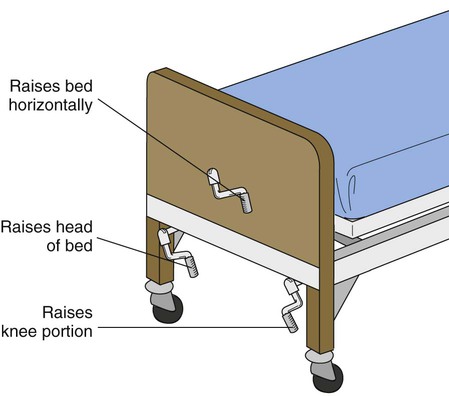
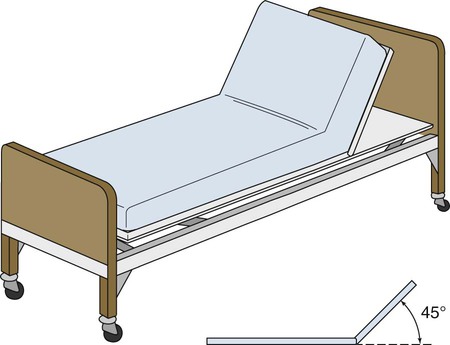
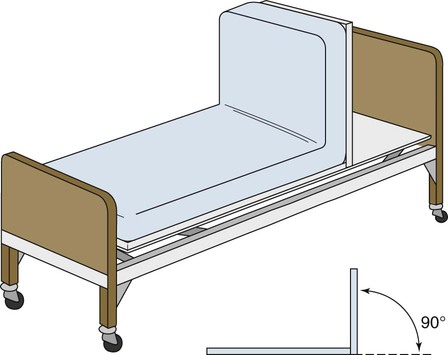
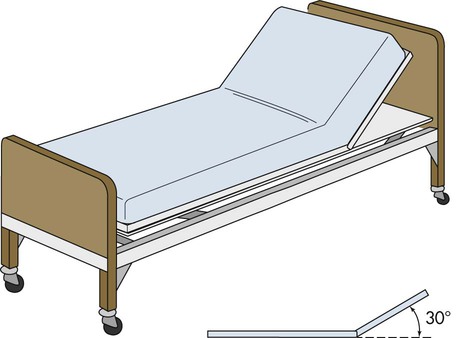
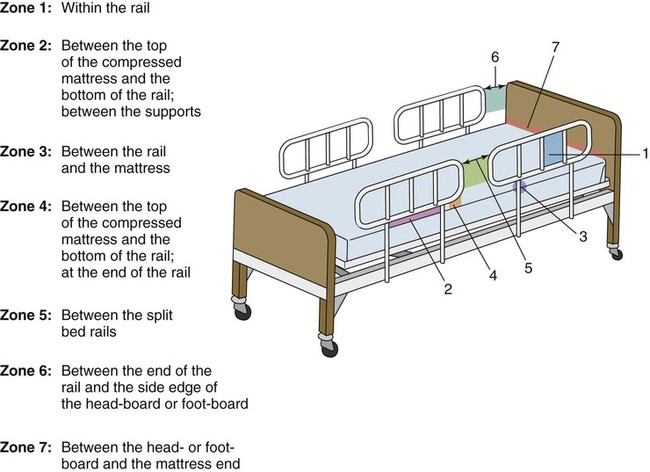
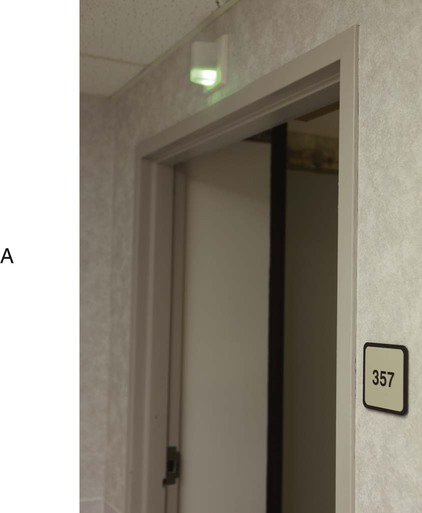
• Define the key terms and key abbreviations listed in this chapter. • Explain how to maintain the person’s unit. • Describe how to control temperature, odors, noise, and lighting for the person’s comfort. • Describe the basic bed positions. • Identify the 7 hospital bed system entrapment zones. • Identify the persons at risk for entrapment. • Explain how to use the furniture and equipment in the person’s unit. • Describe 4 ways to make beds. • Explain how to properly handle linens. • Explain how to assist the nurse with pain relief. • Explain the purposes of a back massage. • Explain how to assist the nurse with promoting sleep. • Perform the procedures described in this chapter. • Explain how to promote PRIDE in the person, the family, and yourself. The person’s unit is the personal space, furniture, and equipment provided for the person by the agency (Fig. 15-1). The person’s unit is designed to provide comfort, safety, and privacy. In nursing centers, resident units also are as personal and home-like as possible. Always treat the person’s unit with respect. You need to keep the person’s unit clean, neat, safe, and comfortable. See Box 15-1. See Focus on Communication: Comfort. • Empty, clean, and disinfect bedpans, urinals, commodes, and kidney basins promptly. • Make sure toilets are flushed. • Check incontinent persons often (Chapters 18 and 19). • Clean persons who are wet or soiled from urine, feces, vomitus, or wound drainage. • Change wet or soiled linens and clothing promptly. • Keep laundry containers closed. • Follow agency policy for wet or soiled linens and clothing. • Dispose of incontinence and ostomy products promptly (Chapters 18 and 19). • Provide good hygiene to prevent body and breath odors (Chapter 16). • Use room deodorizers as needed and allowed by agency policy. Sometimes odors remain after removing the cause. Do not use sprays around persons with breathing problems. Ask the nurse if you are unsure. According to the CMS, a “comfortable” sound level: Common health care sounds may disturb some persons. Such sounds include: • The clanging and clattering of equipment, dishes, and meal trays • Loud voices, TVs, radios, music players, ringing phones, and so on • Intercom systems and call lights • Equipment or wheels needing repair or oil See Focus on Communication: Noise. See Focus on Older Persons: Noise. Rooms are furnished and equipped to meet basic needs. The right to privacy is considered. Electric beds are common. Controls are on a side panel, bed rail, or the foot-board. Some controls are hand-held devices (Fig. 15-2). Patients and residents are taught to use the controls safely. They are warned not to raise the bed to the high position or to adjust the bed to harmful positions. They are told of any position limits or restrictions. Manual beds have cranks at the foot of the bed (Fig. 15-3). Pull the cranks up for use. Keep them down at all other times. Cranks in the “up” position are safety hazards. Anyone walking past may bump into them. See Promoting Safety and Comfort: The Bed. There are 6 basic bed positions. • Flat is the usual sleeping position. • Fowler’s position is a semi-sitting position. The head of the bed is raised between 45 and 60 degrees (Fig. 15-4). See Chapter 13. • High-Fowler’s position is a semi-sitting position. The head of the bed is raised 60 to 90 degrees (Fig. 15-5). • Semi-Fowler’s position means the head of the bed is raised 30 degrees (Fig. 15-6). Some agencies define semi-Fowler’s position as when the head of the bed is raised 30 degrees and the knee portion is raised 15 degrees. Know the definition used by your agency. • Trendelenburg’s position means the head of the bed is lowered and the foot of the bed is raised (Fig. 15-7). A doctor orders this position. Blocks are placed under the bed legs at the foot of the bed. Or the bed frame is tilted. • Reverse Trendelenburg’s position means the head of the bed is raised and the foot of the bed is lowered (Fig. 15-8). A doctor orders this position. Blocks are placed under the bed legs at the head of the bed. Or the bed frame is tilted. Hospital bed systems have 7 entrapment zones (Figs. 15-9 and 15-10, p. 204). Entrapment means that the person can get caught, trapped, or entangled in spaces created by the bed rails, the mattress, the bed frame, the head-board, or the foot-board. Head, neck, and chest entrapment can cause serious injuries and death. Arm and leg entrapment also can occur. Persons at greatest risk: The call system lets the person signal for help. The call light is at the end of a long cord (Fig. 15-12). It attaches to the bed or chair. (See p. 207 for call lights in bathrooms and shower and tub rooms.) Always keep the call light within the person’s reach—in the room, bathroom, and shower or tub room. To get help, the person presses a button at the end of the call light. The call light connects to a light above the room door. The call light also connects to a computer, light panel, or intercom system at the nurses’ station (Fig. 15-13, p. 206). These tell the staff that the person needs help. Some call lights are turned on by tapping with a hand or fist (Fig. 15-14). They are useful for persons with limited hand movement. See Focus on Communication: The Call System. See