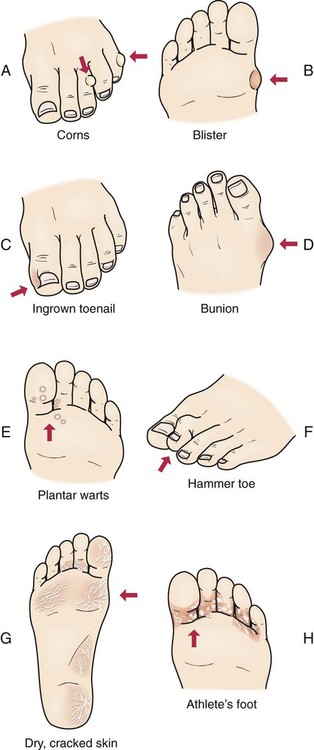
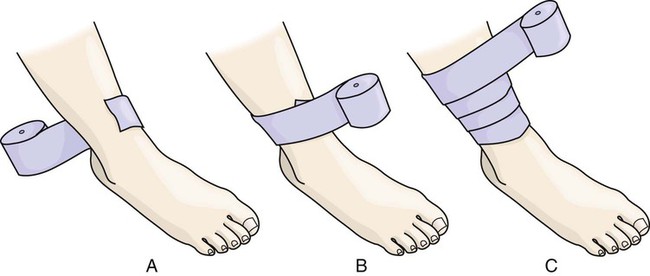
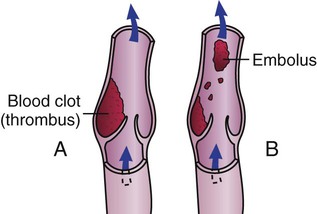
• Define the key terms and key abbreviations listed in this chapter. • Describe skin tears, circulatory ulcers, and diabetic foot ulcers. • Explain how to assist in preventing skin tears, circulatory ulcers, and diabetic foot ulcers. • Describe what to observe about wounds. • Explain how to secure dressings. • Explain the rules for applying dressings. • Explain the purpose, effects, and complications of heat and cold applications. • Describe the rules for applying heat and cold. • Perform the procedures described in this chapter. • Explain how to promote PRIDE in the person, the family, and yourself. A wound is a break in the skin or mucous membrane. Common causes are: • Trauma—an accident or violent act that injures the skin, mucous membranes, bones, and organs • Unrelieved pressure or friction (Chapter 25) • Decreased blood flow through arteries or veins See Delegation Guidelines: Assisting With Wound Care. A skin tear is a break or rip in the outer layers of the skin (Fig. 24-1). The epidermis (top skin layer) separates from the underlying tissues. The hands, arms, and lower legs are common sites for skin tears. Causes include: • Friction, shearing (Chapter 13), pulling, or pressure on the skin. • Falls or bumping a hard surface. Beds, bed rails, chairs, wheelchair footplates, and tables are dangers. • Holding an arm or leg too tight. • Bathing, dressing, and other tasks. • Pulling buttons and zippers across fragile skin. • Jewelry—yours or the person’s. Rings, watches, and bracelets are examples. • Long or jagged fingernails (yours or the person’s) and long or jagged toenails. Skin tears are painful. They are portals of entry for microbes. Infection is a risk. Tell the nurse at once if you cause or find a skin tear. To prevent skin tears, follow the care plan and the measures in Box 24-1. See Focus on Older Persons: Skin Tears. • Venous ulcers (stasis ulcers) are open sores on the lower legs or feet caused by poor venous blood flow (Fig. 24-2). Stasis means stopped or slowed fluid flow. The heels and inner part of the ankles are common sites. They can occur from skin injury. Scratching and trauma are examples. Venous ulcers are painful. Infection is a risk. Healing is slow. • Arterial ulcers are open wounds on the lower legs or feet caused by poor arterial blood flow. They are found between the toes, on top of the toes, and on the outer side of the ankle (Fig. 24-3). • Diabetic foot ulcers are open wounds on the foot caused by complications from diabetes. Diabetes (Chapter 28) can affect the nerves and blood vessels. When nerves are affected, the person can lose complete or partial sensation in a foot or leg. The person may not feel pain, heat, or cold. When blood vessels are affected, blood flow decreases. Tissues and cells do not get needed oxygen and nutrients. Sores heal poorly. Common foot problems (Fig. 24-4) can cause infection and tissue death (gangrene). Sometimes the affected part must be amputated. Check the person’s feet and legs every day. Report any sign of a foot problem at once. You must help prevent skin breakdown on the legs and feet. Follow the care plan to prevent and treat circulatory ulcers (Box 24-2). The doctor orders drugs and treatments as needed. If blood flow is sluggish, blood clots (thrombi) may form in the deep veins in the lower leg or thigh (Fig. 24-5, A). A blood clot (thrombus) can break loose and travel through the bloodstream. It then becomes an embolus—a blood clot that travels through the vascular system until it lodges in a blood vessel (Fig. 24-5, B). An embolus from a vein lodges in the lungs (pulmonary embolism). A pulmonary embolism can cause severe respiratory problems and death. Report chest pain or shortness of breath at once. Persons at risk for thrombi include those who: See Delegation Guidelines: Elastic Stockings. See Promoting Safety and Comfort: Elastic Stockings. See procedure: Applying Elastic Stockings. • Use the correct size—length and width. • Position the person in good alignment. • Face the person during the procedure. • Start at the lower (distal) part of the extremity. Work upward to the top (proximal) part. • Expose the fingers or toes if possible. This allows circulation checks. • Apply the bandage with firm, even pressure. • Check the color and temperature of the extremity every hour. • Re-apply a loose or wrinkled bandage. See Focus on Communication: Elastic Bandages. See Delegation Guidelines: Elastic Bandages. See Promoting Safety and Comfort: Elastic Bandages. See procedure: Applying an Elastic Bandage.
Assisting With Wound Care
Skin Tears
Circulatory Ulcers
Prevention and Treatment
![]() Elastic Stockings.
Elastic Stockings.
![]() Elastic Bandages.
Elastic Bandages.

Assisting With Wound Care
Get Clinical Tree app for offline access