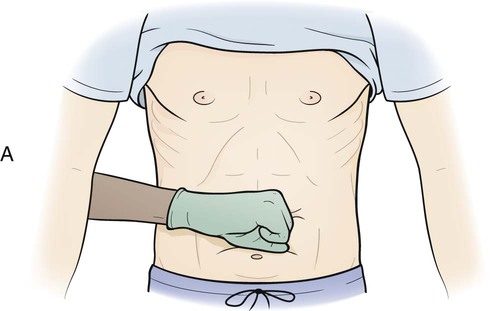
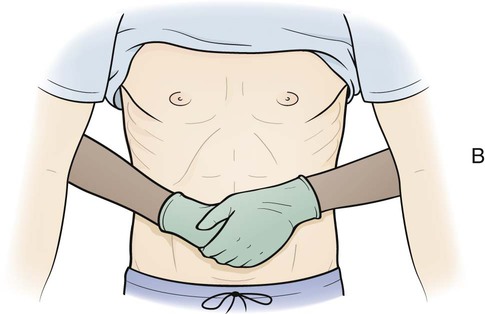
AED Automated external defibrillator CPR Cardiopulmonary resuscitation EMS Emergency Medical Services MSDS Material safety data sheet OSHA Occupational Safety and Health Administration PASS Pull the safety pin, aim low, squeeze the lever, sweep back and forth RACE Rescue, alarm, confine, extinguish • Define the key terms and key abbreviations listed in this chapter. • Describe accident risk factors. • Explain why you identify a person before giving care. • Explain how to correctly identify a person. • Describe the safety measures to prevent burns, poisoning, and suffocation. • Identify the signs and causes of choking. • Explain how to prevent equipment accidents. • Explain wheelchair and stretcher safety. • Explain how to handle hazardous substances. • Identify natural and human-made disasters. • Describe fire prevention measures and oxygen safety. • Explain what to do during a fire. • Explain how to protect yourself from workplace violence. • Describe your role in risk management. • Perform the procedures described in this chapter. • Explain how to promote PRIDE in the person, the family, and yourself. Safety is a basic need. Patients and residents are at great risk for accidents and falls. (See Chapter 10 for falls.) Some accidents and injuries cause death. See Promoting Safety and Comfort: Assisting With Safety, p. 98 See Focus on Surveys: Assisting With Safety, p. 98. • Age. Body changes occur with aging. Many older persons have decreased strength, move slowly, and are unsteady. Often balance is affected. Older persons also are less sensitive to heat and cold. They have poor vision, hearing problems, and a dulled sense of smell. Confusion, poor judgment, memory problems, and disorientation may occur (Chapter 30). Children are also at risk for injuries. • Awareness of surroundings. Coma is a state of being unaware of one’s setting and being unable to react or respond to people, places, or things. The person relies on others for protection. Confused and disoriented persons may not understand what is happening to and around them. • Agitated and aggressive behaviors. Pain can cause these behaviors. So can confusion, decreased awareness of surroundings, and fear of what may happen. • Vision loss. Persons with poor vision may not see toys, rugs, equipment, furniture, and cords. Some cannot read labels on containers. Poisoning can result. • Hearing loss. Persons with hearing loss have problems hearing explanations and instructions. They may not hear warning signals or fire alarms. Some cannot hear approaching meal carts, drug carts, stretchers, or people in wheelchairs. They do not know to move to safety. • Impaired smell and touch. Illness and aging affect smell and touch. The person may not detect smoke or gas odors. Burns are a risk from impaired touch. The person has problems sensing heat and cold. Some people have a decreased sense of pain. They may be unaware of injury. • Impaired mobility. Some diseases and injuries affect mobility. A person may know there is danger but cannot move to safety. Some persons cannot walk or propel wheelchairs. Some persons are paralyzed. Paralysis means loss of muscle function, sensation, or both. • Drugs. Drug side effects may include loss of balance, drowsiness, and lack of coordination. Reduced awareness, confusion, and disorientation occur. See Focus on Older Persons: Accident Risk Factors (Age). The person may receive an identification (ID) bracelet when admitted to the agency (Fig. 9-1). The bracelet has the person’s name, room and bed number, birth date, age, doctor, and other identifying information. • Compare identifying information on the assignment sheet with that on the ID bracelet (Fig. 9-2). Carefully check the information. Some people have the same first and last names. For example, John Smith is a very common name. • Use at least 2 identifiers. An identifier cannot be the person’s room or bed number. Some agencies require that the person state and spell his or her name and give his or her birth date. Others require using the person’s ID number. Always follow agency policy. • Call the person by name when checking the ID bracelet. This is a courtesy given as you touch the person and before giving care. Just calling the person by name is not enough to identify him or her. Confused, disoriented, drowsy, hard-of-hearing, or distracted persons may answer to any name. See Focus on Communication: Identifying the Person. See Promoting Safety and Comfort: Identifying the Person. • Assist with eating and drinking as needed. Spilled hot food or fluids can cause burns. • Be careful when carrying hot food and fluids, especially when near patients or residents. • Keep hot food and fluids away from counter and table edges. • Do not pour hot liquids near a person. • Turn on cold water first, then hot water. Turn off hot water first, then cold water. • Measure bath or shower water temperature (Chapter 16). Check it before a person gets into the tub or shower. • Check for “hot spots” in bath water. Move your hand back and forth. • Do not let the person sleep with a heating pad or an electric blanket. • Follow safety guidelines when applying heat and cold (Chapter 24). • Provide safety measures for persons who smoke. • Make sure patients and residents cannot reach hazardous materials (p. 106). • Follow agency policy for storing personal care items. Shampoo, mouthwash, lotion, perfume, and deodorant are examples. These products are harmful when swallowed. • Keep harmful products in their original containers. • Leave the original label on harmful products. Suffocation is when breathing stops from the lack of oxygen. Death occurs if the person does not start breathing. Common causes include choking, drowning, inhaling gas or smoke, strangulation, and electrical shock (p. 105). Measures to prevent suffocation are listed in Box 9-1. Clear the airway if the person is choking. • Encourage the person to keep coughing to expel the object. • Do not interrupt the person’s efforts to clear the airway. If the person is breathing and coughing, abdominal thrusts are not needed. The conscious person clutches at the throat (Fig. 9-4). Clutching at the throat is often called the “universal sign of choking.” The conscious person is very frightened. If the obstruction is not removed, the person will die. Severe airway obstruction is an emergency. Abdominal thrusts are not used for very obese persons or pregnant women. Chest thrusts are used (Box 9-2 and Fig. 9-5). See Focus on Older Persons: Choking. See procedure: Relieving Choking—Adult or Child (Over 1 Year of Age).
Assisting With Safety
Key Abbreviations
Accident Risk Factors
Identifying the Person

Preventing Burns
Preventing Poisoning
Preventing Suffocation
Choking
![]() Relieving Choking.
Relieving Choking.

Assisting With Safety
Get Clinical Tree app for offline access