Assisting in Pulmonary Medicine
Learning Objectives
1. Define, spell, and pronounce the terms listed in the vocabulary.
2. Apply critical thinking skills in performing the patient assessment and patient care.
3. Describe the organs of the respiratory system and their functions.
4. Explain the process of ventilation.
5. Implement correct respiratory system terminology when documenting in the medical record.
6. Describe the major diseases of the respiratory system.
7. Explain the diagnosis and treatment of tuberculosis.
8. Summarize the disorders associated with chronic obstructive pulmonary disease and their treatments.
9. Teach a patient how to use a peak flow meter.
10. Administer a nebulizer treatment.
11. Detail patient teaching for the use of a metered-dose inhaler.
12. Describe the cancers associated with the pulmonary system.
13. Summarize the medical assistant’s role in assisting with pulmonary procedures.
14. Distinguish among common diagnostic procedures for the respiratory system.
15. Perform a volume capacity spirometry test.
16. Correctly use a pulse oximeter.
17. Collect a sputum sample for culture.
18. Discuss legal and ethical issues associated with pulmonary medicine.
Vocabulary
bifurcates Divides from one into two branches.
bronchiectasis (brong′-ke-ek-tuh-sis) Dilation of the bronchi and bronchioles associated with secondary infection or ciliary dysfunction.
chronic bronchitis Recurrent inflammation of the membranes lining the bronchial tubes.
cilia (sil′-e-uh) Hairlike projections capable of movement; in the lungs, cilia waves move unwanted substances (e.g., mucus, dust, and pus) upward; cilia are destroyed by smoking.
hypercapnia (hi-per-kap′-ne-uh) Excess levels of carbon dioxide in the blood.
pulmonary consolidation In pneumonia, the process by which the lungs become solidified as they fill with exudates.
rhinorrhea (ri-no-re′-uh) The discharge of nasal drainage.
tubercle (too′-buhr-kuhl) A nodule produced by the tuberculosis bacillus.
tracheostomy (tra-ke-os′-tuh-me) A surgical opening made through the neck into the trachea to allow breathing.
virulent (vir′-u-lent) Exceedingly pathogenic, noxious, or deadly.
Scenario
Michael McGuire, CMA (AAMA), works for a primary care physician, Dr. John Samuelson, in the small town in which he grew up. Dr. Samuelson’s practice is open to all patients, but a large number of individuals with respiratory disease seek his help in managing their pulmonary problems. In the 6 months since he started with the practice, Michael has learned how to assist with pulmonary diagnostic tests and the special needs of patients with respiratory diseases. Michael has become familiar with the diagnosis and treatment of many common pulmonary problems and adept at accurately documenting respiratory system signs and symptoms. Many of Dr. Samuelson’s patients smoke cigarettes, and the main employers in the community are coal mining and construction companies, so many patients are at risk for smoking and occupation-related respiratory problems.
While studying this chapter, think about the following questions:
• What clinical skills are required in this specialty practice?
• What pulmonary complications are associated with smoking and occupational respiratory hazards?
• What diagnostic and treatment procedures typically are used in a pulmonary practice?
The respiratory system has two primary functions. The first is to exchange oxygen from the atmosphere for carbon dioxide waste. The two types of respiration are external respiration, which brings oxygen into the lungs, where carbon dioxide exchange occurs in the blood vessels surrounding the alveoli, and internal respiration, in which oxygen is exchanged for carbon dioxide at the cellular level. Cells soon stop functioning and die if they are deprived of oxygen.
The second function of the respiratory system is to maintain the acid-base balance in the body. Failure of this function may result in respiratory acidosis or alkalosis. Respiratory acidosis occurs if the patient experiences hypoventilation and carbon dioxide levels increase in the body, causing hypercapnia. Respiratory alkalosis is related to an excess release of carbon dioxide caused by hyperventilation, which may be associated with anxiety or an acute asthma attack. Both conditions can be life-threatening if the underlying causes are not corrected. The respiratory and circulatory systems work together to supply body cells with oxygen and remove metabolic wastes. The ventilation process is controlled by the respiratory center in the central nervous system and assisted by the intercostal muscles and the diaphragm.
The Respiratory System
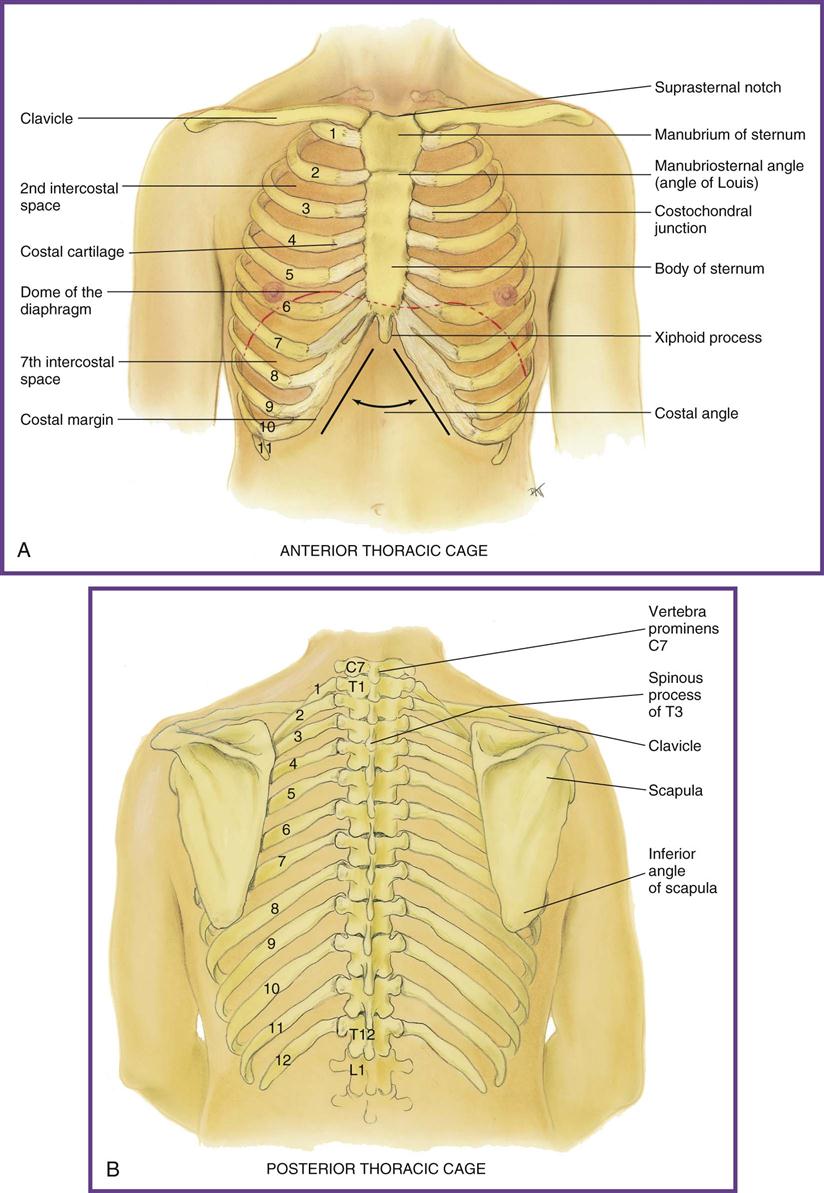
The thoracic cage, sometimes called the rib cage, is a bony structure that is narrower at the top and wider at the base. It is held in place by the thoracic vertebrae of the spine in the center of the back and by the sternum in the center of the anterior aspect of the body. The first seven ribs attach directly to the sternum and are called the true ribs. Ribs 8, 9, and 10 fasten one to another, forming the false ribs, and ribs 11 and 12 are the “floating” ribs, or half ribs, because their only attachment is to the thoracic vertebrae. At the base or floor of the rib cage is the diaphragm, a musculotendinous membrane that separates the thoracic cavity and the abdominal cavity (Figure 46-1). The respiratory system is divided into two anatomic regions, the upper respiratory tract and the lower respiratory tract.
Upper Respiratory Tract
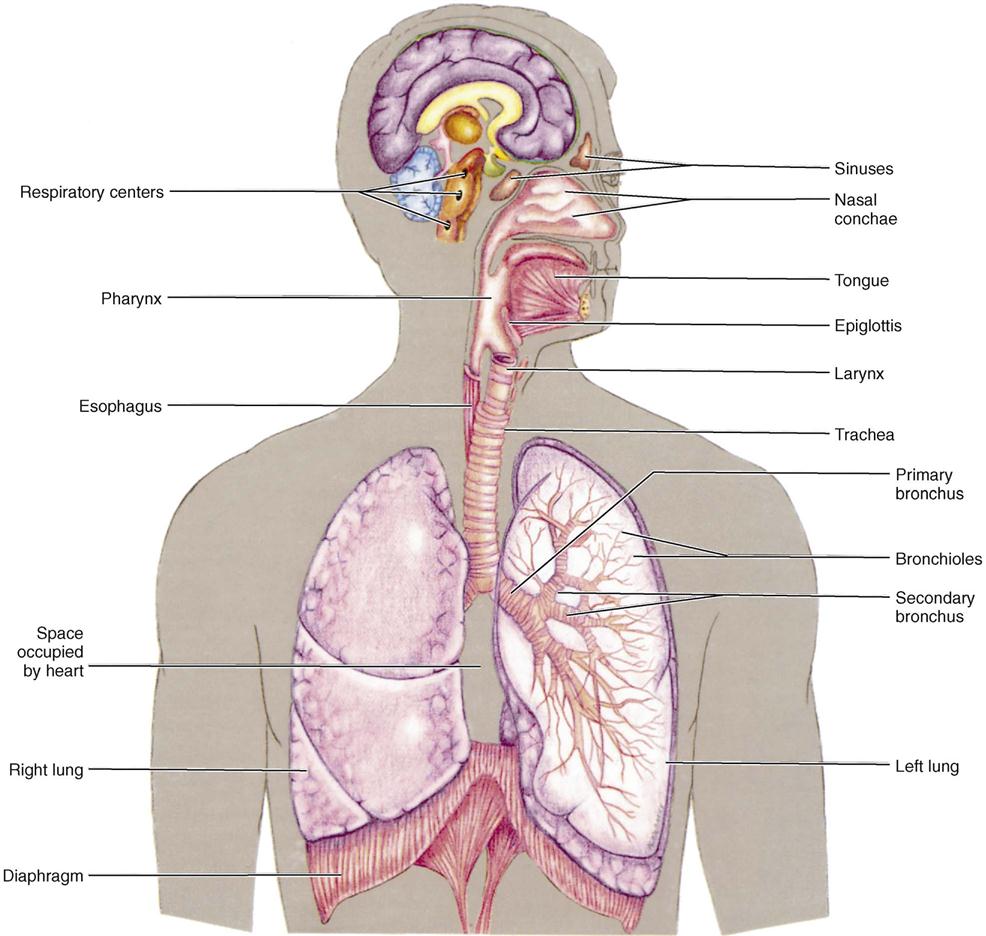
The upper respiratory tract, which transports air from the atmosphere to the lungs, includes the nose, pharynx (throat), and larynx (Figure 46-2). As air enters the nasal cavity, it is cleaned by the cilia, warmed by capillary blood vessels, and moistened by mucous membranes. The paranasal sinuses, hollow cavities that also are lined with mucous cells and cilia, open into the nasal cavity and help warm and moisten inhaled air. The filtered, warmed, and moistened air moves past the tonsils, which have an immunity function and help defend the body from potential pathogens, and through the pharynx. As the air continues toward the lungs, it passes through the larynx. The opening into the larynx is protected by a moveable piece of cartilage, the epiglottis. The larynx, or voice box, is made up of vocal cords, which vibrate when air is exhaled, creating the sound of the voice. Once the air passes through the larynx, it enters the lower respiratory tract.
Lower Respiratory Tract
The lower respiratory tract consists of the trachea, bronchial tubes, and lungs (see Figure 46-2). These structures are also lined with mucous tissue that is covered with cilia. The collection of dust and foreign particles in the cilia initiates the coughing reflex; this helps expectorate mucus, which may contain pathogens. Without these defense mechanisms, pathogens would remain in the lungs and may cause disease. Cigarette smoke and other air pollutants slow or paralyze the cleansing action of the cilia and damage the mucous membrane lining throughout the respiratory tract.
The trachea (windpipe) is a tube that begins at the larynx and extends into the center of the chest, where it divides, or bifurcates, into the right and left bronchi. It is about 5 inches long and is surrounded by C-shaped cartilaginous rings. These rings hold the trachea open regardless of changes in air pressure.
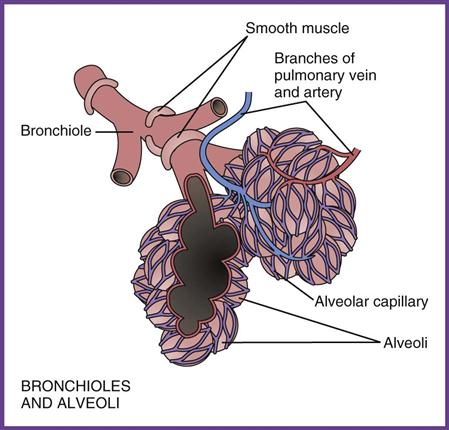
It is often said that the bronchial tubes look like a tree hanging in the chest (Figure 46-3). The right bronchus is wider than the left to accommodate the right lung lobes, which also are larger. This means that foreign substances are more frequently seen in the right bronchus. Once the bronchi enter the lungs, they branch into smaller and smaller passageways, much as blood vessels do in the circulatory system. This branching continues until it becomes microscopic. These very tiny bronchi are called bronchioles. Every bronchiole terminates in microscopic air sacs called alveoli. The alveoli are made of thin tissue, only one cell wall thick that allows for the exchange of oxygen and carbon dioxide through the cell membrane.