Promoting Safety and Comfort: The Call System. Beds are made every day. Clean, dry, and wrinkle-free linens: • Change linens when they are wet, soiled, or damp. • Straighten linens when loose or wrinkled and at bedtime. • Check for and remove food and crumbs after meals and snacks. • Check linens for dentures, eyeglasses, hearing aids, sharp objects, and other items. • Follow Standard Precautions and the Bloodborne Pathogen Standard. Contact with blood, body fluids, secretions, or excretions is likely. • A closed bed is not in use. Top linens are not folded back (Fig. 15-15). The bed is ready for a new patient or resident. In nursing centers, closed beds are made for residents who are up during the day. • An open bed is in use. Top linens are fan-folded back. A closed bed becomes an open bed by fan-folding back the top linens (Fig. 15-16). • An occupied bed is made with the person in it (Fig. 15-17). • A surgical bed is made to transfer a person from a stretcher to bed (Fig. 15-18). This includes an ambulance stretcher. Collect linens in the order you will use them. Doing so makes it easy to remember what you need. • Bottom sheet (flat or fitted) • Waterproof drawsheet or waterproof pad (if needed) • Cotton drawsheet (if needed) Use 1 arm to hold the linens. Use your other hand to pick them up. The first item is at the bottom of the stack. (The mattress pad is at the bottom. The bath blanket is on top.) To get the mattress pad on top, place your arm over the bath blanket. Then turn the stack over onto the arm on the bath blanket (Fig. 15-19). The arm that held the linens is now free. Place the clean linen on a clean surface. Remove dirty linen 1 piece at a time. Roll each piece away from you. The side that touched the person is inside the roll and away from you (Fig. 15-20). Discard each piece into a laundry bag.
Assisting With Comfort
The Person’s Unit
Comfort
Odors
Noise
Room Furniture and Equipment
The Bed
Bed Positions.
Bed Safety.


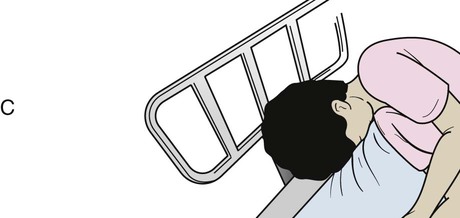




A, Zone 1: Within the bed rail. B, Zone 2: Between the top of the compressed mattress and the bottom of the bed rail and between the rail supports. C, Zone 3: Between the bed rail and the mattress. D, Zone 4: Between the top of the compressed mattress and the bottom of the bed rail and at the end of the bed rail. E, Zone 5: Between the split bed rails. F, Zone 6: Between the end of the bed rail and the side edge of the head-board or foot-board. G, Zone 7: Between the head-board or foot-board and the end of the mattress.
The Call System

Bedmaking
Types of Beds
Linens


A, The arm is placed over the top of the stack of linens. B, The stack of linens is turned onto the arm.
Assisting With Comfort
Get Clinical Tree app for offline access