appreciate each other’s strengths. Areas for improvement can be identified, not just in the performance of individuals but in the organisational system’s performance; this will result in enhanced care, procedures and policy development to improve clinical practice.
Because fractures in themselves are rarely life-threatening, when dealing with children who have multiple systems injuries the splinting of obvious fractures will generally be sufficient as the initial orthopaedic management, while the child’s general condition is stabilised. Loder (1987) reported that in 78 children who had multiple injuries, the early operative stabilisation of fractures within the first 2 or 3 days after injury led to a shorter hospital stay, a shorter stay in the ICU and a shorter time on ventilator assistance. In addition, there were fewer complications in those who underwent surgical treatment of the fractures less than 72 hours after injury.
When reviewing the top-to-toe evidence on the assessment and management of spinal musculoskeletal injuries it is important to acknowledge that some of the evidence and recommendations for management of certain injuries are based on adult findings and data. Until child-based evidence is available, adaptation of adult studies has been utilised.
Spinal Cord Injury (Table 9.2)
Spinal cord injuries (SCI) can be classified as complete or incomplete transection. A complete lesion is irreversible and will result in a loss of sensory, motor and autonomic functioning. The sensory, motor and autonomic functioning damage from incomplete lesions varies. Werndle and colleagues (2012) found variability in the management of adults with SCI. Although there are fewer spinal cord injury centres for children, given that many are nursed, initially at least, on general PICUs, the same lack of standardisation is likely to apply. This chapter focuses on conservative management. Although Singhal and colleagues (2008) found that the neurological outcome in surgically treated patients was comparable to that of conservatively treated patients and that the advantage of surgical management in closed cervical spine injuries (better alignment, easier manual handling and early mobilisation) was traded for poorer neurological outcome in adults, there are as yet no comparable studies for children.
Table 9.2 Spinal cord injuries in infants, children and young people
Source: adapted from Ball and Bindler 2008.
| Location of injury | Injury characteristics |
| Cervical spine | Site of approximately 60% of spinal injuries in children from birth to 10 years. An injury at C3 and above is usually fatal as these cause respiratory arrest. Survivors will require long-term ventilation. Injury from C5 will not affect diaphragmatic function. If the injury is at C6–7 children will retain some function in the upper limbs although this may be limited. With C-spine injuries there will be loss of sensation and sphincter control, leading to continence problems. |
| Types and cause of cervical spine injury | Occipitoatlantal dislocation – a rare injury, which usually occurs in RTAs and is associated with a high mortality. The mechanism of injury can be caused by hyperextension–rotation, combined with a distraction force. Care must be taken not to increase the dislocation. This requires immediate stabilisation and a halo applied before operation facilitates reduction and allows posterior occipitoatlantal fusion to be performed under optimum conditions. Atlas fracture– fracture of the ring of C1, caused by an axial compressive force applied to the head which results in direct compression of the ring of C1 by the occipital condyles. Traumatic atlantoaxial instability– in the older child (as in adults) this is most often a result of injury to the transverse ligament and the alar ligaments, resulting in an increased distance between the atlas and the dens of axis. Odontoid fractures – these account for approximately 10% of all C-spine fractures and dislocations in children. The injury in the child occurs at the synchondrosis at the base of the dens and displaces anteriorly. The mechanism of injury is usually associated with falls from a height or RTAs, however in children <4 years the mode of injury (MOI) could be relatively minor such as a fall from a cot or bed. Pedicle fractures of C2 – the MOI is usually extension and axial loading, with a high incidence of injuries to the face and head. The mechanism of injury is usually associated with falls from a height or RTAs. Fractures and dislocations of the subaxial spine – these are relatively rare in young children but may be seen in children >8 years and may include fracture dislocations, burst fractures, compression fractures, posterior ligamentous injuries, facet fractures and facet dislocations. |
| Thoracic spine | Account for approximately 20% of spinal injury usually between 8 and 14 years. Children may retain control of upper limbs but have poor trunk balance. Injuries above T6 can result in autonomic dysreflexia, which can be a medical emergency, so recognising and treating the earliest signs and symptoms efficiently can avoid the dangerous complication of hypertension. |
| Thoracic/lumbar spine | Retain control of muscles in abdomen and upper back. Children with injuries in this region retain trunk balance. |
| Lumbar spine | Injuries from L2 to L4 may occur because of poorly placed lap seat belts. Children who have injuries below L3 may retain the functioning of upper leg muscles but lose foot and ankle control. |
Spinal cord injuries (SCI) in children are relatively rare. In Europe the incidence of non-fatal SCI is 0.09–2.12 per 100 000 children per year (Barry et al. 2010).They are hard to diagnose because of the problem of obtaining a clear history due to developmental age (McCall et al. 2006) and the difficulty of imaging an immature spine. In addition, children usually regress developmentally in times of stress and injury, making communication challenging.
The patterns of injury in children >10 years are similar to those of adults, with a greater incidence of subaxial injuries than in younger children. In younger children spinal injuries are more commonly seen in the atlas, axis and upper cervical vertebrae owing to the relatively large size of the head, the immature skeleton and the immature supporting muscle and tissue structures which results in the fulcrum of injury being above C3. It is also important to remember that SCI may have occurred with the absence of abnormality on plain X-rays; SCIWORA (spinal cord injury without radiological abnormality). The clinical features may range from tingling and numbness to paralysis. Thoracic SCIWORA should also be considered in accidents involving high-speed direct impact, distraction from lap seat belts and crush injury by a slow-moving vehicle.
The mechanism of injury generally relates to the age of the child. At birth C-spine injury is not clearly defined, however breech and forceps deliveries are associated with SCI (Ruggieri et al. 1999).
SCI in infants and small children may be associated with NAI, therefore very careful consideration and care should be taken in relation to assessment and treatment. As stated, under 5 year olds are also at risk from falls and during pre-teens and adolescence RTA injuries predominate.
Cervical Spine Injury (C-Spine Injury)
C-spine injury should be suspected in any child who has sustained a significant head injury, has suffered blunt trauma to or above the clavicles, has a history of an RTA (as a pedestrian or car passenger), fall from a height, diving into shallow water, associated sporting injury (e.g. a scrum collapse in rugby, horse riding injury, etc.), hangings, NAI with suggested shaking injury or the unconscious child brought into A&E. This list is by no means exhaustive but if the mechanism of injury suggests potential spinal injury, care should be taken to stabilise the head and C-spine. One of the most common presenting complaints when a C-spine injury is present in an alert child is the presence of torticollis (limited neck motion) in which the child will hold the head to one side with the chin pointing to the opposite side.
Spinal Protection
A conscious, frightened child with an actual or suspected SCI is very difficult to immobilise completely and attempts at immobilising are inconsistent (Skettet et al. 2002), although excessive movement and instability need to be limited. In order to try to prevent the extension of the injury, management must be tailored to the patient’s age, neurological status, type and level of injury (Duhem et al. 2008). Initial attempts to protect the spinal cord can involve using a range of devices (cervical collar, spinal board, scoop stretcher, vacuum mattress), sedation and taking appropriate measures when rolling or moving the patient (log rolling).
If there is any concern in relation to C-spine injury the C-spine should be immobilised, usually by using an appropriate-sized hard collar and sand-bags (or equivalent medical device and tape). However, if the child becomes uncooperative or combatant, then they should simply have a hard collar applied (if they will tolerate it). When immobilisation of the head is too rigid there may be an increase in the leverage on the neck as the child struggles, therefore this should be avoided. It is important that the child is treated in a calm atmosphere and communicated with appropriately for their age and level of development so that anxiety and stress are minimised. Parents should ideally remain at the bedside to help facilitate this.
In relation to positioning, Herzenberg and colleagues (1989) reported on 10 children under 7 years of age with unstable C-spine injuries who were found to have an anterior angulation or translation on the lateral radiograph when the patient was positioned on the traditional backboard. They recommend using a bed or a backboard with a posterior recess for the head to drop posteriorly and prevent angulation of the neck.
Log-Rolling
Spinal cord instability should be assumed in all patients with significant trauma injuries until such an injury is excluded. These patients should be log-rolled during the initial assessment and the entire spine should be inspected and palpated for ecchymoses, soft tissue swellings, step-offs and tenderness. Every patient with a suspected spinal injury also needs a thorough and careful neurological examination.
Physical Examination
The physical examination should be undertaken by an experienced clinician and the neck palpated for tenderness, muscle guarding or the presence of a gap in the spinous process that would indicate a posterior ligamentous injury.
Radiography
Radiographic evaluation should be performed along with other C-spine imaging according to local protocols. A complete radiographic examination should include a lateral view, anterior-posterior (AP), and odontoid (open mouth) view, but omit if a CT scan of the head is also required as then a CT of the upper C-spine should be done instead. Oblique views if the lower C-spine is inadequately visualised on the lateral view (this is rarely needed in children) can be notoriously difficult to obtain in young children. The use of the CT scanner has increased in recent years and when CT scanning the head-injured patients bound for intensive care, it seems logical to scan the neck at the same time. A CT scan of the neck reduces the risk of missing an injury of the C-spine (Morris et al. 2004). An MRI scan may be required if there are features of neurological deficit.
Thoracic and Lumbar Spinal Injuries
In children these are less common than C-spine injuries; children under 10 years are more likely to sustain upper thoracic injuries (T4–T10) as a result of a fall or motor vehicle/ pedestrian collision. Between the ages of 10 and 20 years they are more likely to sustain injuries at the thoracolumbar junction (T12–L1), again predominantly as a result of motor vehicle injuries or recreational pursuits.
Some key concepts need to be considered in relation to thoracic and lumbar injuries. First, the ligaments are more elastic and forgiving, second, there is a higher ratio of cartilage to bone, and third, the facets are more horizontal allowing greater motion. The three column spine also requires understanding a concept introduced by Denis (1983). Denis realised that complete rupture of the posterior ligamentous structures did not produce instability. Rather, instability in flexion requires not only rupture of the posterior ligaments but also disruption of the ‘middle column’ – the posterior longitudinal ligament, the posterior annulus fibrosus and the posterior wall of the vertebral body. The anterior column consists of the anterior longitudinal ligament, the anterior annulus fibrosus and the anterior vertebral body. The posterior column is made up of the posterior arch and posterior ligamentous complex. Injuries to the thoracic and lumbar spine are usually the result of high energy forces. They can also be difficult to diagnose as these patients may frequently have associated injuries and an altered state of consciousness. The force that produces the injury is more commonly flexion, which may be combined with compression, distraction or shear forces.
Acute Spinal Cord Injury in Context
An injury to the spinal cord potentially exposes the child to the systemic factors which can be related to injury such as inflammation and infection. Also interruption to the central control of the sympathetic outflow and lack of ‘back-up’ spinal reflexes supporting this, particularly in the weeks immediately following an SCI, means that cardiovascular control, compensation for postural change and the effect of gravity are functionally absent below the level of the lesion.
Management in Intensive Care
When planning the management and care of these injuries the focus will depend on the site of injury/fracture and its severity. Whether it is a C-spine, thoracic or lumber a spinal injury care should be taken when moving these patients. In the initial phases, if there is concern about the C-spine, then it should be immobilised with the ‘Holy Trinity’ of sandbags, collar and tape. The next level of intervention may depend on whether or not surgery, such as halo traction, is required to stabilise the injury.
If the injury does not require immediate surgery, the child will be maintained in an intensive care environment for conservative continuation of care as the general consensus seems to be that the next stage is a waiting game; initially it may be impossible to determine the extent of the injury until the child is awake and a more detailed neurological examination can take place. The primary insult has occurred at the time of the initial injury, therefore the general principle is to prevent a secondary insult by taking care and immobilising the injury. Time is something that the child has, but this uncertainty can be a frustrating and anxious time for the family as they wait to find out the full extent of the injury. This frustration can be shared by the intensive care team as prediction under this degree of uncertainty is unwise.
Steroid Use
A number of pharmacological agents have been used in an attempt to improve recovery after SCI. The aims of using these agents are to reduce swelling and oedema and prevent ischaemic injury. A number of drugs have been tried, but only methylprednisolone has received widespread clinical attention. There is some controversy in the use of steroids in terms of balancing the benefits and outcomes of a high dose against the increased incidence of pneumonia and a potentially longer ICU stay, but no change in mortality and a decrease in rehabilitation periods have been identified (Gerndt et al. 1997). Despite this, many units administer methylprednisolone to patients with SCI within 3 hours of injury and maintain them on this treatment regime for 48 hours.
Spinal Neurological Shock
Continuous monitoring should be undertaken in all critically injured patients and the intensive care nurse should observe the patient for signs of shock caused by neurological injury. Signs include a fall in blood pressure and a drop in heart rate (in hypovolaemia one would usually observe a fall in blood pressure with an accompanying tachycardia).
Moving and Handling
Spinal immobilisation should be continued in the intensive care environment. The difficulty in relation to paediatric intensive care patients is that they may often be ventilated and sedated/muscle relaxed and may also have other associated injuries. The simple rule is that all of these patients should be assumed to have spinal column instability until the injury can be excluded. This creates quite a challenge in paediatric intensive care.
In relation to C-spine immobilisation one of the disadvantages of the rigid collar is that it gets soiled and may result in pressure sores if used long term. An alternative is an Aspen collar. This is a two-part collar with the front detaching to give access the patient. It also has interchangeable foam inserts which can be changed when performing cares.
