1. Define, spell, and pronounce the terms listed in the vocabulary. 2. Apply critical thinking skills in performing the patient assessment and patient care. 3. Describe the structural development of the human body. 5. Outline the medical assistant’s role in preparing for the physical examination. 6. Summarize the instruments and equipment the physician typically uses during a physical examination. 7. Describe the six methods of examination and give an example of each. 8. Outline the basic principles of properly gowning and draping a patient for examination. 9. Name the various positions that may be used during an examination and identify the purpose of each. 12. Outline the sequence of a routine physical examination. 14. Summarize the role of the medical assistant in the physical examination process. 15. Determine the role of patient education during the physical examination. 16. Discuss the legal and ethical implications of the physical examination. auscultation The act of listening to body sounds, typically with a stethoscope, to assess various organs throughout the body. bruit (broo′-it) An abnormal sound or murmur heard on auscultation of an organ, vessel (such as a carotid artery), or gland. colonoscopy Procedure in which a fiberoptic scope is used to examine the large intestine. electrocardiogram (i-lek-tro-kar′-de-uh-gram) A graphic record of electrical conduction through the heart. emphysema (em-fuh-ze′-muh) Pathologic accumulation of air in the alveoli, which results in alveolar destruction and overall oxygen deprivation; in the lungs, the bronchioles become plugged with mucus and lose elasticity. gait Manner or style of walking. hematopoiesis (hi-ma-tuh-poi-e′-suhs) The formation and development of blood cells in the red bone marrow. intercellular Term referring to the area between cells. intracellular Term referring to the area within the cell membrane. manipulation Movement or exercising of a body part by means of an externally applied force. mastication (mas-tuh-ka′-shun) Chewing. nodules (nah′-juhls) Small lumps, lesions, or swellings that are felt when the skin is palpated. peristalsis (per-uh-stahl′-suhs) Rhythmic contraction of involuntary muscles lining the gastrointestinal tract. sclera The white part of the eye that forms the orbit. transillumination Inspection of a cavity or organ by passing light through its walls. trauma Physical injury or a wound caused by an external force or violence. vasoconstriction (va-zo-kuhn-strik′-shun) Contraction of the muscles lining blood vessels, which narrows the lumen. Felicia Grand, a newly hired certified medical assistant (CMA, AAMA), works for Dr. Anna Kosto, who is a member of a busy multiphysician primary care practice. One of Felicia’s chief responsibilities is to assist Dr. Kosto with physical examinations. Her duties include preparing and maintaining the examination room and equipment; getting the patient ready for specific physical examinations; and gowning, draping, and positioning the patient as needed. Because Felicia will be assisting with examinations, she must become familiar with the physical examination procedure and the order in which the physician needs various pieces of medical equipment. It also is important that Felicia protect herself from possible injury by using appropriate body mechanics throughout her day in the office. While studying this chapter, think about the following questions: To promote health maintenance, healthcare professionals must understand the anatomy and physiology of the body, the role each part plays, how each component functions, and what happens to the body when disease occurs in body systems. Anatomy is the study of how the body is shaped and structured. It encompasses a wide range of subjects, including structural development, levels of organization, relationships among microscopic parts, and the interrelationship of structure and function. Physiology is the study of body functions. This field is subdivided into areas of study; some physiologists spend their entire lives studying only one function, such as how cells work or how a single organ, such as the small intestine, is interrelated in function with the stomach and the large intestine. Separating these two sciences is almost impossible, because one continuously influences the other. Function affects structure, and structure affects function; for example, an infant can suck effortlessly because of the lack of teeth in the mouth. Once teeth appear, sucking becomes more tiresome, and the child begins to chew and bite. Phenomena in structure and function affect the interrelationships of all body systems. The basic unit of life is the cell. Cells determine the functional and structural characteristics of the entire body. Cells are microscopic in size, have a variety of shapes, and perform a vast array of functions. It is estimated that the human body is composed of approximately 100 trillion living, functioning cells. A cell is made up of three primary parts: the plasma membrane that surrounds the cell, creating an outer covering; the intracellular environment, which includes the cytoplasm that contains the living material that carries on the cell’s function; and the nucleus of the cell, which contains the genetic code of the cell that determines the cell’s function. When cells with similar structure and function are placed together, they form tissues. The study of tissues is known as histology. All of the body tissues are grouped into four types. The types of tissues distributed throughout the body and where they are located are as follows: An organ is composed of two or more types of tissue bound together to form a more complex structure for a common purpose or function. An organ may have one or many functions; for example, the pancreas has an endocrine function because it produces the hormone insulin, and a digestive function because it produces digestive enzymes. Organs also may be part of one or several