Assisting in Endocrinology
Learning Objectives
1. Define, spell, and pronounce the terms listed in the vocabulary.
2. Apply critical thinking skills in performing the patient assessment and patient care.
3. Summarize the anatomy and physiology of the endocrine system.
4. Explain the mechanism of hormone action.
5. Differentiate among the diseases and disorders of the endocrine system.
6. Describe the diagnostic criteria for diabetes mellitus.
7. Compare and contrast prediabetes, diabetes type 1, diabetes type 2, and gestational diabetes.
8. Outline the treatment plan and management of the different types of diabetes mellitus.
9. Perform blood glucose screening with a glucometer.
10. Identify the characteristics of hypoglycemia and hyperglycemia.
11. Describe the complications associated with diabetes mellitus.
12. Summarize patient education approaches to diabetes.
Vocabulary
adrenocorticotropic hormone (ACTH) (uh-dren-o-cor-ti-ko-tro′-pik) A hormone that stimulates the production and secretion of glucocorticoids; it is released by the anterior pituitary gland.
follicle-stimulating hormone (FSH) A hormone secreted by the anterior pituitary; it stimulates oogenesis and spermatogenesis.
gluconeogenesis (glu-kuh-ne-uh-je′-nuh-suhs) The formation of glucose in the liver from proteins and fats.
glycogen The sugar (starch) formed from glucose; it is stored mainly in the liver.
glycosuria The abnormal presence of glucose in the urine.
growth hormone (GH) Also called somatotropic hormone; it stimulates tissue growth and restricts tissue glucose dependence when nutrients are not available.
luteinizing hormone (LH) (lu-te-uh-niz′-ing) A hormone produced by the anterior pituitary gland that promotes ovulation.
nocturia Excessive urination during the night.
polyphagia (pah-le-faj′-e-uh) Increased appetite.
prolactin (PRL) A hormone secreted by the anterior pituitary gland that stimulates the development of the mammary gland.
satiety The state of being satisfied or feeling full after eating.
specific gravity The density of urine compared with an equal volume of water.
thyroid-stimulating hormone (TSH) A hormone secreted by the anterior pituitary gland that stimulates the secretion of hormones produced by the thyroid gland.
Scenario
Miguel Vasco has been a certified medical assistant (CMA [AAMA]) for 10 years and has worked for the past 3 years with a multiphysician endocrinology and internal medicine practice. Although he has taken care of patients with many different disorders of the endocrine system, most of the practice’s patients are individuals with diabetes mellitus type 2. One of Miguel’s responsibilities is teaching patients newly diagnosed with diabetes how to monitor their blood glucose levels and maintain a healthy lifestyle.
While studying this chapter, think about the following questions:
• What are the primary responsibilities of a medical assistant in an internal medicine practice?
• What clinical skills are required in this specialty practice?
• What diagnostic and treatment procedures typically are used in an endocrinology practice?
Individuals with disorders of the endocrine system usually are seen first by the primary care physician (PCP), who may refer them to an internist or an endocrinologist for specialized care. Patients with certain endocrine disorders, such as diabetes mellitus (DM), also may be seen in a clinic for follow-up and treatment. A medical assistant employed in any of these ambulatory care settings assists with diagnostic procedures, specialized examinations, and patient education. It is important that medical assistants recognize the dynamics of endocrine system diseases so that they can help patients understand how to administer their medications and prevent long-term complications from the disease.
Anatomy and Physiology of the Endocrine System
Both the nervous system and the endocrine system control the body’s physiologic responses to internal and external stimuli. The nervous system is electrical in nature and sends immediate messages along a nerve pathway to evoke a response; the endocrine system relies on the bloodstream to carry hormonal messages to a target cell for action. Through hormonal action, the endocrine system regulates all body functions. Endocrinology is the study of hormones, their receptor cells, and the results of hormone action.
The word part endo- means “in” or “within”; the suffix -crine means “secrete.” The endocrine system consists of glands located throughout the body that produce and secrete chemicals known as hormones. Hormones are excreted directly into the bloodstream, which carries them to the target tissue. Hormones function as the body’s chemical messengers, transferring information from one group of cells to another. Hormones control growth, mood, system functions, metabolism, sexual maturity, and reproduction. Hormone levels vary and can be affected by outside factors such as illness and stress.
Basic Anatomy
Glands are categorized as either exocrine or endocrine. Exocrine glands, such as sweat glands and salivary glands, secrete either through a duct or directly onto the surface of the skin or in the mouth. Endocrine glands release hormones directly into the bloodstream, which transports the hormones to target cells for action.
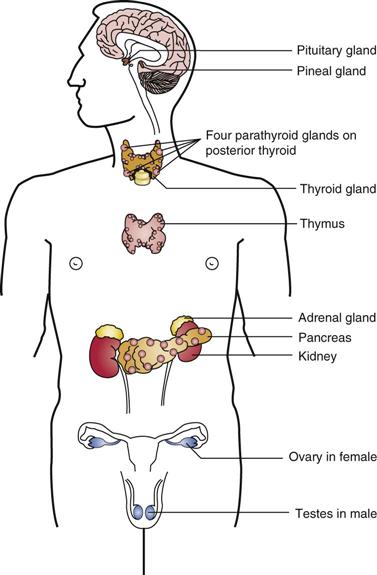
The glands of the endocrine system are the hypothalamus, pituitary, pineal gland, thyroid, parathyroids, thymus, and adrenals and the reproductive glands (i.e., the ovaries and the testes) (Figure 45-1). Some nonendocrine organs, especially the pancreas, also can produce and release hormones. The hypothalamus, located in the inferior midportion of the brain, is the major connection between the nervous and endocrine systems. The hypothalamus controls the action of the pituitary, a pea-sized gland located below the hypothalamus. The pituitary often is called the “master gland” because it secretes hormones that regulate multiple endocrine glands.
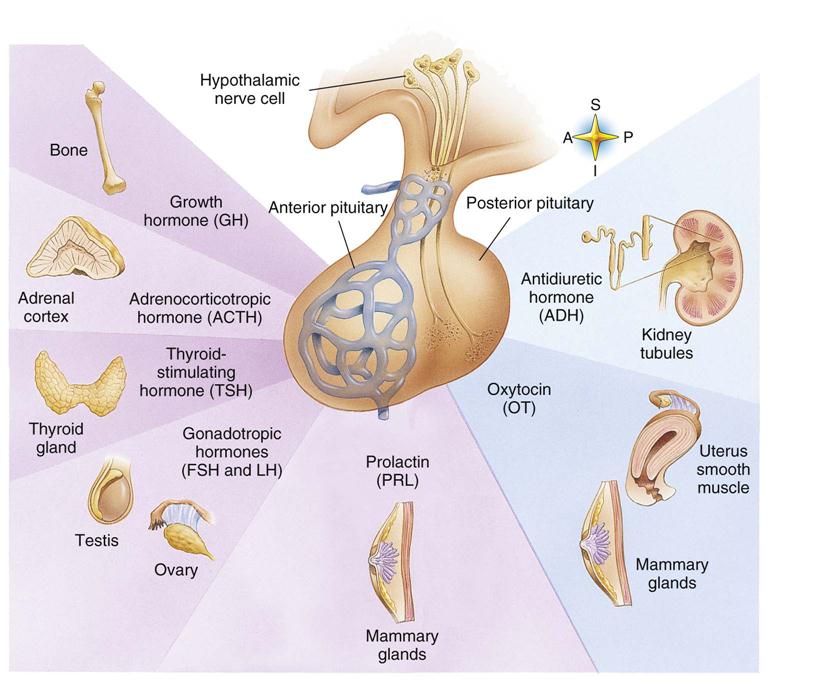
The pituitary gland is separated into two parts, the anterior and posterior lobes. The anterior pituitary, or adenohypophysis, regulates the functions of the thyroid, adrenals, and reproductive glands. It produces growth hormone (GH), thyroid-stimulating hormone (TSH), adrenocorticotropic hormone (ACTH), prolactin (PRL), follicle-stimulating hormone (FSH), and luteinizing hormone (LH). The posterior lobe of the pituitary, or neurohypophysis, excretes oxytocin, which stimulates the contractions of the smooth muscle of the uterus that occur during labor and the flow of breast milk toward the nipple when an infant breastfeeds. The posterior pituitary also produces antidiuretic hormone (ADH), which helps control fluid balance by acting on the kidneys to reabsorb fluid as needed to maintain homeostasis (Figure 45-2).
