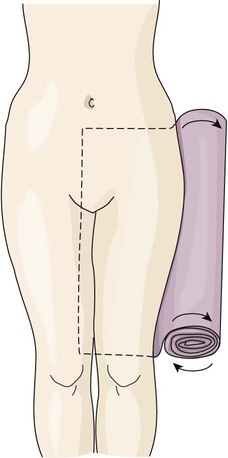
• Define the key terms and key abbreviations listed in this chapter. • Explain how to prevent the complications from bedrest. • Describe the devices used to support and maintain body alignment. • Describe range-of-motion exercises. • Perform the procedures described in this chapter. • Explain how to promote PRIDE in the person, the family, and yourself. See Focus on Older Persons: Assisting With Exercise and Activity. • Strict bedrest. Everything is done for the person. The person stays in bed for all activities of daily living (ADL). • Bedrest. The person can perform some ADL. Self-feeding, oral hygiene, bathing, shaving, and hair care are often allowed. • Bedrest with commode privileges. The commode is used for elimination. • Bedrest with bathroom privileges (bedrest with BRP). The bathroom is used for elimination. • A contracture is the lack of joint mobility caused by abnormal shortening of a muscle. The contracted muscle is fixed into position, is deformed, and cannot stretch (Fig. 23-1). Common sites are the fingers, wrists, elbows, toes, ankles, knees, and hips. They can also occur in the neck and spine. The site is deformed and stiff. • Atrophy is the decrease in size or the wasting away of tissue. Tissues shrink in size. Muscle atrophy is a decrease in size or a wasting away of muscle (Fig. 23-2). Good nursing care prevents complications from bedrest. Good alignment, range-of-motion exercises (p. 370), and frequent position changes are important measures. These are part of the care plan. See Focus on Communication: Complications From Bedrest. Body alignment and positioning were discussed in Chapter 13. Supportive devices are often used to support and maintain the person in a certain position. • Bed-boards—are placed under the mattress to prevent it from sagging (Fig. 23-3). • Foot-boards—prevent plantar flexion that can lead to footdrop. In plantar flexion, the foot (plantar) is bent (flexion). Footdrop is when the foot falls down at the ankle (permanent plantar flexion). The foot-board is placed so the soles of the feet are flush against it (Fig. 23-4). Foot-boards also keep top linens off the feet and toes. • Trochanter rolls—prevent the hips and legs from turning outward (external rotation) (Fig. 23-5). A bath blanket is folded to the desired length and rolled up. The loose end is placed under the person from the hip to the knee. Then the roll is tucked alongside the body. • Hip abduction wedges—keep the hips abducted (apart) (Fig. 23-6). The wedge is placed between the person’s legs. These are common after hip replacement surgery. • Hand rolls or hand grips—prevent contractures of the thumb, fingers, and wrist (Fig. 23-7, p. 370). Foam rubber sponges, rubber balls, and finger cushions (Fig. 23-8, p. 370) also are used. • Splints—keep the elbows, wrists, thumbs, fingers, ankles, and knees in normal position. They are usually secured in place with Velcro (Fig. 23-9, p. 370). • Bed cradles—keep the weight of top linens off the feet and toes (Fig. 23-10, p. 370). The weight of top linens can cause footdrop and pressure ulcers. The movement of a joint to the extent possible without causing pain is the range of motion (ROM) of the joint. Range-of-motion exercises involve moving the joints through their complete range of motion (Box 23-1). They are usually done at least 2 times a day. • Active ROM exercises—are done by the person. • Passive ROM exercises—you move the joints through their range of motion. • Active-assistive ROM exercises—the person does the exercises with some help. See Focus on Communication: Range-of-Motion Exercises. See Focus on Surveys: Range-of-Motion Exercises. See Delegation Guidelines: Range-of-Motion Exercises. See Promoting Safety and Comfort: Range-of-Motion Exercises. See procedure: Performing Range-of-Motion Exercises, p. 372.
Assisting With Exercise and Activity
Bedrest
Complications From Bedrest
Positioning
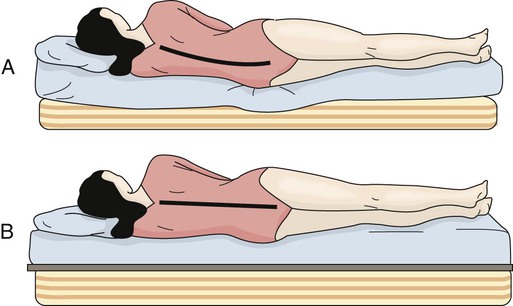
A, Mattress sagging without bed-boards. B, Bed-boards are under the mattress. No sagging occurs.
![]() Range-of-Motion Exercises
Range-of-Motion Exercises
Assisting With Exercise and Activity
Get Clinical Tree app for offline access