systems. For example, in the male system, the urethra is part of both the urinary and the reproductive system. A body system is composed of several organs and their associated structures. These structures work together to perform a specific function in the body. Each system has specific units in it, and each performs specific functions. Table 32-1 summarizes the body systems; their primary cells, organs, and structures; and the major functions of each. TABLE 32-1 Primary care physicians (PCPs) treat patients of all ages for a broad range of diseases and complaints. A PCP is qualified to provide continuing healthcare for the entire family, from birth to old age. Most health insurance programs have converted to the primary care referral system. This means that most patients are required to have a PCP as the gatekeeper in personal healthcare. Therefore, the PCP must be contacted first, before the patient can be referred to specialty physicians for care. The PCP evaluates the patient’s total healthcare needs, provides personal medical care within one or more fields of medicine, and refers the patient to a specialist when an advanced or serious condition warrants additional expertise. The medical assistant’s clinical responsibilities in a primary care office include assisting with patients who may have problems in any of the body systems and with procedures in all age groups. With such a diversified scope of practice, the physician and medical assistant must work as a team to use their time efficiently and still provide quality, patient-centered healthcare. The purpose of a physical examination is to determine the patient’s overall state of well-being. All major organs and body systems are checked during a physical examination. As the physician examines the entire body, he or she interprets the findings, and by the time the examination has been completed, the physician has formed an initial diagnosis of the patient’s condition. Often laboratory and other diagnostic tests are ordered to supplement the physician’s initial diagnosis. The results of these tests are used to refine the patient’s diagnosis, to help the physician plan or revise treatment for the patient, to evaluate and maintain current drug therapy, and/or to determine the patient’s progress. Assessment of the patient begins with the first contact in the office. Before the examination, the medical assistant has the opportunity to make sure that the patient feels comfortable during the examination process and that all the necessary medical information has been obtained. As part of patient preparation, the medical assistant should verify the patient’s insurance information and document current medications and allergies. The medical assistant’s duties include preparing and maintaining the examination room and equipment, preparing the patient, and assisting the physician during the physical examination. The medical assistant is responsible for making sure the examination room is ready for any procedure that might be performed during the physical examination. The area should be as comfortable as possible for the patient and free of any potential dangers (Procedure 32-1). The examination room is prepared as follows: • The examination room should contain all materials required for observing Standard Precautions, including disposable gloves, a sink with an antibacterial hand-washing agent, paper towels, biohazard waste containers, sharps containers, and impervious gowns and face guards. Sharps containers are replaced when they are two-thirds full, as indicated by Standard Precautions (see Chapter 27). Getting the patient ready for the examination includes taking care of paperwork before the patient enters the examination room and performing related clinical skills. • Measure and record the patient’s height, weight, body mass index (BMI), and vital signs. • Assist the patient into and out of various examination positions as needed. • Document patient data in the medical record, completing all forms required. • Help the patient with dressing as needed after the examination. The medical assistant should be prepared to help the physician complete the physical examination as comprehensively and efficiently as possible. You have already prepared the room, so all equipment and supplies are available and in good working order; you also have prepared the patient by gathering the needed information and measuring and recording vital signs. During the examination, the physician may expect the medical assistant to do the following: • Hand him or her instruments and equipment as requested and provide supplies as needed. • Position and drape the patient during different phases of the examination. The instruments typically used during the physical examination are shown in Figure 32-1. They enable the physician to see, feel, inspect, and listen to parts of the body. All equipment must be in good working order, properly disinfected, and readily available for the physician’s use during the examination. The instruments most frequently used for a physical examination are described in the following paragraphs. Physical examinations typically are performed from the head to the feet; the instruments are listed in the order in which the physician typically would request them. An ophthalmoscope is used to inspect the inner structures of the eye. It consists of a stainless-steel handle containing batteries and an attached head, which has a light, magnifying lenses, and an opening through which the eye is viewed. Examination rooms usually are equipped with wall-mounted electrical units for the ophthalmoscope and otoscope, a dispenser for disposable speculums, and a wall-mounted sphygmomanometer. A tongue depressor is a flat, wooden blade used to hold down the tongue when the throat is examined. An otoscope is used to examine the external auditory canal and tympanic membrane. It has a stainless-steel handle containing batteries or is part of a