When undertaking nursing procedures, the care of the child’s C-spine requires two people and clear communication must be maintained throughout. This is particularly important in any procedure where a collar and any anchoring tapes have to be temporarily removed to assess skin integrity or maintain hygiene. One person should manually stabilise the head and neck while the other removes the tapes and sandbags, etc., and then undertakes the procedure.
When changing sheets or the position of the patient the child should be moved by log-rolling. The main issue with this manoeuvre is how many people are required as this will have a demand on the nursing staff. PICUs operate on a 1:1 nurse–patient ratio. If a unit has six patients and one of these patients is an adolescent with a spinal injury, then it may take four people to roll and one person to undertake the nursing care –five in all. This is where a multidisciplinary approach is vital as medical staff and physiotherapists should be co-opted to assist. Therefore, all staff should be trained in log-rolling and handling techniques to care for a patient with a spinal injury. As an alternative, the patient may be nursed on a spinal bed such as a Stryker frame which permits turning in various planes without the movement of individual parts. This is not suitable for small children or for young people who demonstrate loss of physiological stability when turned prone (see autonomic dysreflexia).
If the patient needs to be moved for further imaging investigations such as CT or MRI, this creates another set of obstacles to be overcome. The use of vacuum mattress-type devices has been introduced into paediatric intensive care mainly to transport critically ill children. The value of this should not be underestimated for intra-hospital transfers either. Mattresses could be utilised in taking the patient to CT as many of these devices are now CT-compatible and will allow the safe transfer of patient from bed to CT scanner and back again. Before taking a child for an MRI the compatibility of vacuum mattress needs to be confirmed.
Special Considerations with High Spinal Injury
Children with high spinal lesions need to be handled with care to avoid autonomic dysreflexia which is a medical emergency, so it is important to recognise and treat the earliest signs and symptoms:
- Headache.
- Cutis anserina (goose bumps).
- Red, blotchy and sweaty above the level of injury.
- Slower than usual pulse, hypertension.
- Nausea.
- Cold, clammy skin below level of spinal injury.
Autonomic dysreflexia can be caused by any stimuli such as irritants, pressure and pain to the body below the level of spinal injury. Things to consider include an overstretched bladder, UTI or bowel over-distension due not only to constipation or impaction, but also tight clothing or uncomfortable bedding.
On-Going Management
The care of the patient with an SCI can be both challenging and rewarding for the intensive care team. It produces a unique set of challenges due to the site and severity of the injury sustained and the consequences. This will vary from individual to individual but this group of patients will generally be initially immobilised, on bed rest, may be sedated and ventilated and will potentially be at risk of developing pneumonia, sepsis, pressure sore injury and DVT, and will need complete supportive management.
Respiratory Care
Initial respiratory care will focus on appropriate ventilatory care and prevention of nosocomial infection. This group of patients may be at risk of developing pneumonia or sepsis. Therefore, it is important that careful attention is paid to providing good respiratory care Chapter 4.
In terms of the patient with an SCI, attention should considered for long-term management. The level, innervation and severity of the injury will dictate long-term management. C3, C4 and C5 innervate the diaphragm. Therefore spinal cord injury at this level will dictate whether the patient will be ventilator-dependent and may also require a tracheostomy in the long term. In the immediate environment of intensive care this is generally viewed as routine care management, but to family and the patient this is a life-changing event and the psychological impact should not be underestimated. This will put an immense strain on any family. For example, as a result of a major RTA, the infant who sustains a C3 fracture will be ventilator-dependent for life. If this is the case, support mechanisms should be put in place as soon as possible, utilising all the skills of the multidisciplinary team to facilitate care, including the community respiratory care teams. Once the patient is stable and recovering, plans should be put in place for the continuation of care. This is where the importance of a good high dependency facility is so important and access to one of these can allow for transfer. Some contact should also be made with units that specialise in the intermediate and long-term care of patients with an SCI as they can have a lot to offer.
Specialist Feeding
As with any intensive care patient calorific requirements are vital to recovery. Nasogastric or naso-jejunal feeds should be commenced in line with unit policy. Dietetic involvement and a nutritional management plan are a necessity in care provision (Chapter 12).
Elimination
The patient will be catheterised with the appropriate urinary catheter for the age of the child. Attention should be paid to accurate fluid balance monitoring in relation to input and output. Urine output should ideally be 1 ml/kg/hr. Catheter care should be undertaken as part of hygiene management but the risk remains that the patient could develop a urinary tract infection, therefore careful monitoring of the character and composition of urine should be undertaken when measuring output. The PIC nurse needs to be aware of the signs of underlying infection (raised temperature, tachycardia, offensive smelling urine, protein in the urine, etc.) as the consequences will depend on the site and severity of injury. The spinal nerves that relate to bladder and bowel function innervate at lumbar level, therefore as with respiratory care, long-term planning is vital.
As a result of the injury the child may have to use intermittent catheterisation in the long term and need appropriate bowel management. This is where early communication with specialist services such as a urology nurse specialist is vital in planning and coordinating immediate and future care.
Pain
As with any musculoskeletal injury, pain management is vital. Initially, the child may be sedated and ventilated, depending on the severity of the injury and any coexisting injuries such as a head injury. There may be cases, however, when the child has sustained an injury that may not require sedation or ventilation (e.g. a thoracic SCI). In these circumstances, pain assessment scores and appropriate analgesic intervention will be required. A pain score should be utilised that is appropriate for the child’s age and development, and analgesia administered as prescribed. Opiates should be avoided when dealing with non-ventilated tetraplegia or high paraplegia as they can cause respiratory depression. Diclofenac tends to be the drug of choice for these patients although most other general analgesics can be used (Chapter 13).
Bone Loss, Contractures and Scoliosis
Although the mechanism of future bone loss in these children is not fully understood, it is likely to be a complex interplay between hormones, drug therapy, gender and genetic predisposition. The loss of mechanical stimuli of bone has a major impact on bone integrity, and in individuals with SCI, bone loss begins immediately after injury (Dionyssiotis 2011). This makes these children more prone to subsequent bone injury below the spinal cord injury, so effective and efficient management of movement and positioning learned from the start of rehabilitation may prevent later fractures and complications. Associated muscular atrophy and spasticity can complicate rehabilitation, and positioning supports, splints, footboards, boots and braces all have a role in preventing contractures and optimising residual function. Scoliosis can complicate positioning and respiratory function if the injury was sustained before the skeleton was mature.
Psychosocial Concerns
Adverse psychological and social effects are part of the process of an enforced hospital stay and an admission to intensive care, accompanied by the fact that damage from a SCI may be permanent and the consequences life-changing. Helping the child and family accept the situation is not solely the role of the intensive care nurse as the child will be transferred to rehabilitation and ongoing care units. However the children’s nurse working in the PICU can provide a solid platform by being honest and transparent and never providing false hope or colluding with denial. Even during the early stages the family can benefit from counselling and the idea introduced that the child will need long-term psychological support and not just physical care. While the child is in PIC the children’s nurse role stops short of motivational coaching, but allowing the family to sink into deep despair is not in anyone’s interests. There are some remarkable role models who have overcome disability and achieved incredible results in every sphere of life.
Ruling out C-Spine Injury and Providing Clearance
Ruling out C-spine injury is notoriously difficult in the 0–3 years age range (Anderson et al. 2010) and in the unconscious ventilated patient as generally requirements such as no radiological abnormality, no pain, paraesthesia or paralysis, normal neuro-muscular status observed and can communicate these findings effectively, will be impossible to determine. There are no guidelines to assist the decision-making process. The decision should be taken by an orthopaedic surgeon or neurosurgeon and until the spinal injury is considered clear, then the standard nursing management in relation to care of the spinal injury (i.e. immobilisation and log-rolling, etc.) will apply.
Pelvic Injury
Pelvic ring stability is provided by an intact ring of bones and by strong connecting ligaments, therefore pelvic stability is as much about the state of the ligaments which make the connections as the skeletal framework. These are:
- Iliolumbar ligaments.
- Dorsal sacroiliac ligaments.
- Sacrotuberous ligaments.
- Ventral sacroiliac ligaments.
- Sacrospinous ligaments.
- Posterosuperior interosseous ligaments.
Fractures to the pelvis are rare in children. Motor vehicle accidents account for about 60% in adults (Frakes and Evans 2004) and about 75–90% of all pelvic fractures in children. Whereas adults are likely to have been drivers or passengers in an RTA, children are more likely to have been a pedestrian who has been struck by a vehicle. The high energy that produces these injuries may also result in visceral and vascular injury, which can be fatal. Mortality associated with pelvic fractures in children is lower than that of adults at about 5% (Ismail et al. 1996). The likelihood of associated injuries is higher in those with multiple fractures of the pelvic ring and those with unstable fractures are more likely to have greater resuscitation requirements. Resuscitation takes priority. In the past, pelvic injuries were managed non-operatively, using compression devices, plaster casts and bed rest. Over time, outcome studies have demonstrated that post-traumatic anatomic deformities and pelvic instability correlated with persistent pain and functional limitation (McCormack et al. 2010).
Classification of Pelvic Injury
There are several types of pelvic injury classification (Table 9.3). Torode and Zieg (1985) used a four-part classification based on radiological findings:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