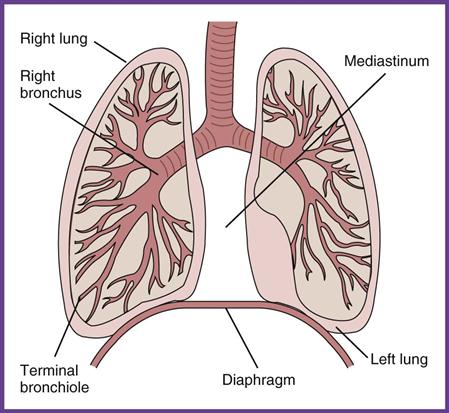
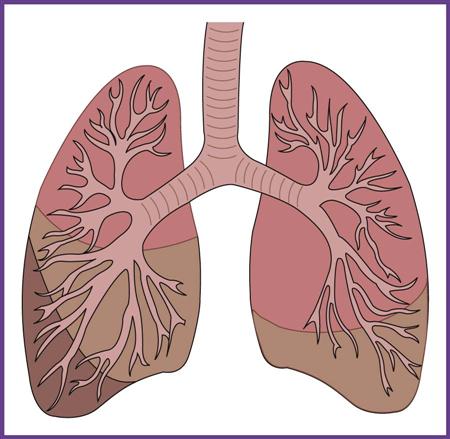
The bronchial tree and alveoli are the major structures housed within the right and left lungs. The lungs are soft and spongy because of the air sacs that make up most of their mass. They hang in the right and left sides of the chest, separated by the pericardial sac, which contains the heart. The right lung is divided into three lobes and has a greater volume capacity than the left lung. Because each lobe has its own bronchus and blood supply, the removal of one lobe (lobectomy) results in little or no damage to the rest of the lung. The left lung is longer and narrower and has a distinct indentation in its center, known as the cardiac notch, where the left ventricle of the heart is located and an apical pulse is heard. The left lung has only two lobes, the upper and lower sections (Figure 46-4).
Each lung is encased in a double-layered sac called the pleural membrane. The membrane closest to the lung is called the visceral pleura, which doubles back to form the parietal pleural membrane. Small amounts of pleural fluid fill the space between the two membranes and provide lubrication for the movement of the lungs during inhalation and exhalation.
Ventilation
In the very delicate lung tissue, the bronchioles deposit oxygenated air into the grapelike structures of the alveoli. Surrounding each alveolus is a network of pulmonary capillaries filled with waste air. The oxygenated air moves through the single-celled walls of the alveoli and into the single-celled walls of the pulmonary capillaries (Figure 46-5). As this is happening, the waste air is forced out of the capillaries, into the alveoli, and then into the bronchioles. This carbon dioxide–oxygen exchange provides oxygen-rich blood that is returned to the heart for distribution throughout the body; carbon dioxide wastes are excreted with exhalation. The process involved in this gaseous exchange is called ventilation. The movement of oxygen from the atmosphere into the alveoli is known as inspiration, and the movement of waste gases from the alveoli into the atmosphere is called expiration.
Inspiration
Inspiration begins with a signal from the medulla oblongata in the brainstem. The signal originates because of a decrease in blood oxygen levels or an increase in carbon dioxide levels. The stimulus is carried by the phrenic nerve to the major muscle of inspiration, the diaphragm. When the diaphragm receives the signal, it flattens out and pulls downward. At the same moment, the intercostal muscles between the ribs contract, causing the ribs to move outward and the chest cavity to enlarge. This movement causes the lungs to expand and increase their volume. The more these muscles are contracted, the deeper the inhalation is and the greater the air volume becomes. Respiratory distress occurs when an individual is unable to move an adequate amount of air into the lungs, using the diaphragm and intercostal muscles, to meet the body’s needs.
Expiration
The second half of ventilation is expiration. Once inspiration is complete, the diaphragm and intercostal muscles relax, causing the diaphragm to move upward into the thoracic cavity and the ribs to move inward, reducing lung capacity. This movement forces the waste air out of the lungs and back into the atmosphere. Expiration requires very little energy and takes place with minimal effort by the body. However, in certain respiratory conditions, such as asthma or emphysema, the person has difficulty getting air out of the lungs, and accessory muscles in the chest and abdomen are needed to assist the intercostal and diaphragm muscles for complete exhalation.
Respiratory System Defenses
Every part of the respiratory system has a defense mechanism. In the upper respiratory tract, the mucus-covered ciliated surface of the mucous membranes trap particles; through the continuous flow of the mucus back toward the nasopharynx, the particles are either sneezed outward or swallowed.
The lower respiratory tract is sterile, which is phenomenal considering that each day these airways are exposed to approximately 10,000 L of air containing an endless number of microorganisms and foreign material. The ever-changing airflow, inspiration to expiration, creates a turbulence that makes remaining in the bronchi very difficult for these invading substances. This, combined with coughing, sneezing, and a functioning immune system, protects the respiratory tract and helps the body maintain homeostasis. Disease occurs when something disrupts the normal homeostatic chain of events.
Major Diseases of the Respiratory System
Many diseases affect the respiratory system. The major ones can be divided into infectious diseases, obstructive disorders, and tumors. Respiratory diseases cause common symptoms, including sneezing, a productive or nonproductive cough, sore throat or hoarseness, fever, general malaise, altered breath sounds, and changes in breathing patterns. The medical assistant must be familiar with common respiratory terms and use them in documenting a patient’s signs and symptoms (Table 46-1).
TABLE 46-1
| MEDICAL TERM | DEFINITION |
| Apnea | Absence of breathing |
| Atelectasis | Collapsed lung |
| Dyspnea | Difficulty breathing |
| Empyema | Accumulation of pus in the pleural space |
| Hemoptysis | Expectoration of blood |
| Hemothorax | Accumulation of blood and fluid in the pleural cavity |
| Hypercapnia | Greater than normal amounts of carbon dioxide in the blood |
| Hyperpnea | Deep, rapid, labored respiration that may occur because of exercise or pain and fever |
| Hypoxemia | Low level of oxygen in the blood |
| Orthopnea | Person must sit or stand to breathe comfortably |
| Pleurisy | Inflammation of the parietal pleura, causing dyspnea and stabbing pain; friction rub may be auscultated |
| Pneumothorax | Collapse of the lung as a result of the collection of air or gas in the pleural space |
| Pyothorax | Collection of pus in the pleural cavity caused by infection |
| Rales | Bubbling or popping sound heard on auscultation; it is produced by the passage of air through bronchi that are constricted or contain secretions |
| Rhinoplasty | Plastic surgery to repair or alter the structure of the nose |
| Rhinorrhea | Excessive drainage from the nose |
| Rhonchi | Continuous rumbling sound heard on auscultation; it is caused by thick secretions or spasms |
| Tachypnea | Abnormally rapid rate of breathing |
| Thoracotomy | Surgical opening into the thoracic cavity |
Infectious Diseases
Respiratory tract infections fall into two categories, depending on their location. Diseases of the nose and upper respiratory tract are more common than diseases of the lower respiratory tract (e.g., pneumonia). Respiratory tract infections account for approximately 75% of all clinically diagnosed infections. Only about 5% of these infections involve the lungs. Most lung infections are seen in hospitalized patients, the elderly, substance abusers, alcoholics, and patients with acquired immunodeficiency syndrome (AIDS). Pneumonia is the seventh leading cause of death in the United States and often is the cause of death for debilitated people.
Upper Respiratory Tract Infections
Common Cold.
The common cold was discussed in Chapter 42 as an acute inflammatory process affecting the mucous membranes that line the nose, pharynx, larynx, and bronchus. Usually the term “cold” is used when only the membranes of the nose and pharynx are affected; however, the same virus can affect the larynx and lungs. The viral invasion can be followed by bacterial infections of the pharynx, sinuses, and middle ear. Common signs of an upper respiratory tract infection (URTI or URI) include nasal congestion and rhinorrhea, sneezing, watery eyes, pharyngitis (sore throat), laryngitis (hoarseness), and coughing. Nasal discharge usually is clear and watery in the early stage but can become greenish yellow as the virus becomes more virulent or when bacteria invade. The patient usually complains of headache, low-grade fever, chills, and anorexia.
Currently there is no cure for the common cold; the infection usually runs its course in 3 to 5 days. The best way to treat it is to get plenty of rest and drink fluids. An over-the-counter (OTC) cold remedy, cough syrup, and acetaminophen may lessen the discomfort of cold-related symptoms. Antibiotics are prescribed only if evidence of a secondary bacterial infection is present. As discussed in Chapter 33, although echinacea may be promoted as an effective preventive and/or treatment for the common cold, most studies show little or no evidence that it is effective.
Sinusitis.
The paranasal sinuses are air-filled spaces in the skull located in the brow area over the eyes, inside each cheekbone, behind the bridge of the nose, and behind the eyes. Each sinus has an opening into the nose for the free exchange of air and is lined with a continuous mucous membrane. Healthy sinuses are sterile, but an infection or an allergic reaction can cause one or more of the sinuses to become inflamed or infected. Inflammation causes edema and the collection of mucus within the sinus cavity, creating a feeling of pressure, nasal congestion or rhinorrhea, and classic sinus headaches. The location of sinus pain depends on the sinus cavity involved but can be described as pain in the forehead (frontal sinuses), upper jaw and teeth discomfort (maxillary sinuses), pain between the eyes (ethmoid sinuses), and/or an earache and neck pain (sphenoid sinuses). The condition is treated with decongestants, antibiotics for bacterial infections, and analgesics. Sinusitis can be acute, lasting 2 to 8 weeks, or chronic, with symptoms lingering much longer.
Allergic Rhinitis (Hay Fever).
Although not caused by a pathogenic organism, allergic rhinitis frequently is confused with infectious disease. This disorder affects millions of people every year. It is caused by a reaction of the nasal mucosa to an environmental allergen. The most common allergen is plant pollen; this is where the term “hay fever” originated. Signs and symptoms include sneezing, nasal congestion, nasal itching, and rhinorrhea. Symptoms can be controlled either with OTC treatments, such as Sudafed, Zyrtec, and fexofenadine hydrochloride (Allegra), or with prescription antihistamines, such as montelukast (Singulair), and fluticasone (Flonase) and cromolyn sodium (Nasalcrom) nasal sprays. The list of possible allergens is extensive. When this condition is seen in the respiratory practice, the patient usually is referred to an allergist for testing and possible immunotherapy.
Patients may have difficulty determining whether symptoms are caused by a cold or an allergy. The condition usually is an allergy if the eyes, ears, nose, throat, and roof of the mouth (palate) are itchy; the eyes are red and watery; a clear, thin nasal discharge is present; symptoms are seasonal and last for weeks or months; and the individual does not have a fever.
Lower Respiratory Tract Infections
Pneumonia.
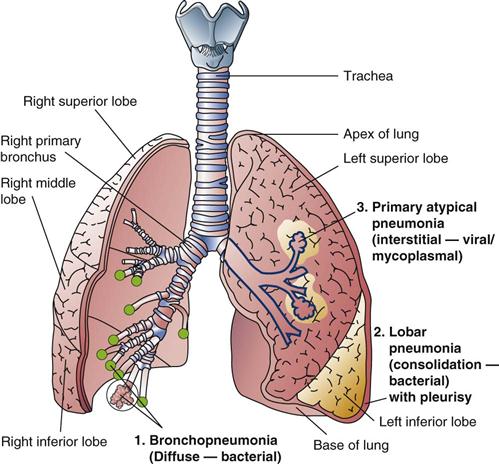
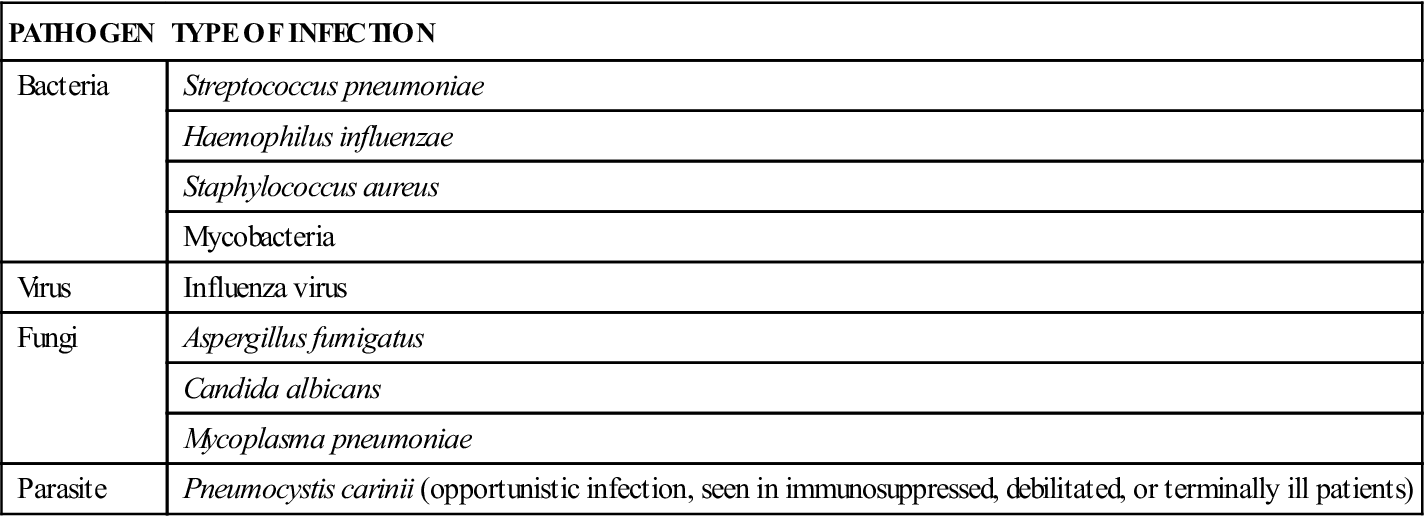
Pneumonia is both a specific disorder and a general term meaning inflammation of all or part of the lungs (Figure 46-6). Pneumonia can be caused by bacteria, viruses, or other pathogens (Table 46-2). It also can be caused by inhalation of irritants or poisonous gas and by aspiration of solids or fluids into the lungs. The most common causative organisms are staphylococci and streptococci.
TABLE 46-2
Pathogens That Cause Pneumonia
| PATHOGEN | TYPE OF INFECTION |
| Bacteria | Streptococcus pneumoniae |
| Haemophilus influenzae | |
| Staphylococcus aureus | |
| Mycobacteria | |
| Virus | Influenza virus |
| Fungi | Aspergillus fumigatus |
| Candida albicans | |
| Mycoplasma pneumoniae | |
| Parasite | Pneumocystis carinii (opportunistic infection, seen in immunosuppressed, debilitated, or terminally ill patients) |
Pneumonia can occur in any age group but most often affects preschoolers and the elderly (over age 65). It can range from a mild complication to a life-threatening illness. Risk factors include smoking, alcoholism, and immunosuppression caused by diseases or treatment. The patient usually comes to the office with symptoms of high fever, chills, and general malaise. Signs of the illness include dyspnea, tachypnea, chest pain during inspiration, and a relentless cough with possible hemoptysis. Auscultation of the chest reveals rales, rhonchi, and other signs of pulmonary consolidation. The infection may spread into the pleural cavity, causing empyema and pleurisy.
The diagnosis is confirmed with a chest x-ray evaluation; sputum culture and sensitivity testing to identify the invading organism and determine the appropriate antibiotic therapy; and a white blood cell (WBC) count, including a differential count to determine whether the pneumonia is viral or bacterial. If the pneumonia is viral, the number of WBCs does not increase; if it is bacterial, the greater the invasion, the higher the WBC count. With bacterial pneumonias, the differential count shows elevated neutrophil and monocyte levels. If the invading organism is bacterial, the treatment of choice is antibiotics and lung function therapy until the patient has recovered. If the organism is viral, the patient is given supportive care, such as antipyretics, fluids, and oxygen, until the immune system can control the spread of the virus.
Tuberculosis.
According to the Centers for Disease Control and Prevention (CDC), approximately one third of the world’s population is infected with tuberculosis (TB). TB causes more deaths than any other infectious agent in the world. For more than 50 years, the incidence of TB in the United States steadily declined; however, from the late 1980s through the 1990s, a resurgence in reported cases occurred. This increase was believed to be the result of increased travel and immigration; the number of individuals with AIDS, who have little resistance to disease; an increase in the number of homeless and malnourished people; and the overwhelming proliferation of drug-resistant TB bacilli. An international TB vaccine, bacille Calmette-Guérin (BCG), is available, but it is rarely used in the United States. The vaccine does not always provide protection from the disease and those who are vaccinated may have a positive Mantoux test result.
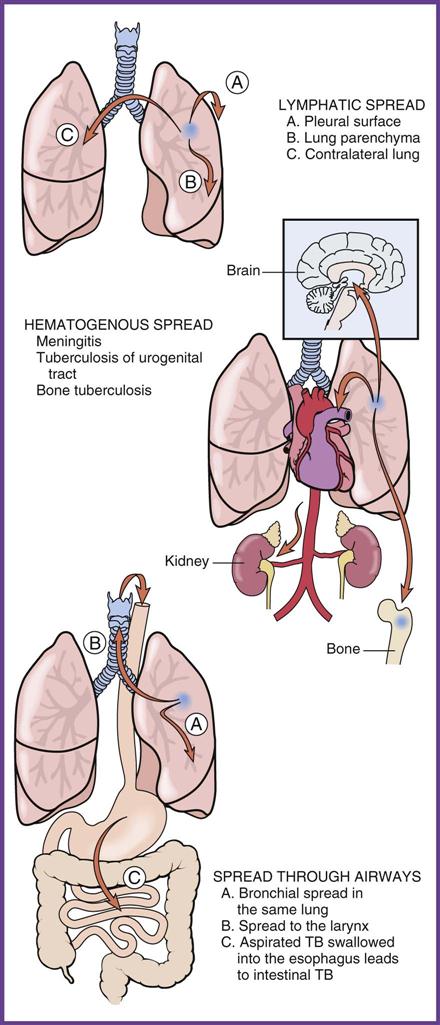
TB is caused by the bacterium Mycobacterium tuberculosis. This organism is covered with a waxy substance that enables it to survive outside a living host for a long time. It is transmitted by droplets of sputum expectorated into the environment by an infected host that are inhaled by another person. In the warm, moist respiratory tract, these organisms again can become active if the individual is susceptible to the disease. TB also can be spread when an infected person coughs or sneezes, releasing airborne infected droplets, which are inhaled and cause an infection if the person is susceptible.
TB develops in two stages. The primary infection occurs when the person is first infected with the bacteria and the lungs become inflamed. Cell-mediated immunity ensues, isolating the bacteria and forming a tubercle. At this point a healthy individual can stop the spread of infection, causing the TB bacillus in the tubercle to become inactive. In this case, the person was exposed to the pathogen but never developed active disease and so is said to have a latent TB infection. Individuals with latent TB are asymptomatic and are not infectious. However, because an exposed person develops antibodies to the disease, he or she consistently tests positive on TB skin screening tests. Therefore, rather than the purified protein derivative (PPD), or Mantoux test, these patients should have chest x-ray studies to diagnose active TB.
At any time the bacilli in the tubercles can be reactivated, and secondary, or active, TB can develop. The patient now is actively infected with the disease, which can spread to the bones, brain, and kidneys (Figure 46-7). Some people develop active TB soon after becoming infected, before the immune systems can fight the TB bacteria; others develop it later in life, when the immune systems are weakened for other reasons.
TB is diagnosed most frequently in people living in crowded conditions with poor hygiene, those who are malnourished, and those who have other chronic conditions. It spreads most rapidly in large cities, in the elderly, alcoholics, and the homeless. Symptoms of an active infection include an intermittent fever that peaks in the afternoon, night sweats, weight loss, and general malaise. As the infection becomes virulent in the host, a productive cough develops, and thick, dark, frequently blood-tinged mucus is expectorated.
The primary diagnosis of TB is established through the patient’s signs and symptoms. The infection is suspected with a positive chest x-ray film but is confirmed with a sputum culture. Traditional culture methods originally took 4 to 6 weeks, and this extended period allowed a potentially infectious individual to continue to spread the disease. New culture techniques identify the bacterium in as little as 36 to 48 hours. The physician also may order a blood test, the QuantiFERON-TB Gold test (QFT), to diagnose TB infection. The QFT measures the response to TB proteins when they are mixed with a small amount of blood. A two-step Mantoux test is recommended for individuals who are over age 45 and have never had a Mantoux test; those who have been vaccinated with BCG; and employees of hospitals and long-term care facilities. For this test, the initial intradermal skin test is administered and read in 48 to 72 hours. If the result is negative, a second Mantoux is performed on the opposite arm 1 to 3 weeks after the first test and again read in 48 to 72 hours.
Once a diagnosis of TB has been confirmed, the patient is prescribed long-term treatment with a combination of drugs to eradicate the bacilli. If the patient has tested positive for TB but does not have an active infection, the physician prescribes isoniazid (INH) and rifampin (RIF) for 6 months to treat any possible tubercle formations. If the patient has active pulmonary TB, the CDC recommends a four-drug regimen—INH, RIF, pyrazinamide, and ethambutol—daily for 2 months; this is then reduced to two drugs for an additional 4 to 7 months, depending on sputum culture outcomes. It is crucial that patients being treated with TB medications strictly comply with medication orders to prevent the creation of multidrug-resistant TB (MDR-TB). Resistant strains of TB develop because of skipped doses or failure to take the medication as long as prescribed. MDR-TB requires at least 2 years of drug therapy with medications that can cause serious side effects, especially liver damage. All tuberculin-negative healthcare workers should have a PPD annually; workers who show a positive reaction but are not actively infected with TB should have an annual chest x-ray evaluation to screen for the disease.