wall-mounted electrical unit. The head of the otoscope has a light that is focused through a magnifying lens and should be covered with a disposable ear speculum. The light also may be used to illuminate the nasal passages and throat. A nasal speculum is a stainless-steel instrument used to inspect the lining of the nose, nasal membranes, and internal septum (Figure 32-2). When the handles of the nasal speculum are squeezed, the tips spread apart to dilate the nostrils, allowing the physician to visualize the internal aspects. An otoscope with a special attachment may also be used for nasal visualization. Tuning forks are aluminum fork-shaped instruments that consist of a handle and two prongs (Figure 32-3, A). The prongs produce a humming sound when the physician strikes them against his or her hand. Tuning forks are available in different sizes, and each size produces a different pitch level. A tuning fork is used to check the patient’s auditory acuity (Figure 32-3, B) and to test bone vibration (Figure 32-3, C). This aluminum instrument consists of a handle and two prongs that produce a humming sound when the physician strikes the prongs against his or her hand. A tape measure is a flexible ribbon ruler that is usually printed in inches and feet on one side and in centimeters and meters on the opposite side. Measurements may be used to assess length and head circumference in infants, wound size, and so on. A stethoscope is a listening device used when certain areas of the body are auscultated, particularly the heart and lungs. This instrument is available in many shapes and sizes. All have two earpieces that are connected to flexible rubber or vinyl tubing (Figure 32-4). At the distal end of the tubing is a diaphragm or bell (many have both), which, when placed securely on the patient’s skin, enables the physician to hear internal body sounds. A reflex hammer is sometimes called a percussion hammer. This stainless-steel instrument has a hard rubber head that is used to strike the tendons of the knee and elbow to test the neurologic reflexes. Disposable examination gloves protect the healthcare worker and the patient from microorganisms. According to Standard Precautions, gloves must be worn whenever the potential exists for contact with any body fluid, broken skin or wounds, or contaminated items. Gauze squares, cotton balls, cotton-tipped applicators, specimen containers, hemoccult packets, Pap smear supplies for female patients, lubricating jelly for vaginal and rectal examinations, and laboratory request forms should be easily accessible during the examination. Examinations are performed as both a routine confirmation of the absence of illness and a means of diagnosing disease. Healthcare providers use six methods to examine the human body. All six are part of a complete physical examination. During inspection, the examiner uses observation to detect significant physical features or objective data. This method of examination ranges from focusing on the patient’s general appearance (general state of health, including posture, mannerisms, and grooming) to more detailed observations, including body contour, gait, symmetry, visible injuries and deformities, tremors, rashes, and color changes. In palpation, the examiner uses the sense of touch (Figure 32-5, A). A part of the body is felt with the hand to determine its condition or the condition of an underlying organ. Palpation may involve touching the skin or performing a firmer exploration of the abdomen for underlying masses. This technique involves a wide range of perceptions, including temperature, vibration, consistency, form, size, rigidity, elasticity, moisture, texture, position, and contour. Palpation is performed with one hand, both hands (bimanual), one finger (digital), the fingertips, or the palmar aspect of the hand. A pelvic examination is done bimanually, whereas an anal examination is performed digitally. Do not confuse palpation with palpitation, which is a throbbing pulsation felt in the chest. Percussion involves tapping or striking the body, usually with the fingers or a small hammer, to elicit sounds or vibratory sensations. Percussion aids determination of the position, size, and density of an underlying organ or cavity. The effect of percussion is both heard and felt by the examiner; it is helpful in determining the amount of air or solid matter in an underlying organ or cavity. The two basic methods of percussion are direct percussion and indirect percussion. Direct (immediate) percussion is performed by striking the body with a finger. With indirect (mediate) percussion, which is used more frequently, the physician places his or her hand on the area and then strikes the placed hand with a finger of the other hand (Figure 32-5, B). Both a sound and a sense of vibration are evident. The examiner quantifies the sound in terms of pitch, quality, duration, and resonance. For auscultation, the physician uses a stethoscope to listen to sounds arising from the body (not the sound produced by the physician, as in percussion, but sounds that originate within the patient’s body). Auscultation is a difficult method of examination, because the physician must distinguish between a normal sound and an abnormal sound (Figure 32-5, C). It is particularly useful for evaluating sounds originating in the lungs, heart, and abdomen, such as a murmur, a bruit, and bowel sounds. Mensuration is the process of measuring. Measurements that are recorded include the patient’s height and weight, the length and diameter of an extremity, the extent of flexion or extension of an extremity, the size of the uterus during pregnancy, the size and depth of a wound, and the pressure of a grip. Measurements are taken with a flexible tape measure, a circular wound measurement device (Figure 32-6), or a specialized piece of equipment (e.g., a goniometer, which is used to measure joint angles) and usually are recorded in centimeters.
