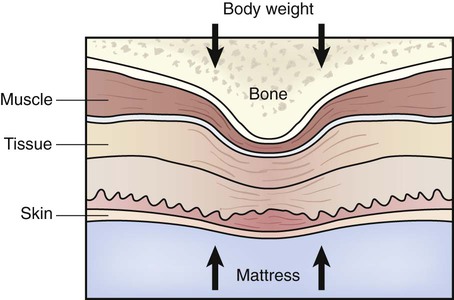
• Define the key terms and key abbreviation listed in this chapter. • Describe the causes and risk factors for pressure ulcers. • Identify the persons at risk for pressure ulcers. • Describe the stages of pressure ulcers. • Identify the sites for pressure ulcers. • Explain how to prevent pressure ulcers. • Identify the complications from pressure ulcers. • Explain how to promote PRIDE in the person, the family, and yourself. Before defining pressure ulcer, you need to understand these terms. • Bony prominence—an area where the bone sticks out or projects from the flat surface of the body. The back of the hand, shoulder blades, elbows, hips, spine, sacrum, knees, ankles, heels, and toes are bony prominences (Fig. 25-1, p. 400). These areas also are called pressure points. • Shear—when layers of the skin rub against each other. Or shear is when the skin remains in place and underlying tissues move and stretch and tear underlying capillaries and blood vessels. Tissue damage occurs. See Chapter 14. • Friction—the rubbing of 1 surface against another. The skin is dragged across a surface. Friction is always present with shearing. The National Pressure Ulcer Advisory Panel (NPUAP) defines pressure ulcer as a localized injury to the skin and/or underlying tissue, usually over a bony prominence (Fig. 25-2, p. 401). It is the result of pressure or pressure in combination with shear. Decubitus ulcer, bed sore, and pressure sore are other terms for pressure ulcer. Unrelieved pressure squeezes tiny blood vessels. For example, pressure occurs when the skin over a bony area is squeezed between hard surfaces (Fig. 25-3). The bone is 1 hard surface. The other is usually the mattress or chair seat. Squeezing or pressure prevents blood flow to the skin and underlying tissues. Oxygen and nutrients cannot get to the cells. Skin and tissues die. Persons at risk for pressure ulcers are those who: • Are bedfast (confined to bed) or chairfast (confined to a chair). • Need some or total help moving. • Are agitated or have involuntary muscle movements. • Have urinary or fecal incontinence. • Are exposed to moisture—urine, feces, wound drainage, sweat, or saliva. • Have poor nutrition or poor fluid balance. • Have lowered mental awareness. • Have problems sensing pain or pressure. • Have a healed pressure ulcer. • Take drugs that affect wound healing. • Refuse some care and treatment measures. • Have health problems such as kidney failure, thyroid disease, or diabetes. See Focus on Older Persons: Persons at Risk. In persons with light skin, a red area is the first sign of a pressure ulcer. In persons with dark skin, the skin may have no color change or appear red, blue, or purple. Color does not fade when pressure is applied. The area may feel warm or cool and soft or firm. The person may complain of pain, burning, tingling, or itching in the area. Some persons do not feel anything unusual. Box 25-1 describes pressure ulcer stages. The stages are shown in Figure 25-4. See Focus on Communication: Pressure Ulcer Stages. Pressure ulcers usually occur over bony prominences (pressure points). These areas bear the weight of the body in certain positions (see Fig. 25-1). Pressure from body weight can reduce the blood supply to the skin. According to the CMS, the sacrum is the most common site for a pressure ulcer. However, pressure ulcers on the heels often occur. The ears also are sites for pressure ulcers. This is from pressure on the ear from the mattress when in the side-lying position. Eyeglasses and oxygen tubing (Chapter 26) also can cause pressure on the ears. A urinary catheter can cause pressure and friction on the meatus. Tubes, casts, braces, and other devices can cause pressure on arms, hands, legs, and feet. A pressure ulcer can develop where medical equipment is attached to the skin.
Assisting With Pressure Ulcers
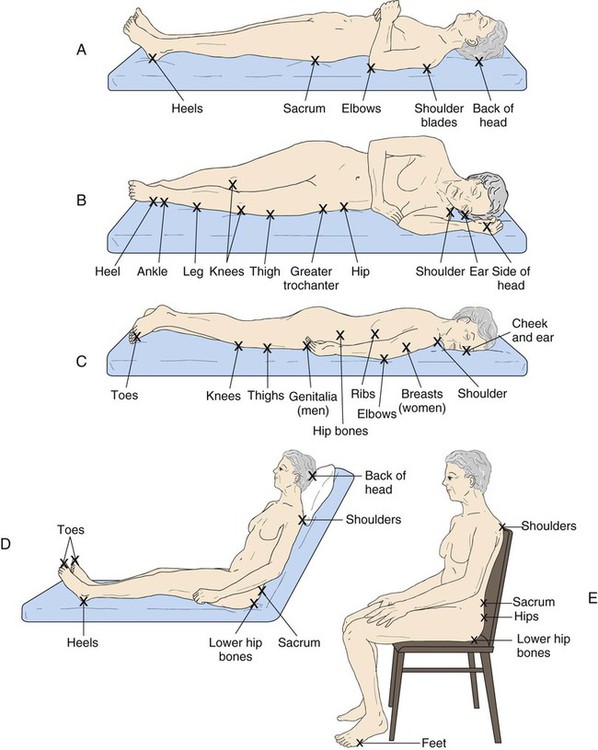
A, The supine position. B, The lateral position. C, The prone position. D, Fowler’s position. E, Sitting position.
Risk Factors
Persons at Risk
Pressure Ulcer Stages
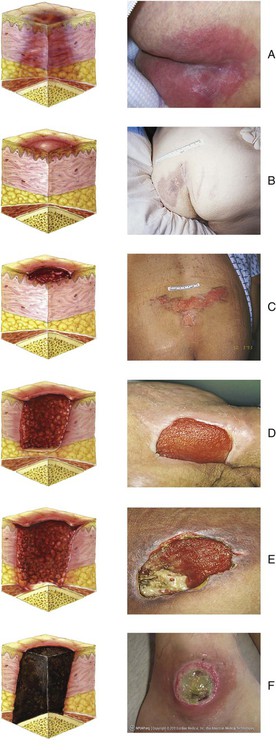
A, Suspected deep tissue injury. B, Stage 1. C, Stage 2. D, Stage 3. E, Stage 4. F, Unstageable.
Sites
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



