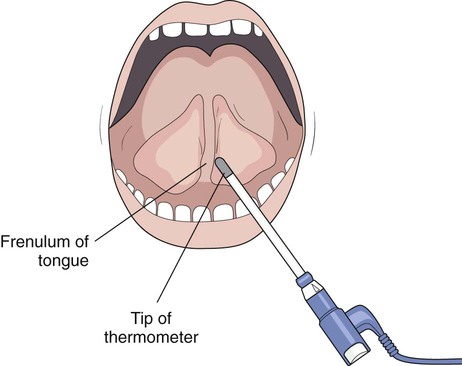
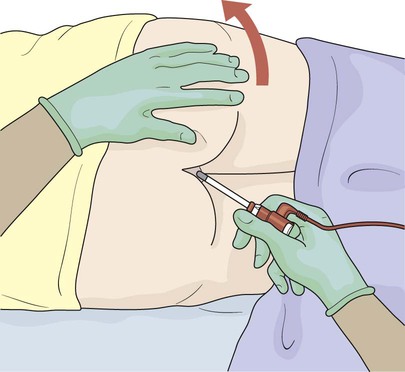
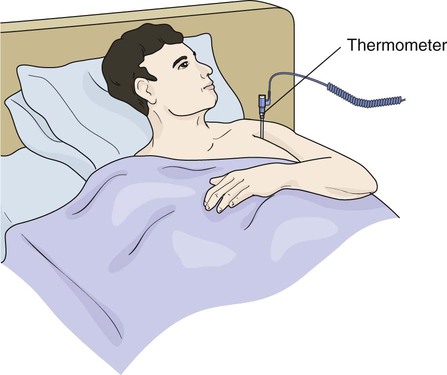
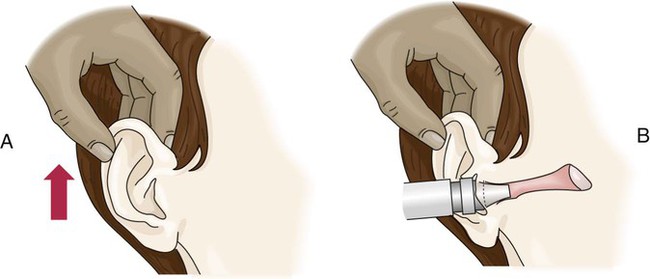
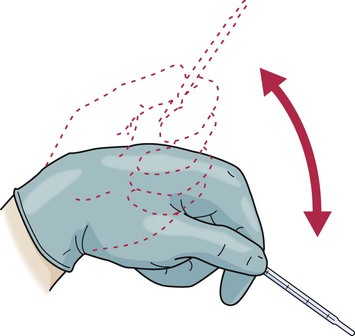
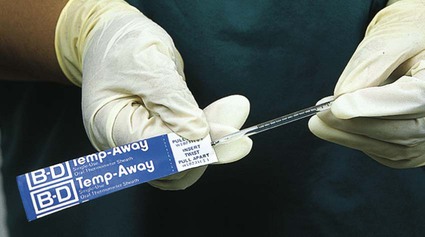
• Define the key terms and key abbreviations listed in this chapter. • Explain why vital signs are measured. • List the factors affecting vital signs. • Identify the normal ranges for each temperature site. • Explain when to use each temperature site. • Explain how to use thermometers. • Describe a normal pulse and normal respirations. • Describe the practices to follow when measuring blood pressure. • Describe the 4 types of pain. • Explain why pain is personal. • List the signs and symptoms of pain. • Identify the fluids counted as intake and the fluids counted as output. • Explain how to prepare the person for weight and height measurements. • Explain how you assist with assessment. • Perform the procedures described in this chapter. • Explain how to promote PRIDE in the person, the family, and yourself. Vital signs are often called TPR (temperature, pulse, and respirations) and BP (blood pressure). A person’s vital signs vary within certain limits. Box 21-1 lists the factors affecting vital signs. See Focus on Communication: Vital Signs. See Focus on Older Persons: Vital Signs. Body temperature is the amount of heat in the body. It is a balance between the amount of heat produced and the amount lost by the body. Heat is produced as cells use food for energy. It is lost through the skin, breathing, urine, and feces. Body temperature stays fairly stable. It is lower in the morning and higher in the afternoon and evening. See Box 21-1 for the factors affecting body temperature. Temperature sites are the mouth, rectum, axilla (underarm), tympanic membrane (ear), and temporal artery (forehead) (Box 21-2). Each site has a normal range (Table 21-1). Fever means an elevated body temperature. Always report temperatures that are above or below the normal range. TABLE 21-1 See Focus on Communication: Temperature Sites. See Focus on Older Persons: Temperature Sites. See Promoting Safety and Comfort: Temperature Sites. Follow the manufacturer’s instructions and agency procedures to use, clean, and store thermometers. • Electronic thermometers are battery operated. The temperature is shown on the front of the device. See “Electronic Thermometers.” • Standard electronic thermometer—measures body temperature at the oral, rectal, and axillary sites. See Figure 21-1, A. • Tympanic membrane thermometer—measures body temperature at the tympanic membrane in the ear (Fig. 21-1, B). • Temporal artery thermometer—measures body temperature at the temporal artery in the forehead (Fig. 21-1, C). • Digital thermometer—measures body temperature at the oral, rectal, and axillary sites. Depending on the type, the temperature is measured in 6 to 60 seconds. See Figure 21-1, D. • Glass thermometers have a hollow glass tube and a bulb tip (Fig. 21-1, E). The device is filled with a substance. When heated, the substance expands and rises in the tube. When cooled, the substance contracts and moves down the tube. See “Glass Thermometers” on p. 336. Electronic thermometers are commonly used. Probe covers or caps prevent the spread of infection. Electronic thermometers have batteries. Some are kept in chargers when not in use. • Standard electronic thermometers (see Fig. 21-1, A) measure temperature in a few seconds. They have oral (blue) and rectal (red) probes. The oral (blue) probe is used for axillary temperatures. • Tympanic membrane thermometers measure temperature in 1 to 3 seconds. They are comfortable and not invasive. There are fewer microbes in the ear than in the mouth or rectum. The risk of spreading infection is reduced. To use one, gently insert the covered probe into the ear (see Fig. 21-1, B). • Temporal artery thermometers measure body temperature in 3 to 4 seconds. Non-invasive, they measure the temperature of the blood in the temporal artery. It is the same temperature of the blood coming from the heart. To use one: 1. Use the side of the head that is exposed. Do not use the side covered by hair, a dressing, a hat, or other covering. Do not use the side that was on a pillow. 2. Place a disposable cap or cover on the thermometer. 3. Place the device in the center of the forehead. 5. Slide the device across the forehead and across the temporal artery (see Fig. 21-1, C). See Focus on Older Persons: Electronic Thermometers. See procedure: Taking a Temperature With an Electronic Thermometer, p. 334. Long- or slender-tip thermometers are used for oral and axillary temperatures. So are thermometers with stubby and pear-shaped tips. Rectal thermometers have stubby tips. See Figure 21-6. Glass thermometers are color-coded. Glass thermometers are re-usable. However, the following are problems. • They take a long time to register—3 to 10 minutes depending on the site. • They break easily. Broken rectal thermometers can injure the rectum and colon. • The person may bite down and break an oral thermometer. Cuts in the mouth are risks. If the thermometer contains mercury, swallowed mercury can cause mercury poisoning. See Box 21-3 for how to use and read glass thermometers. See Promoting Safety and Comfort: Glass Thermometers. See procedure: Taking a Temperature With a Glass Thermometer, p. 338.
Assisting With Assessment
Vital Signs
Body Temperature
Temperature Sites.
Site
Baseline
Normal Range
Oral
98.6°F (37.0°C)
97.6°F to 99.6°F
(36.5°C to 37.5°C)
Rectal
99.6°F (37.5°C)
98.6°F to 100.6°F
(37.0°C to 38.1°C)
Axillary
97.6°F (36.5°C)
96.6°F to 98.6°F
(35.9°C to 37.0°C)
Tympanic membrane
98.6°F (37.0°C)
98.6°F (37.0°C)
Temporal artery
99.6°F (37.5°C)
99.6°F (37.5°C)
Thermometers.



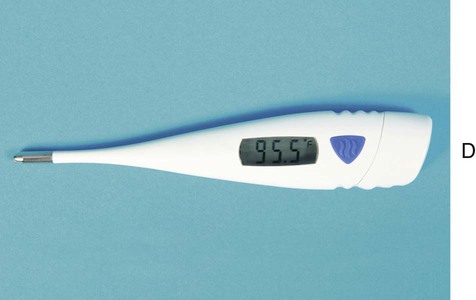
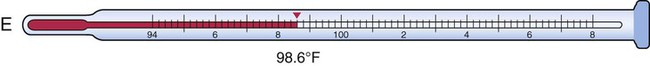
A, Standard electronic thermometer. B, Tympanic membrane thermometer. C, Temporal artery thermometer. D, Digital thermometer. E, Glass thermometer.
![]() Electronic Thermometers.
Electronic Thermometers.
![]() Glass Thermometers.
Glass Thermometers.
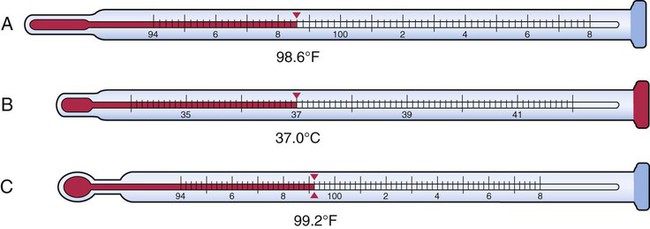
A, A Fahrenheit thermometer with a long or slender tip. The temperature measurement is 98.6°F. B, Centigrade thermometer with a stubby tip (rectal thermometer). The temperature measurement is 37.0°C. C, Fahrenheit thermometer with a pear-shaped tip. The temperature measurement is 99.2°F.

Assisting With Assessment
Get Clinical Tree app for offline access