Assisting with the Primary Physical Examination
Learning Objectives
Vocabulary
Scenario
Anatomy and Physiology
Structural Development
Cells
Tissues
Organs
Systems
BODY SYSTEM
CELLS, ORGANS, AND STRUCTURES
FUNCTIONS
Blood
Arteries, arterioles, veins, venules, white blood cells, red blood cells, platelets, plasma
Transports materials and collects wastes throughout the body; white blood cells fight infection; red blood cells carry oxygen; platelets help form clots; plasma carries dissolved nutrients and other materials
Cardiovascular
Heart, valves, arteries, arterioles, veins, venules
Circulatory system transports materials in the blood throughout the body; veins return deoxygenated blood to the heart, which pumps it into the lungs; oxygenated blood is pumped into the aorta and branching arteries to cells throughout the body
Endocrine
Pituitary, pineal gland, hypothalamus, thyroid, pancreas, adrenal cortex and medulla, parathyroid, thymus, ovaries, testes
Produces hormones that circulate in the blood to target tissue that stimulates a particular action
Integumentary
Skin, subcutaneous tissue, sweat and sebaceous glands, hair, nails, sense receptors
Protection, temperature regulation; senses organ activity
Gastrointestinal
Mouth, tongue, teeth, pharynx, esophagus, stomach, small intestine, large intestine, liver, gallbladder, pancreas, appendix
Mastication, swallowing, digestion, absorption of nutrients, excretion of waste materials
Lymphatic and immune
Lymph, lymph vessels, lymph nodes, thymus, tonsils, spleen, lymphocytes, antibodies
Maintains fluid balance; protects internal environment; defends against foreign cells and disease; provides immunity to some diseases
Musculoskeletal
Bones, joints, muscles, tendons, ligaments, cartilage
Movement, posture, heat production, support, protection, mineral storage, hematopoiesis
Nervous
Brain, spinal cord, neurons, neuroglial cells, peripheral nerves, autonomic nerves
Controls body structures to maintain homeostasis; higher-order thinking and reflex centers that control autonomic processes; carries sensory stimulus to the brain and motor impulses to the periphery
Reproductive
Female: Estrogen and progesterone, ovum, ovaries, fallopian tubes, uterus, vagina, vulva, mammary glands
Male: testosterone, sperm, epididymis, vas deferens, prostate gland, testes, scrotum, penis, urethra
Produces hormones; reproduction
Respiratory
Nose, sinuses, pharynx, larynx, trachea, bronchi, lungs, bronchioles, alveoli
Responsible for inhalation of oxygen and exhalation of carbon dioxide externally and exchange of oxygen and carbon dioxide internally at the cellular level; acid-base regulation
Sensory
Eyes, ears, taste buds, olfactory receptors, sensory receptors
Helps sense changes in the external and internal environments through vision, hearing, balance, taste, and smell
Urinary
Nephron unit, bilateral kidneys, ureters, urinary bladder, urethra
Filters waste material from the blood; reabsorbs fluid and electrolytes as needed; excretes waste in the urine; maintains electrolyte, water, and acid-base balances; regulates blood pressure; activates red blood cells
Primary Care Physician
Physical Examination
Preparing for the Physical Examination
Role of the Medical Assistant in the Physical Examination
Room Preparation.
