Janice Cuzzell and M. Linda Workman
Assessment of the Skin, Hair, and Nails
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
8 Compare the structures and function of the epidermis, dermis, and subcutaneous tissue.
9 Use proper terminology to communicate skin assessment findings.
11 Use the ABCDE method of assessing skin lesions for cancer.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
The integumentary system includes the skin, hair, and nails. The skin plays a major role in the concept of body protection. As shown in Fig. 26-1, the skin protects against foreign invasion by providing a first line of defense (the moat), a second line of defense (the castle wall), and even a third line of defense (the knights and soldiers). The normal flora on the surfaces of skin and mucous membranes repels some of the more harmful microorganisms. Intact skin has barrier functions, alarm functions, and even combat functions. Specialized cells called Langerhans’ cells, present in the skin, engulf foreign substances (antigens) that invade the body when the skin is injured. These cells then alert the immune system to the presence of the invader.
The skin is the largest organ of the body and plays a major role in homeostasis. When intact, it helps regulate body temperature and maintains fluid and electrolyte balance. Changes in the skin can communicate information about a person’s health and well-being (Anderson et al., 2007).
Emotional stress, systemic disease, and skin injury or disease can alter the function, appearance, and texture of the skin. Therefore examine the skin for important clues about the patient’s health.
The sensory function of the skin allows the use of touch as a therapeutic intervention to provide comfort, relieve pain, and communicate caring. Because the skin has many sensory receptors, the patient can report subjective skin sensations that might indicate specific health problems.
Anatomy and Physiology Review
Structure of the Skin
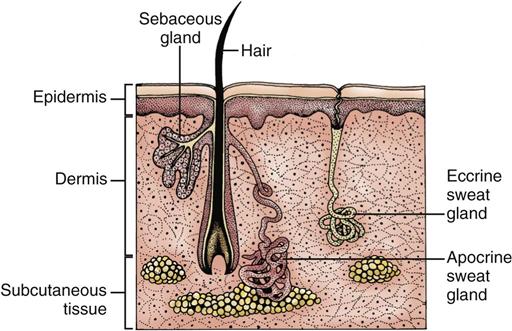
As shown in Fig. 26-2, the skin has three layers: subcutaneous tissue (fat), dermis, and epidermis. Each layer has unique properties that contribute to the skin’s ability to maintain its complex functions.
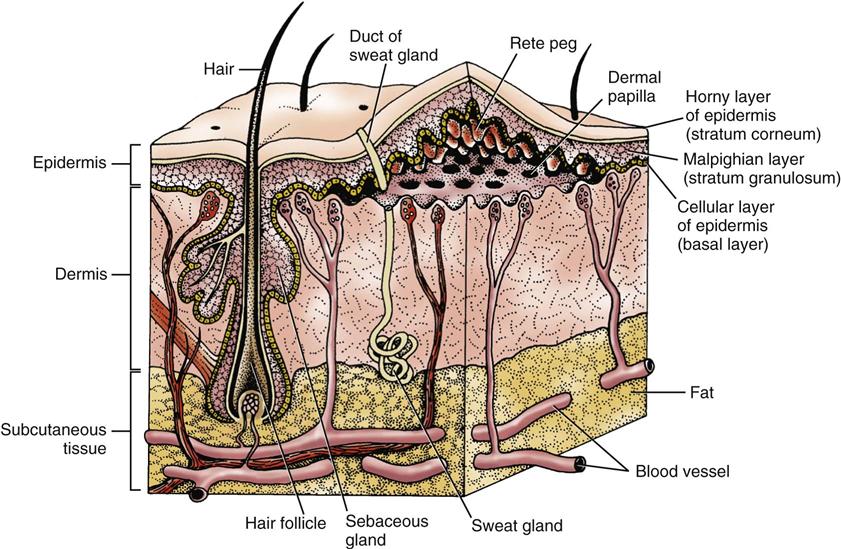
Subcutaneous fat (adipose tissue [fat]) is the innermost layer of the skin, lying over muscle and bone. Fat cells serve as an energy reserve in the event extra calories are needed to power the body. These cells also act as heat insulators for the body. They absorb shock and protect against injury by padding internal structures. Fat distribution varies with body area, age, and gender. Many blood vessels go through the fatty layer and extend into the dermal layer, forming capillary networks that supply nutrients and remove wastes.
The dermis (corium) is the layer above the fat layer. It is composed of connective tissue that contains no cells. The dermis is composed of collagen and elastic fibers that are interwoven to give the skin both flexibility and strength.
Collagen, the main component of dermal tissue, is a protein formed by dermal cells called fibroblasts. Collagen production increases in areas of tissue injury and helps form scar tissue. Fibroblasts also produce ground substance, a protein lubricant that surrounds the dermal cells and fibers and contributes to the skin’s normal suppleness and turgor.
The elasticity of the skin depends on both the amount and quality of the elastic fibers, which are scattered among the collagen fibers. The major component of the elastic fiber is elastin.
The dermis has capillaries and lymph vessels for the exchange of oxygen and heat. The dermis is also rich in sensory nerves that transmit the sensations of touch, pressure, temperature, pain, and itch.
The epidermis is the outermost skin layer. It is anchored to the dermis by finger-like projections of dermal tissue (dermal papillae). The fingers of epidermal tissue that project into the dermis are called rete pegs. The epidermis is less than 1 mm thick, but it is the protective barrier between the body and the environment.
The epidermis does not have its own blood supply and receives its nutrients by diffusion from the blood vessels in the dermal layer through the basement membrane. Attached to the basement membrane are the keratinocytes, the actual skin cells. The keratinocytes capable of cell division are the basal cells, which are located closest to the basement membrane and continuously divide to form new cells. Older keratinocytes are pushed upward and flattened to form the stratified layers of the epithelium (malpighian layers). When these cells reach the outermost skin layer, the stratum corneum (horny layer), they are no longer living cells and are shed from the skin. Keratin, the protein produced by keratinocytes, makes the horny layer waterproof. A keratinocyte takes about 28 to 45 days to move from the basement membrane to the skin surface.
Vitamin D is activated in the epidermis by ultraviolet (UV) light, such as sunlight. It is then distributed by the blood to the intestinal tract, where it promotes uptake of dietary calcium.
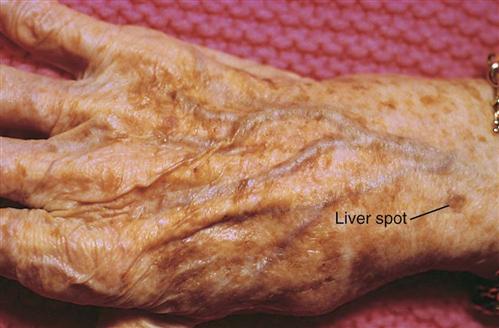
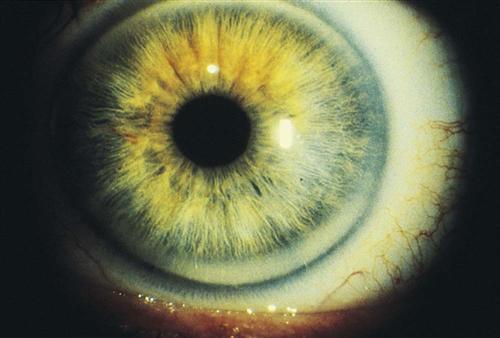
Melanocytes are pigment-producing cells found at the basement membrane. These cells give color to the skin and account for the ethnic differences in skin tone. Darker skin tones are not caused by increased numbers of melanocytes; rather, the size of the pigment granules (melanin) contained in each cell determines the color. The purpose of melanin is to protect the skin from damage by UV light. For this reason, people with dark skin are less likely to develop sunburn than lighter-skinned people with the same sun exposure. Freckles, birthmarks, and age spots are caused by patches of melanin within the skin. UV light stimulates the production of melanin, which protects against the harmful effects of sun exposure. Melanin production increases in areas that have endocrine changes or inflammation.
Structure of the Skin Appendages
Hair, a thick protective pelt worn by most mammals, is mainly a cosmetic feature for modern humans. Hair growth varies with race, gender, age, and genetic predisposition. Individual hairs can differ in both structure and rate of growth, depending on body location.
Hair follicles are located in the dermal layer of the skin but are actually extensions of the epidermal layer (see Fig. 26-2). Within each hair follicle, a round column of keratin forms the hair shaft. Hair keratin is tougher than skin keratin. Hair color is genetically determined by a person’s rate of melanin production.
Hair growth occurs in cycles, with a growth phase followed by a resting phase. Stressors can alter the growth cycle and result in temporary hair loss. Permanent baldness, such as male pattern baldness, is inherited and is seldom influenced by personal or environmental factors.
Nails on fingers and toes have cosmetic value and are useful for grasping and scraping. Like hair follicles, the nails are extensions of the keratin-producing epidermal layers of the skin.
The white, crescent-shaped portion of the nail at the lower end of the nail plate is called the lunula and is the location of the nail matrix, where nail keratin is formed and nail growth begins (Fig. 26-3). Nail growth is a continuous but slow process. Fingernail replacement requires 3 to 4 months. Toenail replacement may take up to 12 months.
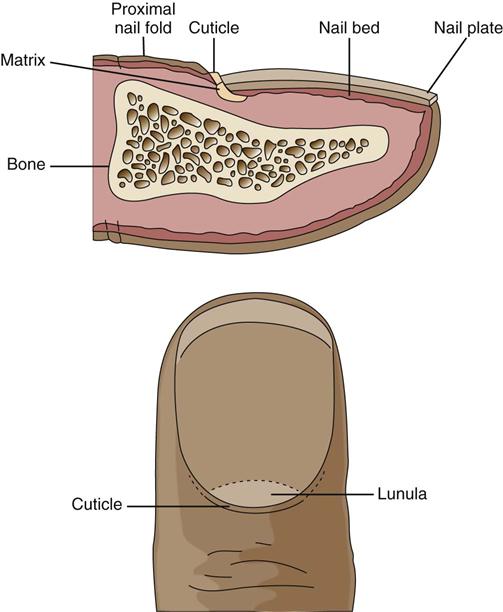
The cuticle, a layer of keratin at the nail fold, attaches the nail plate to the soft tissue of the nail fold. The nail body is translucent, and the pinkish hue reflects a rich blood supply beneath the nail surface. Nail growth and appearance are often altered during systemic disease or serious illness.
Sebaceous glands are distributed over the entire skin surface except for the palms of the hands and soles of the feet. Most of these glands are connected directly to the hair follicles (Fig. 26-4). The sebaceous glands of the eyelids, nipple areolae, and genitalia are freestanding.
Sebaceous glands produce sebum, a mildly bacteriostatic, fat-containing substance. Sebum lubricates the skin and reduces water loss from the skin surface.
Sweat glands of the skin are of two types: eccrine and apocrine. Eccrine sweat glands arise from the epithelial cells. They are found over the entire skin surface and are not associated with the hair follicle. The odorless, colorless, isotonic secretions of these glands are important in the regulation of body temperature. Stimulation of sweat from these glands and the resultant water evaporation can cause the body to lose as much as 10 to 12 L of fluid in a single day.
Apocrine sweat glands are in direct contact with the hair follicle. They are found mostly in the axillae, nipple areolae, periumbilicus, and perineal body areas. The interaction of skin bacteria with the secretions of the apocrine glands causes the distinctive body odor.
Functions of the Skin
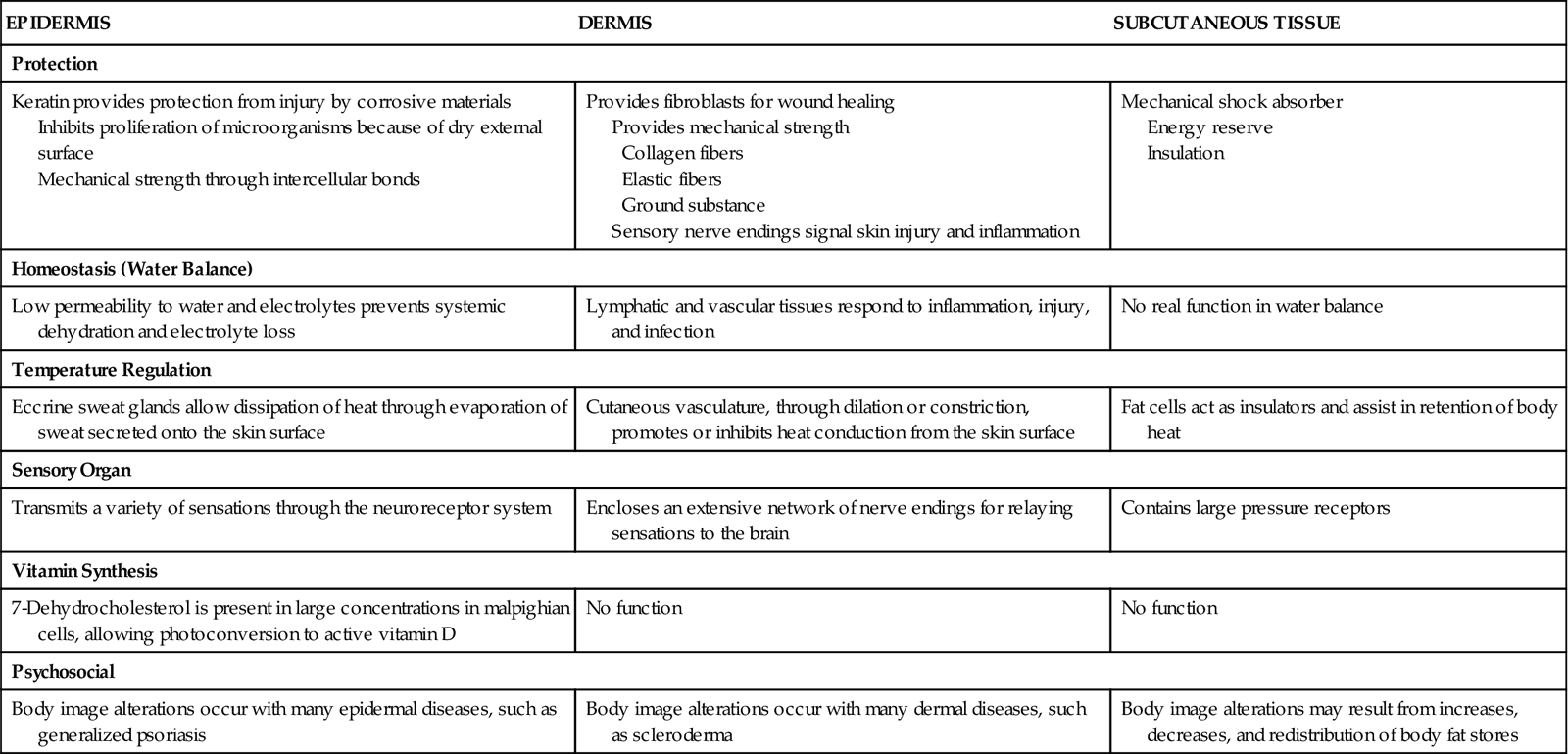
The skin is a complex organ responsible for the regulation of many body functions throughout the life span (Table 26-1) (McCance et al., 2010). In addition to the skin’s protective and regulatory functions, its location on the outside of the body makes it an important way to communicate a patient’s state of health and body image.
TABLE 26-1
| EPIDERMIS | DERMIS | SUBCUTANEOUS TISSUE |
| Protection | ||
| Keratin provides protection from injury by corrosive materials Inhibits proliferation of microorganisms because of dry external surface Mechanical strength through intercellular bonds | Provides fibroblasts for wound healing Provides mechanical strength Collagen fibers Elastic fibers Ground substance Sensory nerve endings signal skin injury and inflammation | Mechanical shock absorber Energy reserve Insulation |
| Homeostasis (Water Balance) | ||
| Low permeability to water and electrolytes prevents systemic dehydration and electrolyte loss | Lymphatic and vascular tissues respond to inflammation, injury, and infection | No real function in water balance |
| Temperature Regulation | ||
| Eccrine sweat glands allow dissipation of heat through evaporation of sweat secreted onto the skin surface | Cutaneous vasculature, through dilation or constriction, promotes or inhibits heat conduction from the skin surface | Fat cells act as insulators and assist in retention of body heat |
| Sensory Organ | ||
| Transmits a variety of sensations through the neuroreceptor system | Encloses an extensive network of nerve endings for relaying sensations to the brain | Contains large pressure receptors |
| Vitamin Synthesis | ||
| 7-Dehydrocholesterol is present in large concentrations in malpighian cells, allowing photoconversion to active vitamin D | No function | No function |
| Psychosocial | ||
| Body image alterations occur with many epidermal diseases, such as generalized psoriasis | Body image alterations occur with many dermal diseases, such as scleroderma | Body image alterations may result from increases, decreases, and redistribution of body fat stores |
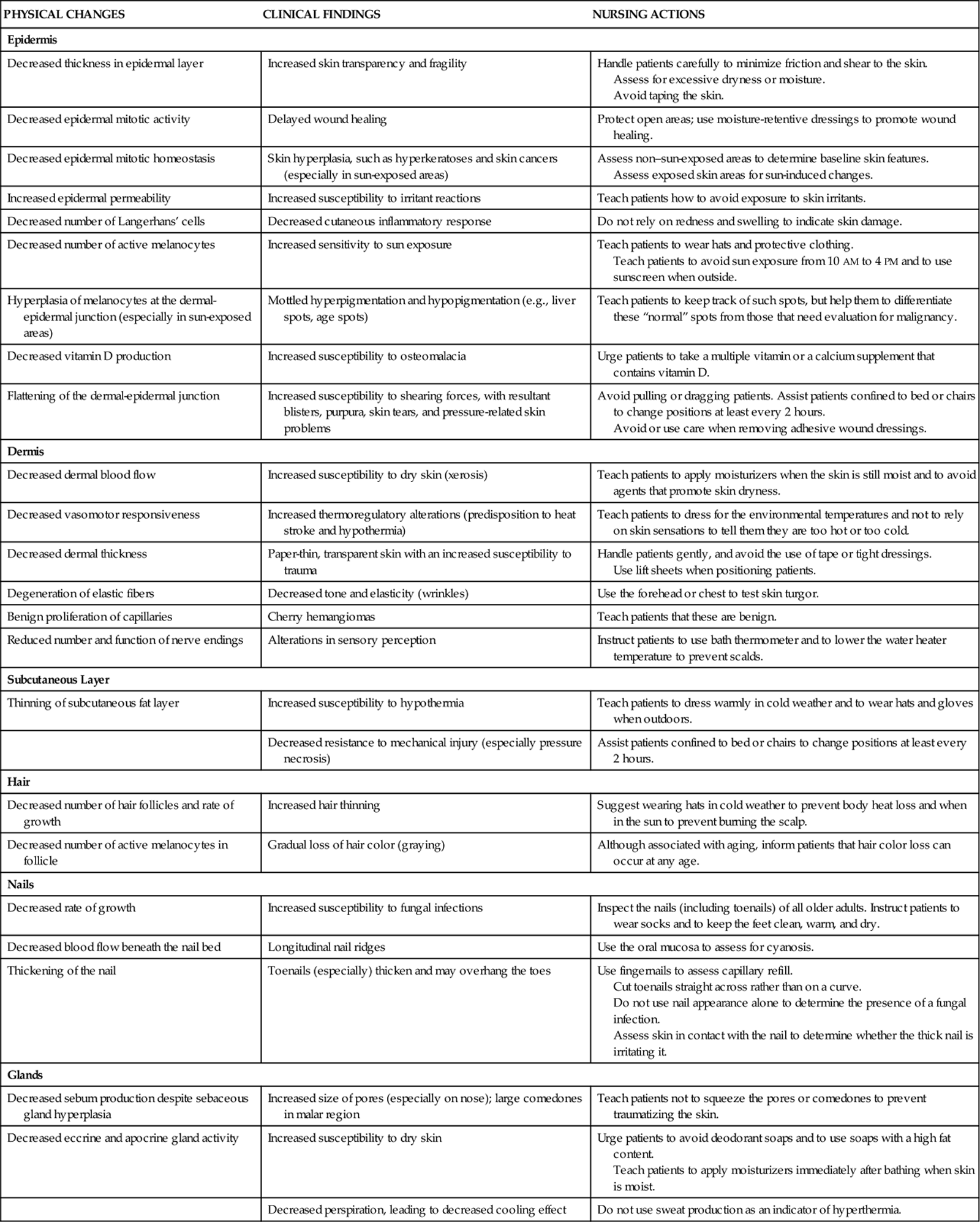
Skin Changes Associated with Aging
The process of aging begins at birth. As changes in physiology progress with aging, the skin also undergoes age-related changes in both structure and function (Chart 26-1). Figs. 26-5 through 26-12 show some common age-related skin changes (Bianchi & Cameron, 2009).




Individual differences exist in how quickly and to what degree the skin ages (Helfrich et al., 2008). Although genetic background, hormonal changes, and systemic disease may change the appearance of the skin over time, chronic sun exposure is the single most important factor leading to degeneration of the skin components.
Assessment Methods
Patient History
Before examining the skin, take an accurate history from the patient so that actual and potential skin problems can be readily identified. Important data to collect include demographic and socioeconomic information. Chart 26-2 highlights specific questions to ask during a skin assessment.
Demographic data include age, race, occupation, and hobbies or recreational activities. This information can help identify causative or aggravating factors for skin problems. Age is important because many changes in the skin, hair, and nails are normal manifestations of the aging process.
Race and nationality can also be important. Some variations in the appearance of skin are normal among patients of specific races and ethnicities but are abnormal for those of other races or ethnicities.
Information about occupation and hobbies can provide clues to chronic skin exposure to chemicals, irritants, abrasive substances, and other environmental factors that can contribute to skin problems. Also, frequent or recent travel to tropical climates may be associated with the development of skin infections or infestations.
Socioeconomic status data can help identify environmental factors that might contribute to skin disease. Recent travel may be a source of skin infections or unusual lesions.
If the patient is well tanned, ask about the amount of time spent in the sun and tanning salons and whether he or she has any skin problems from sun exposure. Use this time to teach the patient about the harmful aspects of sun exposure and how to reduce sun exposure.
Skin problems related to poor hygiene are common. Ask about living conditions, bathing practices, and the availability of running water. Teach people that keeping the skin and hair clean by bathing and shampooing regularly helps maintain the skin’s health.
Information about drug use is important to obtain because prescribed drugs, over-the-counter (OTC) drugs, herbal preparations or remedies, and tobacco use can cause allergies or skin reactions or affect skin function. Ask the patient about any recent use of prescription drugs, OTC drugs (e.g., laxatives, antacids, cold remedies), and herbal preparations or remedies. Determine when each drug was started, the dose and frequency of the drug, and the time the last dose was taken. Ask the patient whether skin changes began after starting a new drug. A drug history also helps identify skin changes that result from the treatment of other health problems, such as the changes that occur with long-term steroid or anticoagulant therapy.
Allergies can develop to environmental substances and often have skin manifestations. These allergies may be well documented or have a new onset. Ask about the use of any new personal care product (e.g., shaving products, perfumes, soap, shampoo, lotion, makeup, hair gel, toothpaste), laundry detergents and softeners, and home cleaning products. Determine whether the patient wears gloves to avoid direct contact with cleaning solutions. New clothing may contain chemicals that come into contact with and irritate the skin. Documenting the body location(s) of the skin problem can help determine its cause.
Nutrition Status
Document the patient’s weight, height, body build and fat distribution, and food preferences. Poor nutrition, especially protein deficiencies, vitamin deficiencies, and obesity, can increase the patient’s risk for skin lesions and delay wound healing. Fat-free diets and chronic alcoholism can lead to vitamin deficiencies and related skin changes. Some skin diseases, such as chronic urticaria and acne, may be worsened by certain foods or food additives.
Hydration influences overall skin health, and the skin reflects hydration status. Reduced fluid intake can lead to dry skin. Skin manifestations of severe fluid losses are seen as loose skin that tents when pinched together. Fluid overload with edema can stretch the skin, masking wrinkles and allowing the formation of skin “pits” when pressure is applied to it.
Family History and Genetic Risk
Many skin problems (e.g., psoriasis, skin cancer, keloid formation, eczema) have a familial predisposition or can be inherited (Nussbaum et al., 2007). Explore any family tendency of chronic skin problems. Ask about immediate family members’ current health status to identify a disease that could be transferred among family members (e.g., ringworm, scabies).
Current Health Problems
Chart 26-2 lists the best practices for obtaining a history from a patient with a skin problem. Begin by gathering information about skin changes and current skin care practices.
If a skin problem is identified, obtain more information about the specific problem, such as:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree