Carline A. Dalgleish, Sharon Oliver and Alexandra Patricia Adams 1. Define, spell, and pronounce the terms listed in the vocabulary. 2. Describe the steps for abstracting procedural data from clinical documentation. 3. Identify four purposes of the CPT. 4. List the six main sections of the CPT and describe their content. 5. Describe the coding conventions, guidelines, and layout of the CPT manual and their importance. 6. Describe the process and steps for selecting the most accurate code based on clinical documentation. 7. Explain the importance of correctly assigning Evaluation and Management (E/M) codes. 8. Discuss the importance of modifiers. 9. Define upcoding and explain why it must be avoided. 10. Explain the process for selecting the correct procedure codes. 11. Explain the process for selecting main and modifying terms. 12. Explain how to find codes in the Alphabetic Index of the CPT manual. 13. Explain how to analyze and select codes using the CPT Main Text. acronyms Abbreviations, such as ECG for electrocardiography. add-on codes Codes that indicate additional or supplemental procedures carried out along with the primary procedure. Alphabetic Index The reference section of the CPT manual; it is used to help find a code or code range. Category I codes Five-digit primary procedure or service codes, found in the Tabular Index, that are selected when performing insurance billing or statistical research. Category II codes Special codes that can help providers track revenue and reimbursement; these codes are alphanumeric and end in the letter F. Category III codes Codes for a new or experimental procedure or service, otherwise referred to as “Emerging Technology”; these codes are alphanumeric and end in the letter T. established patient (EP) A patient who has received professional services (face to face) from the physician, or from another physician of the exact same specialty and subspecialty who belongs to the same group practice, within the past 3 years. Main Text See Tabular Index. modifying terms Key words selected after the main term has been chosen to help further define or describe the procedure or service performed. patient status (PS) The state of a patient as either new or established; appears in the Evaluation and Management section of the CPT. physical status The physical condition of the patient. place of service (POS) codes Codes used on professional claims to specify the facility or location where the service or services were rendered. section One of the six primary divisions of the main body of the CPT. unbundled codes Codes in which the components of a major procedure are separated and reported separately. Sherald Vogt excelled on her diagnostic coding examinations, and she now looks forward to learning procedural coding. The process for coding procedures and services will prove to be similar to that of ICD-9-CM and diagnostic coding, except she will use a different coding manual, the Current Procedural Terminology (CPT), for most procedural and services rendered coding. She will also use the Healthcare Common Procedural Coding System, or HCPCS (pronounced “hic-pix”) manual. As with the ICD-9-CM, accurate coding begins with the proper analysis of clinical information to abstract the correct data and accurately assign a procedure or service code. In the ICD-9-CM, she learned about coding conventions and guidelines. The CPT also has conventions, symbols, guidelines, and formal steps specific to procedural coding that Sherald will use to correctly assign procedure codes. Sherald is beginning to fully understand the impact diagnostic and procedural coding has on reimbursement, and her responsibility to uphold ethical standards when coding to keep her employers, Dr. Shuman, Dr. Taylor, and Dr. Caddell, in compliance with federal and state guidelines. She is excited to begin this new phase of her education and to have the opportunity to learn more skills, which will help her reach her goal of becoming an even more valuable asset to the practice. While studying this chapter, think about the following questions: • What will help Sherald in selecting the most specific and accurate CPT code? • What are the differences between coding for the CPT and coding for HCPCS? • What will Sherald learn about the legal and compliance implications of improper coding? Procedural coding is defined as the transformation of verbal descriptions of medical services and procedures into numeric or alphanumeric designations. As with diagnostic coding and use of the ICD-9-CM manual, the medical assistant must develop meticulous accuracy when using the Current Procedural Terminology (CPT) manual, developed by the American Medical Association (AMA), and the Healthcare Common Procedural Coding System (HCPCS), developed by the Centers for Medicare and Medicaid Services (CMS). The medical assistant facilitates accurate medical recordkeeping and efficient processing of insurance claims by using the CPT and HCPCS, which identify appropriate procedures and services common to the physician’s office. CPT and HCPCS (discussed later in the chapter) are used in the claims submission process to obtain reimbursement from payers, to track physicians’ productivity, and to provide statistical data for research and other purposes. The CPT manual is a list of descriptive terms and identifying codes for reporting medical services and procedures performed by physicians. The CPT provides a uniform, or standard, language that accurately describes medical, surgical, and diagnostic services and enhances reliable communication among physicians, patients, and third parties. The manual was developed after the AMA recognized a need for a standardized description of services that would be universally understood by physicians, hospitals, insurance companies, and all involved in the reimbursement or statistical data collection process. The second edition of the CPT, published in 1970, presented an expanded system of terms and codes to designate diagnostic and therapeutic procedures in surgery, medicine, radiology, laboratory, pathology, and medical specialties. At that time, the four-digit classification was replaced with the current five-digit coding system. The fourth edition was published in 1977 and included significant updates in medical technology. At the same time, a system of periodic annual updating was introduced to keep pace with the rapidly changing environment. The fourth edition is still in use today; however, at this writing, the AMA is in the process of developing the fifth edition of the CPT, the first major revision since 1977. The CPT uses a five-digit classification system that is designed to do the following: • Encourage the use of standard terms and descriptors to document procedures in the medical record • Provide the basis for a computer-oriented system to evaluate operative procedures • Contribute basic information for actuarial and statistical purposes Before continuing, consider this important fact: there are roughly 150,000 procedure and service codes in the CPT manual and thousands more in the HCPCS manual. Memorizing the codes for each specific procedure and service would be impractical, if not impossible. Instead, the key to success is learning how to use the coding manuals to find the most specific and accurate code based on interpretation of the medical record. This requires a solid understanding of medical terminology, anatomy, and physiology and a knowledge of how to use the CPT manual and its symbols, conventions, guidelines, and notes. The goal of this chapter is to teach the skills, processes, and decisions required to use the CPT and HCPCS manuals. Remember, the CPT and HCPCS manuals for the current year are always the final authority. The symbols, guidelines, conventions, and other instructions found in the CPT manual contain all the information needed to select the correct code for the procedure or service documented in the medical record. The CPT code is a five-digit code also known as a Category I code. Category I codes are located in the Tabular Index (also called the Main Text) of the CPT manual and arranged by sections. For example, codes beginning with 7 (e.g., 70100—a radiologic examination of the mandible, partial, with less than four views) are located in the Radiology section of the manual. Each code has a description of the service or procedure performed. Some CPT codes (e.g., Category II and Category III codes, discussed later) are alphanumeric. Occasionally, a new vaccine is assigned a Category I code before the Food and Drug Administration (FDA) has approved the vaccine for use. These vaccines are listed in Appendix K and are identified in the Tabular Index of the CPT in various ways by different publishers. Some publishers use the letter P (approval pending); others use a lightning bolt symbol ( Bundled codes indicate procedures or services that are grouped together and paid for as one procedure or service, as designated by the NCCI edits. If bundled codes are separated and used individually, a special report should be used to describe the circumstances that made the unbundling necessary. Unbundled codes are used when the components of a major procedure are separated and reported separately. Category II codes are a set of supplemental tracking codes that can be used for performance measurement. Category II codes are optional; they cannot be used as a substitute for Category I codes, and they are not reported as part of the billing process. Providers can use Category II codes to help measure performance and outcomes. These codes describe clinical components that may be typically included in Evaluation and Management services or clinical services. No relative value is associated with them. In a Category II code, the fifth digit is the letter F. Category II codes are described and listed in Appendix H of the CPT manual. They are listed in alphabetic order by condition instead of numerically. Category II codes are reviewed by the Performance Measures Advisory Group, which is composed of members from various medical organizations and government agencies. In some publisher’s editions of the CPT manual, Category II codes are also listed in their own section immediately after the Medicine section and before the appendixes. Category III codes are temporary codes assigned for emerging and new technology, services, and procedures that have not been officially added to the Main Text of the CPT manual. In a Category III code, the fifth digit is the letter T. Category III codes may be used in billing and reporting if no code in the Main Text accurately describes the technology, service, or procedure performed, and no Category I code matches the medical documentation. Category III codes have no reimbursement value. In most publisher’s editions of the CPT manual, Category III codes are also listed in their own section immediately after the Medicine section and before the appendixes. Modifiers (Table 19-1) give providers a means of indicating that a service or procedure performed was altered by some specific circumstance but was not changed in its definition. Two- or five-digit alphanumeric modifiers, included with the five-digit CPT code, can be used to supply additional information or to describe extenuating circumstances that affect the rendered procedure or service. For instance, modifier -50 adds the detail that a procedure was performed bilaterally, or on both sides of the body. For example, the code 99050 is used to describe care provided after normal business hours. To describe a situation in which an assistant surgeon is needed for a surgical procedure, modifier -80 can be used to allow the assistant surgeon to submit charges for his or her time and services (code 99080 describes a special report). TABLE 19-1 Commonly Used CPT Code Modifiers The modifiers for HCPCS are codes composed of two alphanumeric characters. Like the modifiers for CPT Category I codes, the HCPCS modifiers do not change the description of the code, but rather provide additional information or describe extenuating circumstances. In the CPT manual, each procedure or service is represented by a five-digit numeric code (Figure 19-1), a type of medical shorthand that saves enormous amounts of time and effort and helps to ensure accuracy of information. Just imagine, for example, if a billing department had to describe, in writing, every single one of the medical procedures and services represented by the codes in the CPT manual. Preparing one bill for one patient could take an hour or longer, and problems with reimbursement still would arise if the health insurance or third-party payer had additional questions or, worse, reduced or even denied payment based on its interpretation of the written narrative. In most instances, using the five-digit CPT codes eliminates the need for written descriptions, thus assuring clear communication, and the standardization of codes ensures that everyone in the reimbursement cycle understands exactly what procedure or service was provided to the patient. In addition, these codes enable automated computer processing of claims, which also saves time and effort. The CPT manual generally includes the following content, depending on the publisher: • Comprehensive instructions for use of the manual, including steps for coding • The Main Text (Tabular Index), composed of: The CPT has two primary divisions, the Alphabetic Index and the Main Text (Tabular Index). The Alphabetic Index is like any other index in a textbook; it is simply a guide to finding data in the body of the textbook. However, instead of providing the page numbers where the information is located, as a typical index does, the CPT’s Alphabetic Index lists the code or code ranges, which are arranged in numeric order in each section of the Main Text. The Tabular Index (Main Text) is divided into six broad categories, or sections, with codes listed in numeric order in each section. Like the ICD-9-CM, the codes in the Tabular Index include definitions, guidelines and notes, which enable the coder to select the most specific code or codes based on the procedures and services descriptions documented in the medical record. The six sections of the Tabular Index include: Each of the six sections reflect the general type of service. Sections are subdivided into subsections; subsections are further divided into categories; and categories can be subdivided into subcategories. Each level of a section provides more specificity regarding the procedure or service performed and the anatomic site or organ system involved (Table 19-2). In most instances, all four levels are found, although this is not a hard and fast rule. TABLE 19-2 Section, Subsection, Category, and Subcategory Examples In the CPT manual, the subsection is listed below the section and indented two spaces. The subsection usually describes an anatomic site or an organ system, as in the following examples: A category is listed below the subsection and indented two spaces. It generally refers to a specific procedure or service, but it can also indicate a more specific anatomic site: • Procedures: esophagoscopy, incision and drainage, or cardiac catheterization • Specific anatomic site: mitral valve, distal femur, or occipital bone Subcategory is the lowest level of code description. The subcategory is listed below the category and indented two spaces. It provides even more specificity about an anatomic site or the procedure or service performed. The Evaluation and Management (E/M) section contains codes for the different types of encounters or visits patients have with providers; these encounters may include office, hospital, and emergency department visits; consultations; and physician contact with patients in intensive care units, skilled nursing facilities, nursing homes, and other facilities. The code range in the E/M section is 99201 to 99499. The E/M section is further divided into subsections that include different types of services (e.g., office visits, hospital visits, consultations, skilled nursing facility, or nursing home visits). The subcategories of E/M services are further classified into levels of E/M services that are identified by specific codes. This classification is important, because the nature of a physician’s work varies by type of service, place of service, and the patient status. The subsections, categories, and subcategories are written to further modify or describe the service or procedure performed. The Anesthesia section includes codes for anesthesia services rendered by anesthesiologists and anesthetists before, during, and after surgery. The code ranges in the Anesthesia section are 00100 to 01999 and 99100 to 99140. Codes are included for the types of anesthesia administered (e.g., general, local, and sedation anesthesia); other support services, including the anesthesiologist’s preoperative and postoperative encounters with the patient, evaluation of the patient’s physical status, and the administration of anesthesia, fluids, and/or blood; and monitoring services, such as blood pressure, temperature, and electrocardiography (ECG). Unusual forms of monitoring (e.g., intra-arterial, central venous, and Swan-Ganz) are not included and can be billed separately. The Surgery section, the largest section of the CPT, includes standardized codes for all invasive surgical procedures performed by physicians. An invasive procedure is defined as any medical procedure in which a bodily orifice or the skin must be penetrated by cutting, puncture, or other method. This section is divided into subsections typically identifying specific body systems, beginning with the integumentary (skin) system and ending with the ophthalmologic (eye) and otologic (ear) systems. In most instances, each subsection is further divided into categories and subcategories, which describe procedures and services unique to that anatomic subsection. The Radiology section includes codes for diagnostic imaging, including x-ray studies and scans, and for therapy used in the treatment of cancer. The code range in the Radiology section is 70000 to 79999. Codes are included for all diagnostic tests performed on bodily fluids and tissue, including urine, blood, sputum, and feces, as well as excised or biopsied cells, tissue, or body organs; and for evaluation of those fluids and tissues to identify any pathology or disease present. The code ranges for the Pathology and Laboratory section are 80047 to 80076 for Organ or Disease–Oriented Panels and 80100 to 89999 for all other tests. The codes for the Medicine section range from 90281 to 99199 and 99500 to 99607 (excluding the anesthesia code ranges described in the Anesthesia section). The Medicine section includes many and varied subsections, categories, and subcategories. This section can be considered a catchall section in that it includes codes for services and procedures that do not fit into any of the other sections of the CPT manual. Medical specialties, such as ophthalmology, otolaryngology, and allergy, which involve procedures and services that vary greatly from the traditional office encounter, are grouped in the Medicine section rather than the E/M section. Noninvasive diagnostic tests are included in the Medicine section rather than in the Surgery section, which typically includes only invasive procedures. Conventions (Figure19-2) are special symbols used to provide additional information about certain codes. Examples of conventions include triangular and round symbols, which indicate that a code or description was revised, removed, or added. A plus sign (+) indicates an add-on code. Codes with a plus sign are additional codes that must be used with certain Category I codes. For example, one of the codes in the Surgery section, Integumentary subsection, is +15401. Code 15401 describes “each additional 100 sq. cm.…” Just above code 15401 is code 15400, which describes a “xenograft of the skin… the first 100 sq. cm. or less…” If the medical documentation states that a “200 sq. cm. xenograft of the skin” was performed, the medical assistant would code the first 100 sq. cm. using code 15400, and the second 100 sq. cm. by using add-on code 15401 (+15401). Another example of a symbol convention is a circle with a small round dot in the center. This symbol indicates that conscious sedation, rather than a general anesthetic, was used during a surgical procedure. In most CPT manuals, the legend explaining the meanings of the convention symbols is found at the bottom of each page of the Tabular Index. Guidelines, which are found at the beginning of each section and some subsections of the CPT manual , add definitions and descriptions necessary to appropriately interpret and report the procedures and services in that section or subsection. For example, in the Medicine section, specific instructions are provided for handling unlisted services or procedures, special reports, and supplies and materials provided to the insurance company or the patient (Figure 19-3). Guidelines are written to assist in understanding when and under what circumstances codes may be used. It is important to thoroughly read and understand the guidelines provided throughout the Main Text. This is especially important when first learning to code, or working in a section of the CPT that is rarely used. It is also important to reread the guidelines after the CPT annual revisions, additions, and deletions, are effective January of each year. Selecting a code without reading the guidelines will usually lead to selection of the wrong code. Not only will this result in the potential for delayed or denied reimbursement, but continued inappropriate code selection can be considered fraud or abuse and can result in serious civil or criminal penalties. Notes are typically found only in the category, subcategory, or code description area of the CPT. They apply only to the designated group of codes following the note and (unlike guidelines) not to the whole section. As do guidelines, notes provide additional information to assist in the selection of specific codes. Occasionally, even with the best documentation and the coder’s best efforts, an accurate, specific code to match the procedure or service performed cannot be found in the CPT manual . In each section (and sometimes in subsections, categories, and/or subcategories), nonspecific codes have been provided. These codes are called Unlisted Procedures and Services. For example, code 29999 is found in the Surgery section, Musculoskeletal subsection. It describes an “unlisted procedure, arthroscopy.” Unlisted codes can be used only when no Category I or Category III code provides an exact match to the medical documentation. When an unlisted code is used, a Special Report must be sent with the insurance claim that describes the procedure or service thoroughly. When bills are submitted for services rendered or procedures performed, most insurance carriers or third-party payers require no additional information on the insurance claim form other than the procedure or service CPT code. When a bill is submitted for a service that is unlisted, unusual, or newly adopted, the third-party carrier requires a special report so that the company can determine whether provision of that service or procedure was medically appropriate. The following appendixes are found in the CPT manual. The steps for using the CPT manual actually begin not in the CPT coding manual but in the medical documentation. Information pertinent to code selection is taken from a variety of medical documents. Sources of information include the following: • Encounter form (also called a superbill, fee slip, or charge ticket) • History and physical report (H&P) These documents were discussed in earlier chapters, and examples were given. Although these same forms are used for CPT coding, the information abstracted is different (as shown later in the chapter). As in ICD-9-CM coding, when the medical documentation is compared against any code description, all the elements of that code must substantially match, with nothing added or missing. Many providers have CPT and ICD-9-CM codes preprinted on their encounter forms or charge tickets. However, it is important also to review the medical record carefully and compile an abstract of all the procedures and services rendered during an encounter. For example, on the encounter form, a provider checks off the procedure for a esophagogastroduodenoscopy (EGD); however, when the medical assistant reviews the medical record, he discovers that the operative report states that an EGD with biopsy was performed. If the medical assistant had not reviewed the medical record, a code with a lower reimbursement amount for the procedure would have been submitted to the insurance carrier, and the provider would have lost revenue. Update encounter forms annually to ensure that code additions, changes, and revisions appear on the preprinted forms. The coding steps and process outlined in this chapter, including use of the Alphabetic Index and the Main Text of the CPT, apply to all sections of the CPT manual. Some special considerations and differences apply to the E/M and Anesthesia sections. The basic steps in medical coding are to (1) read, analyze, and abstract the procedure or service documented in the medical record and (2) compare it with the encounter form, operative report, or other documentation to ensure that all services and procedures have been recorded. The term abstract, used as a verb in this context, means to create an outline or summary of information from a text or record. In procedural coding, an abstract is created to find all the procedures and services performed during a patient encounter and also to ensure that nothing has been omitted from or added to the encounter form or charge ticket that is not documented in the medical record. The abstracted data are then broken down into main terms and modifying terms. A main term is usually the primary procedure or service performed, and a modifying term further defines or adds information to the main term. Next, the main and modifying terms are used to find the code or code ranges in the Alphabetic Index. Last, the code selected is confirmed by reviewing the guidelines, notes, and conventions in the Main Text to verify that the most accurate code has been chosen. The Alphabetic Index is a comprehensive, alphabetic listing of all procedures and services in the CPT manual. Medical assistants must keep in mind the most important fact about the Alphabetic Index: it should be used only as an aid to finding the area in the Main Text to evaluate for selecting the proper code. The Alphabetic Index is not a substitute for the Main Text. Even if only one code is assigned, the Main Text must be used to ensure that the code selection is accurate. The Alphabetic Index is used as a guide to search for one or more codes or code ranges. The index is similar to that found in any textbook; it is an alphabetic list of main and modifying terms found in the Main Text of the coding manual. In a typical index, the term or concept listed in the index is followed by a reference page or pages, where detailed information is presented in the body of the book. The Alphabetic Index in the CPT is used in the same way, except that it references codes or code ranges rather than pages. As discussed earlier, the Main Text is divided into sections, and the procedures and services are listed in numeric order by the Category I code. The Alphabetic Index is organized by main terms that can stand alone. The CPT code set has been developed as stand-alone descriptions of medical procedures. Some of the procedures in the CPT are not printed in their entirety but refer back to a common portion of the procedure listed in a preceding entry. This is evident when an entry is followed by one or more indentations. This is the part before the semicolon (;) in the description. Do not confuse the two-digit modifiers discussed earlier in the chapter with modifying terms. Modifiers are numeric supplements to a Category I code, whereas modifying terms are words that add to or modify the meaning of the main term. Modifying terms are indented two spaces below the main term. They further describe or add information or a definition needed to narrow the search for an appropriate procedure or service code. A main term might be a procedure, such as an excision, and each modifying term could provide further information about the anatomic location or the organ excised, the type of instrument used, or a special technique, or whether other procedures were performed at the same time as the excision, such as obtaining biopsy tissue for examination. Modifying terms affect the selection of appropriate codes; therefore, it is important to review the list of modifying terms when selecting a code or code range. Consider the examples presented in Table 19-3. If the medical documentation contains the narrative description of a procedure as a “diagnostic cystoscopy,” the main term is Cystoscopy; the modifying term is diagnostic, because it describes the type of cystoscopy performed. Another example is “esophagogastroscopy with biopsy and fulguration of lesions.” In this example, the main term is Gastroscopy (the procedure performed), and the modifying terms are esophago- (which adds another anatomic site scoped at the same time as the gastroscopy); with biopsy and fulguration (two additional procedures performed during the gastroscopy); and lesions (describes the object of the biopsy and fulguration). TABLE 19-3 Identification of Main and Modifying Terms in the Alphabetic Index
Basics of Procedural Coding
Learning Objectives
Vocabulary
Scenario
Getting to Know the CPT
The Evolution of CPT Coding
Purpose of CPT Procedural Coding
The CPT Code
Category I Codes
Product Pending U.S. Food and Drug Administration Approval
 ) in various colors to designate the pending FDA approval. These codes are tracked by the AMA to monitor FDA approval status. When the FDA status changes to approval, the lightning bolt symbol (
) in various colors to designate the pending FDA approval. These codes are tracked by the AMA to monitor FDA approval status. When the FDA status changes to approval, the lightning bolt symbol ( ) or other “pending” identifier is removed.
) or other “pending” identifier is removed.
Bundled Codes
Unbundled Codes
Category II
Category III
Modifiers
MODIFIER
DESCRIPTION
-50
Bilateral procedure. If procedure was performed on both sides of the body (e.g., both knees, both eyes) and code description does not indicate that the procedure or service was performed bilaterally, modifier -50 is used.
-62
Two surgeons. When two surgeons work together as primary surgeons performing distinct parts of a procedure, each surgeon should report the procedure he or she performed to the insurance carrier and use modifier -62. (This prevents the insurance carrier from possibly rejecting a surgical charge as a duplicate.)
Format of the CPT Coding Manual
CPT Content
The Indexes
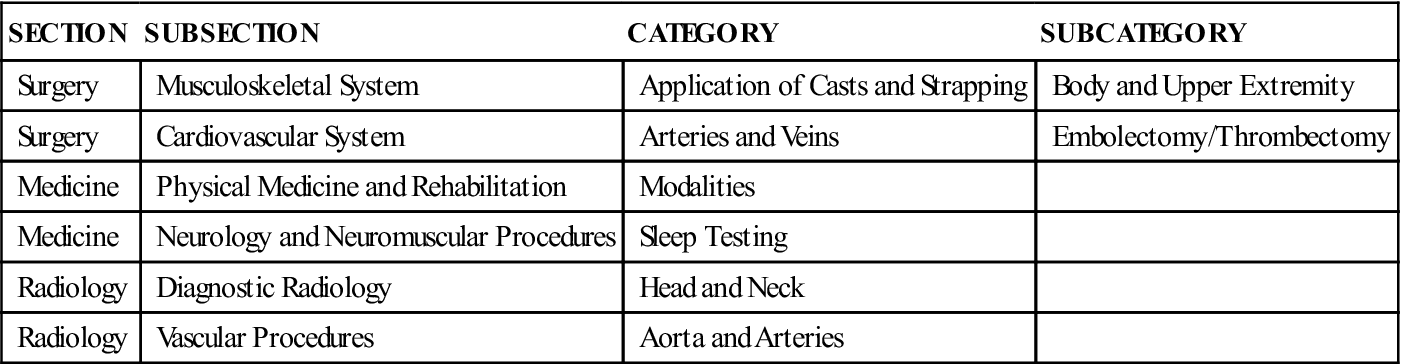
Main Text
SECTION
SUBSECTION
CATEGORY
SUBCATEGORY
Surgery
Musculoskeletal System
Application of Casts and Strapping
Body and Upper Extremity
Surgery
Cardiovascular System
Arteries and Veins
Embolectomy/Thrombectomy
Medicine
Physical Medicine and Rehabilitation
Modalities
Medicine
Neurology and Neuromuscular Procedures
Sleep Testing
Radiology
Diagnostic Radiology
Head and Neck
Radiology
Vascular Procedures
Aorta and Arteries
Evaluation and Management Section
Anesthesia Section
Surgery Section
Radiology Section
Pathology and Laboratory Section
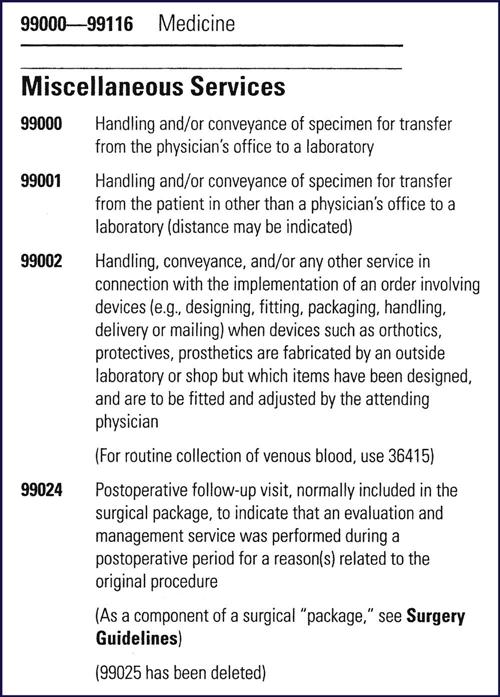
Medicine Section
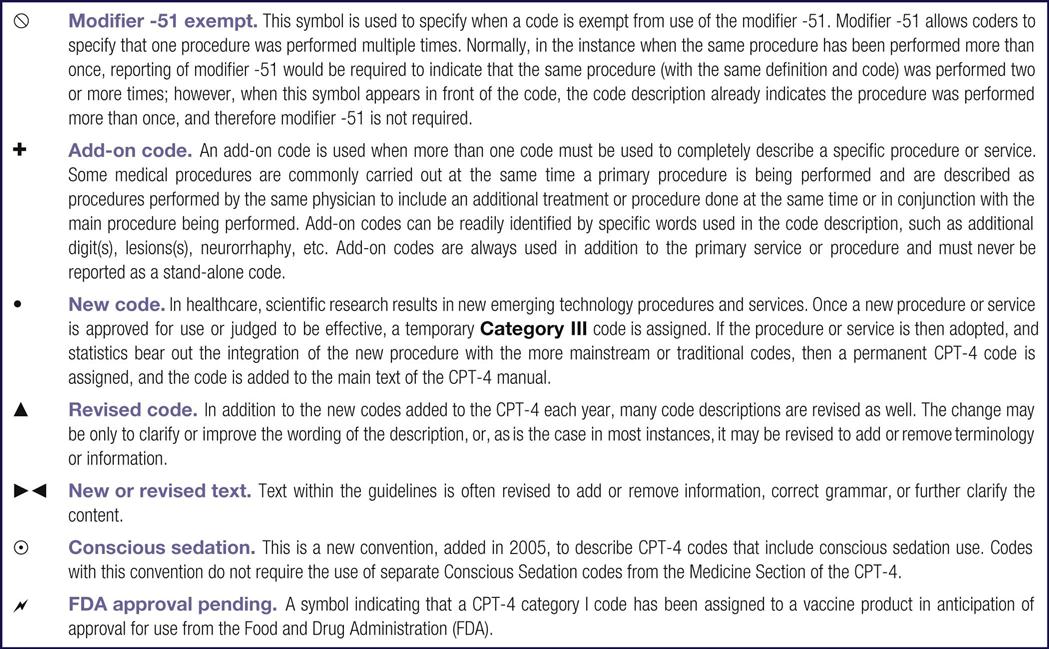
Conventions of the CPT Main Text
Guidelines
Notes
Unlisted Procedure or Service Code
Special Reports
Appendixes
Beginning the Coding Process
Medical Documentation
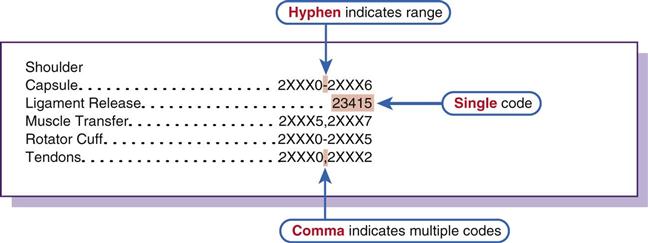
Using the Alphabetic Index
MODIFYING TERMS
CODE
MAIN TERM(S)
FIRST
SECOND
THIRD
FOURTH
Cystoscopy
Diagnostic
Gastroscopy
Esophago-
With biopsy
With fulguration
Of lesions
492000
Cyst
Abdomen
Ankle
Bartholin’s gland
Bile duct
21030
Excision
Cheekbone
23140
Clavicle
23146
With allograft
23147
With autograft
27355-27758
Femur
Cyst excision: 49200
Cyst excision of clavicle: 23140
Cyst excision of clavicle with allograft: 23146
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access