Patient Preparation.
Assisting the Physician.
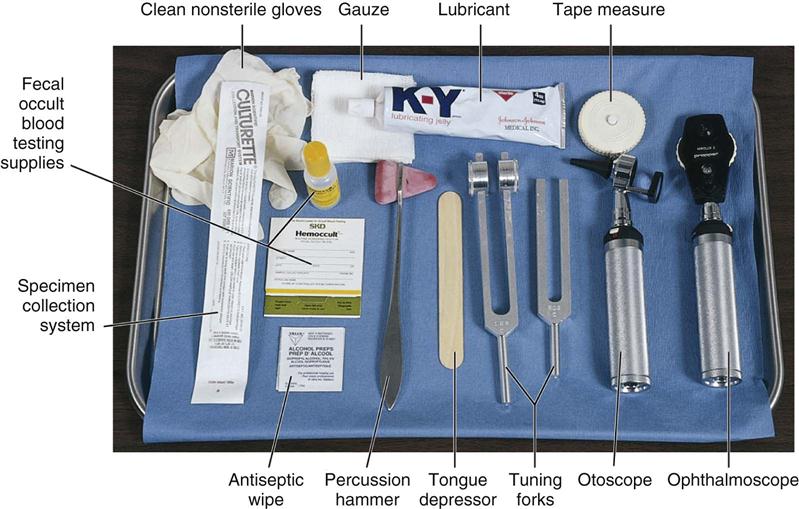
Supplies and Instruments Needed for the Physical Examination
Ophthalmoscope.
Tongue Depressor.
Otoscope.
Nasal Speculum.

Tuning Fork.
Tape Measure.
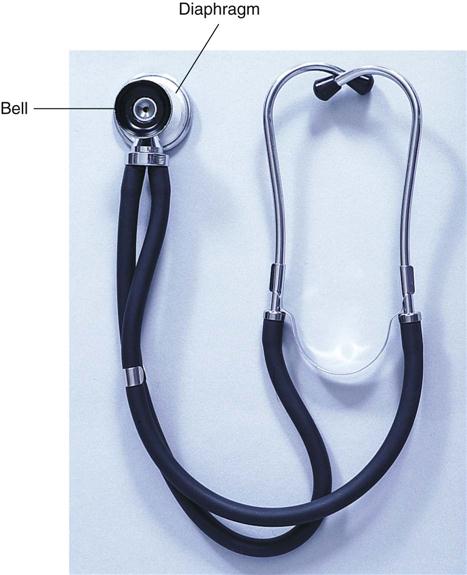
Stethoscope.
Reflex Hammer.
Gloves.
Additional Supplies.
Assisting With the Physical Examination
Methods of Examination
Inspection.
Palpation.
Percussion.
Auscultation.
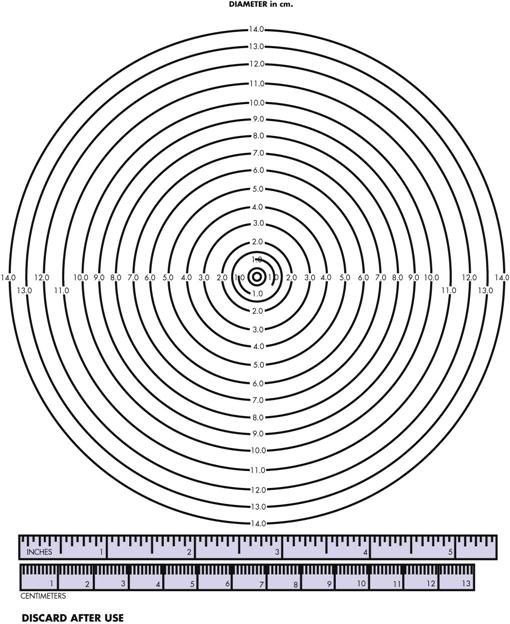
Mensuration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree