Chapter 21 Bacterial Diseases
Insider’s Guide to Bacterial Diseases for the USMLE Step 1
There is no better way to say it: the USMLE loves bacterial diseases! This is one of the highest-yield subjects on the examination, so you must know it well! Our book has divided microbiology into two chapters, but you should note that the breakdown of the examination is not likely to be evenly distributed among bacteria, viruses, fungi, and parasites. Bacterial diseases are tested far more commonly than the other three types, but recently, fungal diseases have been heavily represented on many students’ forms. Fungal diseases are discussed more in Chapter 22.
Basic Concepts
1 What makes an organism gram-positive or gram-negative?
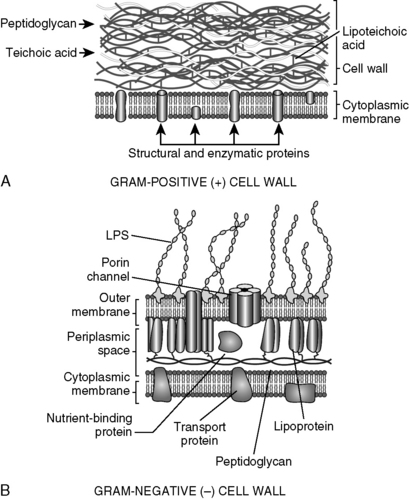
Both gram-positive and gram-negative organisms have an internal cell membrane and cell walls made of peptidoglycan. However, gram-negative bacteria have much thinner cell walls and, in addition, have an outer membrane outside the cell wall. Gram-positive organisms have techoic acid in their cell walls, and gram-negative organisms have lipopolysaccharide (endotoxin) (Fig. 21-1).
3 Describe the mechanism by which lipid A causes toxicity?
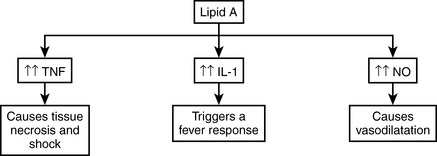
Lipid A activates macrophages to secrete interleukin 1 (IL-1) and tumor necrosis factor (TNF), both of which are referred to as acute-phase cytokines. Lipid A also stimulates the release of nitric oxide (NO) from endothelial cells. Large amounts of lipid A may lead to shock and intravascular coagulation via this stimulatory effect (Fig. 21-2).
7 Identify the Gram stain and the morphology of the organisms in Table 21-1
| Image | Gram Stain and Morphology |
|---|---|
 Gram stain of a sputum sample infected with Streptococcus pneumoniae. Gram stain of a sputum sample infected with Streptococcus pneumoniae. | Gram-positive cocci in pairs: S. pneumoniae |
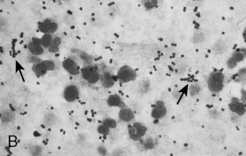 Expectorated sputum with gram-negative rods in a patient with Klebsiella pneumoniae pneumonia. Expectorated sputum with gram-negative rods in a patient with Klebsiella pneumoniae pneumonia. | Gram-positive cocci (staining purple in a color image) in chains: Staphylococcus aureus |
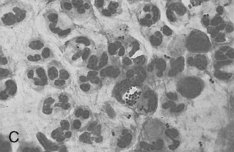 Sputum smear, stained with Gram stain, shows many neutrophils and intracellular gram-negative diplococci, suggestive of Neisseria meningitidis infection (oil immersion). Sputum smear, stained with Gram stain, shows many neutrophils and intracellular gram-negative diplococci, suggestive of Neisseria meningitidis infection (oil immersion). | Gram-negative cocci (staining pink in a color image) in pairs: Neisseria spp. |
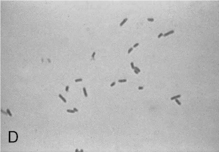 | Gram-negative rods: many possibilities |
Klebsiella pneumoniae image from Mandell GL, Bennett JE, Dolin R: Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, 7th ed. Philadelphia, Churchill Livingstone, 2009. Images of Streptococcus pneumoniae, Neisseria meningitidis, and gram-negative rods from McPherson RA, Pincus MR: Henry’s Clinical Diagnosis and Management by Laboratory Methods, 22nd ed. Philadelphia, WB Saunders, 2011.
8 Cover the two columns on the right in Tables 21-2 through 21-9 to test your knowledge of the properties of the clinically relevant bacteria listed in the left column
Table 21-2 Gram-Positive Cocci
| Organism | Associated Disease(s) | Pearls to Remember |
|---|---|---|
| Staphylococcus aureus | Cellulitis Acute endocarditis (in previously normal valve) Osteomyelitis Pneumonia Carbuncles/furuncles Stye (hordeolum) | Toxin-mediated diseases: Staphylococcal toxic shock Scalded skin syndrome Staphylococcal gastroenteritis Note: Like all staphylococcal species, S. aureus is catalase-positive—but it also is coagulase-positive. |
| Staphylococcus epidermidis | Prosthetic valve endocarditis | Normal skin flora Novobiocin-sensitive |
| Staphylococcus saprophyticus | Cystitis in young women Second most common cause of UTI (behind E. coli) | Novobiocin-resistant |
| Streptococcus agalactiae (group B streptococci) | Neonatal pneumonia, meningitis, sepsis Chorioamnionitis | Normal vaginal flora β-Hemolysis Bacitracin-resistant |
| Streptococcus pneumoniae | Pneumonia Meningitis Sinusitis Otitis media | Bile-soluble Optochin-sensitive α-Hemolysis See Case 21-1 for more details |
| Streptococcus pyogenes (group A streptococci) | Pharyngitis Impetigo Erysipelas Cellulitis Necrotizing fasciitis Rheumatic fever Poststreptococcal glomerulonephritis | Remains largely sensitive to penicillin β-Hemolysis Bacitracin-sensitive |
| Enterococcus spp. | UTI Bacteremia/sepsis Endocarditis Abdominal abscess | Part of normal bowel flora that causes disease when host is immunocompromised or gastrointestinal tract has been breached α- or γ-Hemolysis |
| Viridans streptococci | Dental caries (S. mutans) Subacute bacterial endocarditis (S. sanguis) | Normal oral flora α-Hemolysis Optochin-resistant |
UTI, urinary tract infection.
Table 21-3 Gram-Positive Bacilli
| Organism | Associated Disease(s) | Pearls to Remember |
|---|---|---|
| Bacillus anthracis | Cutaneous anthrax (most common form) Pulmonary anthrax | Painless black eschars with cutaneous anthrax Wool-sorters at risk for pulmonary anthrax (“wool-sorter’s disease) Spore-forming |
| Corynebacterium spp. | Diphtheria Granulomatous lymphadenitis Pneumonitis Pharyngitis Skin infections Endocarditis | Normal skin flora Pseudomembrane or esophageal web Toxin causes disease and is encoded by β-prophage Metachromatic granules ADP ribosylation of EF-2 |
| Listeria monocytogenes | Listeriosis | Perinatal/neonatal infections Immunocompromised persons at risk Raw milk and dairy products |
ADP, adenosine diphosphate; EF-2, elongation factor.
Table 21-4 Gram-Negative Cocci
| Organism | Associated Disease(s) | Pearls to Remember |
|---|---|---|
| Neisseria meningitidis (meningococcus) | Meningitis Septicemia Waterhouse-Friderichsen syndrome | Has a capsule Purpuric nonblanching rash Vaccine available See Case 21-8 |
| Neisseria gonorrhoeae (gonococcus) | Infects superficial mucosal surfaces lined with columnar epithelium: Urethra: urethritis (gonorrhea) Vagina: vulvovaginitis in young girls Rectum: proctitis Conjunctiva: ophthalmia neonatorum | No vaccine Main cause of infectious arthritis in sexually active persons Prepubescent vaginal epithelium is columnar because not yet acted on by estrogen to become squamous |
Table 21-5 Enteric Gram-Negative Rods
| Organism | Associated Disease(s) | Pearls to Remember |
|---|---|---|
| Campylobacter jejuni | Enteritis | Present in animal feces |
| Escherichia coli | Enteritis UTI Meningitis Peritonitis Mastitis Septicemia Gram-negative pneumonia HUS | Normal gut flora E. coli O157:H7—a particularly virulent pathologic strain associated with HUS See Case 21-2 |
| Salmonella spp. | Food-borne illness Typhoid fever (Salmonella typhi) | Osteomyelitis in patients with sickle cell anemia |
| Shigella spp. | Shigellosis (bacterial dysentery) | Bloody diarrhea Fecal oral route of transmission Low inoculum required Toxin-mediated |
| Helicobacter pylori | Peptic ulcer disease Gastritis Duodenitis Gastric cancer Mucosa-associated lymphoid tissue (MALT) lymphoma | Positive urea breath test due to presence of enzyme urease Lives in stomach but common in duodenal ulcers Triple treatment: amoxicillin, clarithromycin, and proton pump inhibitor |
HUS, hemolytic uremic syndrome; UTI, urinary tract infection.
Table 21-6 Other Gram-Negative Rods
| Organism | Associated Disease(s) | Pearls to Remember |
|---|---|---|
| Bordetella pertussis | Pertussis (whooping cough) | Highly contagious; spread by coughing and nasal drops |
| Brucella spp. | Brucellosis (also called “undulant fever”) | Transmitted via contaminated or unpasteurized milk |
| Francisella tularensis | Tularemia (“rabbit fever”) | Reservoir in rabbits; transmitted by tick Symptoms/signs similar to those of plague Culture, drainage contraindicated owing to high virulence |
| Haemophilus influenzae | Meningitis (type b) Bacteremia Cellulitis Pneumonia Sinusitis | Type b encapsulated and more virulent Vaccine available for type b strain |
| Pseudomonas aeruginosa | Pneumonia in cardiac failure patients External otitis Osteomyeltis in diabetics Endocarditis UTI Hot tub folliculitis | Think Pseudomonas infection in burn patients and intravenous drug users Can cause black skin lesions Cultures make blue-green pigment Has endotoxin A Resistant to many antibiotics |
| Legionella pneumophila | Legionnaire’s disease Pontiac fever | Legionnaire’s disease: acute pneumonia with multisystem involvement; from water source, so no person-to-person spread Pontiac fever: similar to flu |
| Yersinia pestis | Bubonic plague | Transmitted by fleas from rodents to humans Black buboes |
| Yersinia enterocolitica | Enterocolitis | Pseudoappendicitis Seen in nursery schools |
| Organism | Associated Disease(s) | Pearls to Remember |
|---|---|---|
| Clostridium perfringens | Anaerobic cellulitis Gas gangrene (myonecrosis) Food poisoning | Crepitus is associated with gas gangrene Alpha toxin (lecithinase) |
| Clostridium tetani | Tetanus | Exotoxin that causes spastic paralysis by blocking glycine release from Renshaw cells in spinal cord Vaccine is available |
| Clostridium botulinum | Botulinism | Food poisoning that causes flaccid paralysis Preformed toxin prevents release of ACh Classic scenario from consumption of dented canned goods or honey |
| Clostridium difficile | Pseudomembranous colitis | Caused by antibiotic use, especially clindamycin or ampicillin Treat with metronidazole or oral vancomycin |
ACh, acetylcholine.