The pineal gland, which is located deep within the brain, excretes the hormone melatonin. Melatonin helps regulate waking and sleeping patterns and also may affect seasonal reactions to alterations in the availability of sunlight.
When stimulated by TSH, the thyroid gland produces the thyroid hormones triiodothyronine (T3) and thyroxine (T4), which control the body’s metabolic rate and are important factors in bone growth and nervous system development in children. On the dorsal aspect of the thyroid gland are several small parathyroid glands, which release hormones (parathyroid and calcitonin) that regulate the level of calcium in the blood. The parathyroid hormone (PTH) maintains a constant concentration of calcium in the body by regulating the absorption of calcium from the gastrointestinal tract and stimulating the reabsorption of calcium stored in the bone as needed to maintain homeostasis. Calcitonin stimulates deposition of calcium into the bone when excess amounts of calcium are available.
The thymus gland, located behind the upper portion of the sternum, produces hormones that stimulate the production of specialized immune system cells called T cells. The thymus gland is present at birth, enlarges as the child ages, but begins to atrophy as the child reaches puberty. It once was thought that the thymus played no role in the physiology of adults, but we now know that its hormone action is crucial to T-cell maturation. (T cells are discussed in further detail in Chapter 54.)
On top of each kidney are the adrenal glands, which are triangular-shaped glands consisting of an outer layer, called the adrenal cortex, and an inner body, called the adrenal medulla. The adrenal cortex secretes corticosteroid hormones, including cortisol, aldosterone, and adrenal androgens, all of which influence a wide range of bodily functions. The adrenal medulla produces epinephrine, also called adrenaline, which activates the body’s reaction to stress.
The gonads produce sex hormones. The male gonads are the testes; they secrete testosterone, which regulates the development of secondary sexual characteristics, such as voice changes and the growth of facial and pubic hair, and promotes the production of sperm. The female gonads, the ovaries, produce eggs or ova (oogenesis) and secrete estrogen and progesterone. The female hormones control the development of breast tissue and other secondary sexual characteristics, regulate menstruation, and play important roles during pregnancy.
The pancreas performs essential endocrine functions by producing insulin and glucagon, which work together to maintain normal blood glucose levels and store glucose for energy.
Mechanisms of Hormone Action
The goal of hormone regulation is to maintain homeostasis. Hormone secretion is regulated by a number of mechanisms, including nervous stimulation, endocrine control (a hormone from one gland, such as the anterior pituitary, stimulates the release of a hormone from another gland), and feedback systems. An example of nervous system regulation of endocrine function is the release of adrenaline from the adrenal medulla in response to stimulation from the sympathetic nervous system during a stressful episode. In the most common feedback system, negative feedback, an endocrine gland is activated by an imbalance and acts to correct the imbalance by stopping the secretion process. For example, if calcium blood levels fall below normal, the parathyroid glands are stimulated to release PTH. PTH acts to increase blood calcium levels either by stimulating the absorption of calcium from the gut or by demineralizing bone to release stored calcium. This change in the blood calcium level is detected by the parathyroid gland, which then stops production of PTH.
Each hormone released into the bloodstream has particular target cells for action. The target cells have receptors that attract only specific hormones and permit the hormone to pass through the cell membrane and affect cellular action.
Diseases and Disorders of the Endocrine System
Faulty secretion of any hormone, whether too much or too little, can cause health problems for patients. The goal of treatment is either to control the hypersecretion of hormones or to replace hormones that are not being secreted at therapeutic levels.
Posterior Pituitary Gland Disorder
Diabetes Insipidus
When ADH (or vasopressin) is not produced or released in sufficient amounts, the patient develops a condition called diabetes insipidus. ADH increases the permeability of the renal tubules and the collecting tubules in the kidneys, permitting fluid to be reabsorbed and causing the urine to become more concentrated. Without the action of ADH, fluid is not reabsorbed from the renal tubules, which causes a large amount of fluid to be excreted in the urine, with the potential onset of dehydration. A lack of ADH results from a tumor either in the hypothalamus or the posterior pituitary gland, or diabetes insipidus may develop because of an inadequate response to ADH in the renal tubules.
Diabetes insipidus usually has an acute onset, and the patient presents with polyuria, polydipsia, nocturia, low urine specific gravity, and high blood plasma osmolality (concentration). It can result in fatal dehydration if fluid and electrolyte levels cannot be controlled. Replacement therapy with a synthetic vasopressin (desmopressin) nasal spray, oral tablets, or injections can be used to treat the disorder.
Diseases of the Anterior Pituitary
Hormones secreted by the anterior pituitary control a number of glandular functions. The effects on the body of changes in anterior pituitary gland secretion depend on whether the hormones are produced at an abnormally low level (hypopituitarism) or at a very high level (hyperpituitarism). A patient diagnosed with panhypopituitarism has a deficiency of all the hormones produced by the anterior pituitary, and the symptoms reflect systemic inactivity of all the glands stimulated by the anterior pituitary hormones.
Growth Hormone Abnormalities
Hypopituitary dwarfism occurs when the pituitary gland fails to produce normal amounts of GH. The child’s height is impaired, but he or she will have a normal-sized head and trunk. Hypersecretion of GH causes two different disorders, depending on the patient’s developmental age. Oversecretion of GH in childhood, before closure of the epiphyseal plates in the long bones, causes the long bones to grow excessively. Affected individuals may reach a height of 8 feet or taller. Because GH has a secondary effect on the blood glucose level, these individuals may develop diabetes mellitus. Slow-growing, benign anterior pituitary adenomas frequently are the cause of gigantism, and treatment consists of removing the tumor if possible and radiation therapy or drug therapy.
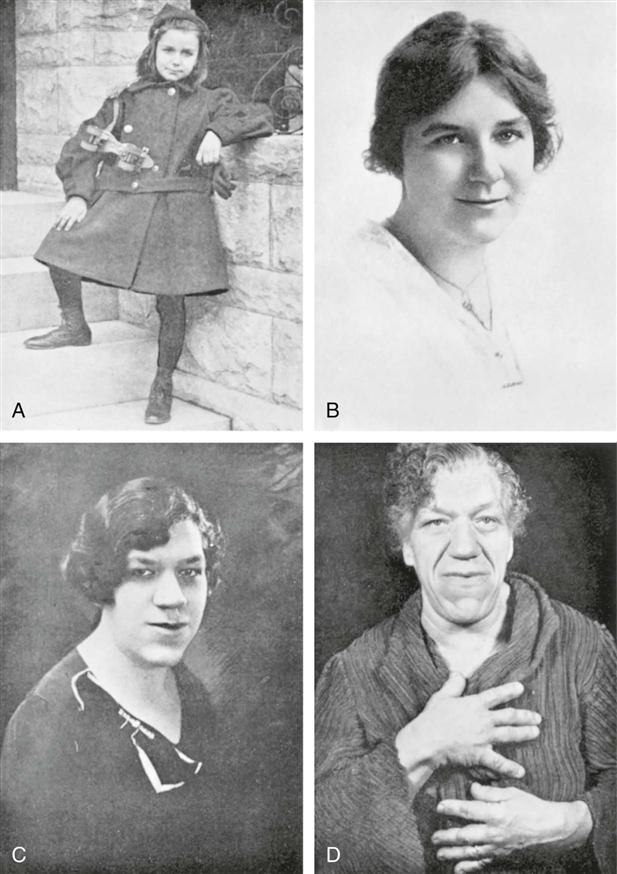
If hypersecretion of GH occurs in adulthood, the disorder is called acromegaly. Because the epiphyseal plates are closed, the long bones cannot grow. Consequently, a wide range of manifestations can occur because of excessive connective tissue growth and overproduction of bone. Signs and symptoms include arthralgia, an enlarged tongue, overactive sebaceous and sweat glands, coarse skin, excessive body hair, and nerve damage caused by pressure on peripheral nerves from increasing amounts of bone and soft tissue. A gradual but noticeable enlargement occurs in the bones of the jaw, face, hands, and feet (Figure 45-3). Advanced acromegaly causes complications such as congestive heart failure, DM, cerebrovascular abnormalities, and neurologic symptoms as the tumor grows within the confined space of the hypothalamus. Treatment of acromegaly requires either surgical removal or irradiation of the pituitary tumor.
Disorders of the Thyroid
Hypothyroidism
Deficient secretion of the thyroid hormones may result from a number of factors. One cause of hypothyroidism is endemic iodine deficiency, a lack of iodine in the diet, resulting in the formation of a simple goiter. A simple goiter is any thyroid enlargement that has not been caused by an infection or neoplasm. Endemic goiters occur in certain geographic areas. If more than 10% of the children 6 to 12 years of age in a particular area have goiters, that geographic location is defined as endemic for goiters.
T3 and T4 are produced in the thyroid gland from iodine and are responsible for the regulation of metabolic activities in all body cells. When the thyroid gland is unable to obtain sufficient amounts of iodine from the circulating blood, it enlarges, or hypertrophies, in an attempt to produce the hormones needed by the body. A decreased amount of thyroid hormones results in a lower metabolic rate, heat loss, and poor mental and physical development. Iodine deficiency is rare in the United States because of the widespread use of iodized table salt and the distribution of foods from iodine-rich areas. The treatment for a simple goiter is to reduce its size by prescribing dietary supplements of iodine, thyroid hormone replacement, or surgery.
Improper development of the thyroid in an infant or young child usually is congenital. The absence of adequate levels of thyroid hormones results in a condition known as cretinism. Newborns have feeding problems, constipation, and a hoarse cry and sleep for extreme lengths of time. Symptoms include lethargy, bradycardia, stunted skeletal growth, and varying degrees of mental retardation, depending on the severity and the length of the hypothyroidism.
When severe or chronic hypothyroidism occurs in an adult or older child, the condition is called myxedema. The patient shows fatigue, weight gain, hair loss, a slower pulse rate, a lowered body temperature, muscle cramps, menorrhagia, and thick, dry, puffy skin. Routine tests to diagnose hypothyroidism include radioimmunoassay, a radiologic blood test, for T3, T4, and TSH. Adequate doses of thyroxine (Levothroid, Levoxyl, or Synthroid) restore normal function and appearance. Patients diagnosed with hypothyroidism must take hormone replacement therapy daily for the rest of their lives.
Hyperthyroidism
Thyrotoxicosis, a condition in which the serum levels of thyroid hormones are excessively high, can also be caused by a number of factors. Symptoms include weight loss, tachycardia, palpitations, hypertension, agitation, nervousness, depression, tremor, excessive sweating, goiter, and exophthalmia (protruding eyes) (Figure 45-4). Graves’ disease, an autoimmune disorder that stimulates overactive thyroid hormone production, is the most common cause of thyrotoxicosis. The goal of treatment is to control excessive thyroid hormone production through drug therapy (methimazole and propylthiouracil); radioactive implants to destroy part of the gland; ingestion of radioactive iodine, which concentrates in the thyroid gland, causing it to shrink; or thyroidectomy, which is the surgical removal of a section of the gland. After irradiation or surgical removal of part of the thyroid gland, the patient’s thyroid hormone levels are evaluated. The patient often must receive replacement hormone therapy (Levothroid, Levoxyl, or Synthroid) postoperatively to maintain normal thyroid hormone levels. Individuals who develop exophthalmia from hyperthyroidism may require orbital decompression surgery, in which the bone between the eye socket and sinuses is removed, giving the eyes room to return to their normal position.
Disorders of the Adrenal Glands
Adrenal insufficiency is called Addison’s disease. This condition is relatively rare and is caused by an autoimmune reaction that affects the adrenal cortex, which secretes corticosteroid hormones. Symptoms include hypoglycemia, increased pigmentation of the skin, muscle weakness, gastrointestinal disturbances, and fatigue. Cortisol and aldosterone deficiencies lead to retention of potassium and the excretion of water and sodium in the urine. Severe dehydration, low blood volume, low blood pressure, and circulatory shock can occur. Treatment includes replacement of cortisol with the long-term daily administration of glucocorticoids (e.g., prednisone) and replacement of aldosterone with fludrocortisone (Florinef) to control sodium and potassium levels while helping to maintain normal blood pressure levels. Patients should also be encouraged to eat a diet high in complex carbohydrates and protein and to maintain an adequate fluid intake. Patients with Addison’s disease are at risk for addisonian crisis, a life-threatening drop in blood pressure, hypoglycemia, and high blood potassium levels. A crisis can be brought on by stressful situations, infections, minor illness, or surgery. Treatment requires immediate administration of an intravenous saline and dextrose solution with corticosteroids.
Hypersecretion of the adrenal cortex, causing increased levels of cortisol, is known as Cushing’s syndrome. Usually a benign pituitary tumor causes the release of excessive amounts of ACTH. Symptoms associated with Cushing’s syndrome may be seen in individuals taking corticosteroids for medical reasons, such as organ transplantation, severe asthma, or rheumatoid arthritis. Excessive levels of cortisol cause an accumulation of adipose tissue in the trunk, a round, or “moon,” face, and fat pads in the cervical spine region, causing the formation of a “buffalo hump” (Figure 45-5). The patient also has glucose intolerance because of insulin resistance at the target cell level.
Additional symptoms include hyperpigmentation, muscle wasting, problems with wound healing, hypertension, kidney stones, and osteoporosis. Female patients have menstrual irregularity, and many patients with Cushing’s syndrome experience mental disorders such as irritability, depression, or severe psychiatric disorders. Treatment depends on the cause of the disorder; it includes medication to control cortisol levels, radiation therapy to reduce the size of the tumor, and surgery to remove the tumor.
Endocrine Dysfunction of the Pancreas: Diabetes Mellitus
Diabetes mellitus is a common hormonal imbalance that has reached epidemic proportions in the United States. Approximately 24 million Americans, or close to 8% of the population, have DM, and the number is growing. Diabetes occurs in people of all ages and races but is more common in older adults (23% of individuals over age 60) and in African-Americans, Latinos, Native Americans, and Asian-Americans/Pacific Islanders. DM is characterized by chronic hyperglycemia and problems with carbohydrate metabolism. This problem with glucose management is caused by a lack of insulin production and/or resistance to insulin at the target cell level. The pancreas contains islets of Langerhans, which produce and secrete the hormones insulin and glucagon. When the blood glucose level is too high, beta islet cells secrete insulin, which is sent through the bloodstream to the target tissue site to conduct glucose into the cell. When blood glucose levels are low, glucagon is secreted by the alpha islet cells to stimulate the liver to convert glycogen (stored glucose) into circulating glucose.
If there is resistance to insulin at the target cell membrane or if not enough insulin is available to help transport glucose from the blood into the cells, the person experiences a variety of symptoms, including glycosuria, polyuria, polydipsia, polyphagia, rapid weight loss, drowsiness, fatigue, itching of the skin, visual disturbances, and skin infections. The American Diabetes Association has identified four major types of diabetes: prediabetes, DM type 1, DM type 2, and gestational diabetes. If left untreated or managed poorly, DM can have serious, life-threatening consequences, such as cardiovascular disease, stroke, hypertension, blindness, kidney disease, nervous system disorders, amputations, pregnancy complications, and diabetic coma. Patient education is crucial for compliance with treatment and prevention of life-threatening complications.