| Organism | Associated Disease(s) | Pearls to Remember |
|---|---|---|
| Borrelia burgdorferi | Lyme disease | See Case 21-5 |
| Borrelia recurrentis | Relapsing fever | Organism switches surface proteins to evade immune response, leading to intermittent fevers |
| Treponema pallidum | Syphilis | See Case 21-4 |
| Leptospira interrogans | Leptospirosis | Transmitted by water that is contaminated by animal urine through cracks in the skin, eyes, or mucous membranes |
Table 21-9 Intracellular Organisms
| Organism | Associated Disease(s) | Pearls to Remember |
|---|---|---|
| Mycoplasma pneumoniae | Atypical (“walking”) pneumonia | No cell wall Treat with macrolides Blood shows IgM “cold agglutinins” Chest radiograph demonstrates diffuse interstitial infiltrates; radiographic changes often more extensive than expected from patient’s symptoms |
| Chlamydia trachomatis | Urethritis Pelvic inflammatory disease Blindness Lymphogranuloma venereum Neonatal conjunctivitis | See Case 21-7 Treat neonates with erythromycin eye drops for conjunctivitis |
| Chlamydia psittaci | Psittacosis (flu-like syndrome) | Transmitted from bird droppings via aerosol |
| Chlamydia pneumoniae | Atypical pneumonia | Transmitted via aerosols |
| Mycobacterium tuberculosis | Tuberculosis | See Case 21-6 |
| Mycobacterium leprae | Leprosy (Hansen’s disease) | Tuberculoid form: milder with few organisms in lesions Lepromatous form: severe with many organisms in lesions Grows in cool temperatures, so affects distal sites Treat with dapsone |
| Rickettsia rickettsii | Rocky Mountain spotted fever | Rash that starts on palms and soles and migrates centrally (centripetal migration) Weil-Felix test results positive for rickettsial diseases |
Basic concepts in antibacterial pharmacology
1 What are the β-lactam antibiotics and what is their mechanism of action?
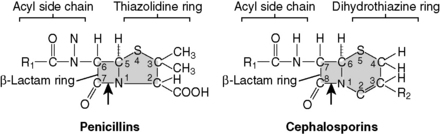
The β-lactam antibiotics include the penicillins, cephalosporins, and carbapenems (imipenem, meropenem). By virtue of their β-lactam chemical moiety, they all inhibit bacterial cell wall synthesis. Resistance to these antibiotics is mediated by bacterially synthesized β-lactamase enzymes that destroy the β-lactam ring (Fig. 21-3).
3 What is the antibacterial spectrum of the various subclasses of penicillins and cephalosporins (Table 21-10)?
| Drug Class | Examples | Coverage |
|---|---|---|
| Natural penicillins | Penicillin V (oral) Penicillin G (intravenous) Benzathine penicillin | Mostly gram-positive |
| Extended-spectrum penicillins | Ampicillin Amoxicillin (oral) | Gram-positive and increased gram-negative |
| Antistaphylococcal penicillins | Dicloxacillin Cloxacillin | Staphylococcus aureus |
| Antipseudomonal penicillins | Ticaracillin Piperacillin | Increasing gram-negative coverage, including Pseudomonas |
| Penicillin plus beta-lactamase inhibitor | Ampicillin-sulbactam (Unasyn) Amoxicillin–clavulanic acid (Augmentin) Piperacillin-tazobactam (Zosyn) | β-Lactam–resistant bacteria |
| First-generation cephalosporins | Cephalexin Cefotetan Cefazolin | Mostly gram-positive |
| Second-generation cephalosporins | Cefuroxime Cefaclor Cefoxitin | Mostly gram-positive |
| Third-generation cephalosporins | Ceftazidime Ceftriaxone | Penetrates the blood-brain barrier Ceftazidime covers Pseudomonas |
| Aztreonam | Aztreonam | Gram-negative rods |
10 Cover the two columns on the right of Table 21-11 and describe the mechanism of action and mechanism of bacterial resistance for the antimicrobial agents listed in the left column
Table 21-11 Mechanisms of Drug Action/Resistance
| Drug Class | Mechanism of Action | Mechanism of Resistance |
|---|---|---|
| Penicillin, cephalosporin, aztreonam | Inhibit transpeptidase and stimulation of autolysins | Formation of β-lactamases that break the β-lactam ring |
| Vancomycin | Inhibits cell wall synthesis by binding D-alanine | D-Alanine replaced with D-lactate |
| Tetracyclines | Bind to the 30S subunit of the bacterial ribosome, inhibiting protein synthesis | Decreased transport into the cell and increased transport out of the cell |
| Aminoglycosides | Impairs proper assembly of the ribosome, causing the 30S subunit to misread the genetic code | Acetylation, adenylation, or phosphorylation |
| Clindamycin | Binds 50S subunit to prevent peptide bond formation | |
| Chloramphenicol | Reversibly inhibits protein synthesis by binding to the 50S subunit | Acetylation |
| Linezolid | Binds to 50S subunit to prevent protein synthesis | |
| Macrolides | Bind to 50S subunit of ribosome, inhibiting translocation | Methylation |
| Fluoroquinolones | Inhibit DNA gyrase, preventing DNA replication | |
| Trimethoprim | Inhibits folic acid synthesis by inhibiting dihydrofolate reductase | |
| Sulfonamides | Inhibit folic acid synthesis by being a structural analog (competitive inhibitor) of PABA, a precursor of folic acid in bacteria | Modifications of PABA enzyme and increased synthesis of PABA |
| Metronidazole | Converts to a toxic metabolite that prevents cell wall synthesis | |
| Polymyxins | Interact with phospholipids to disrupt the bacterial cell wall |
PABA, para-aminobenzoic acid.
11 Cover the right column in Table 21-12 and describe the adverse effects for each of the antimicrobial agents listed in the left column
Table 21-12 Adverse Drug Effects
| Drug | Adverse Effects |
|---|---|
| β-Lactams | Hypersensitivity Diarrhea Cephalosporins have 10-20% cross-reactivity in penicillin-allergic patients |
| Tetracyclines | Gastrointestinal upset Discolors teeth in children Toxicity in patients with renal impairment Photosensitivity Affects bone growth in children |
| Aminoglycosides | Nephrotoxicity and ototoxicity |
| Macrolides | Gastrointestinal distress Acute cholestatic hepatitis Prolonged QT interval |
| Fluoroquinolones | Damages cartilage in young children Tendon rupture in adults |
| Chloramphenicol | Aplastic anemia Gray baby syndrome |
| Trimethoprim | Mimics folic acid deficiency (megaloblastic anemia, leukopenia, granulocytopenia) |
| Sulfonamides | Allergic reactions Hemolysis in glucose 6-phosphate deficiency Photosensitivity |
| Vancomycin | Nephrotoxicity and ototoxicity Thrombophlebitis Red man syndrome (prevented by antihistamines) |
| Metronidazole | Disulfiram-like reaction with concurrent alcohol intake Metallic taste |
 Mechanism of action and mode of resistance
Mechanism of action and mode of resistance
 Unique side effects and toxicity symptoms: Note that we said you should learn the unique side effects of each drug. Boards will not test you on the fact that certain antibiotics can cause occasional gastrointestinal (GI) upset or headache. These symptoms are characteristic of too many drugs to make for good test questions. Focus on the toxicities listed in Table 21-12.
Unique side effects and toxicity symptoms: Note that we said you should learn the unique side effects of each drug. Boards will not test you on the fact that certain antibiotics can cause occasional gastrointestinal (GI) upset or headache. These symptoms are characteristic of too many drugs to make for good test questions. Focus on the toxicities listed in Table 21-12.
 Clinical uses: Note that you should know the general uses for each drug (e.g., vancomycin is used for gram-positive organisms only, aminoglycosides for serious gram-negative infections, aztreonam for gram-negative rods, metronidazole and clindamycin for anaerobes) but you do not necessarily need to learn the individual organisms affected by every antibiotic. We do not mean to imply that this material is not important for your clinical years or fair game for boards, but it is less likely to be tested than the previous two points. However, you should be sure to know which drugs can be used for select bacterial species—namely, Pseudomonas, methicillin-resistant Staphylococcus aureus (MRSA), and Enterococcus.
Clinical uses: Note that you should know the general uses for each drug (e.g., vancomycin is used for gram-positive organisms only, aminoglycosides for serious gram-negative infections, aztreonam for gram-negative rods, metronidazole and clindamycin for anaerobes) but you do not necessarily need to learn the individual organisms affected by every antibiotic. We do not mean to imply that this material is not important for your clinical years or fair game for boards, but it is less likely to be tested than the previous two points. However, you should be sure to know which drugs can be used for select bacterial species—namely, Pseudomonas, methicillin-resistant Staphylococcus aureus (MRSA), and Enterococcus.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree