Chapter 26 Assessment of the Skin, Hair, and Nails
Safe and Effective Care Environment
1. Use knowledge of integumentary changes associated with aging to protect older adult patients from skin injury.
2. Modify techniques to assess skin changes in patients with darker skin.
Health Promotion and Maintenance
3. Teach all people how to protect the skin from sun exposure.
4. Teach all people to use the ABCDE method of checking lesions for manifestations of melanoma.
5. Perform health history and risk assessment for skin, hair, and nail problems.
6. Teach patients and family members about what to expect during tests and procedures to assess skin function and skin disease.
7. Reassure patients who have skin changes that are variations of normal.
8. Compare the structures and function of the epidermis, dermis, and subcutaneous tissue.
9. Use proper terminology to communicate skin assessment findings.
10. Distinguish between normal variations and abnormal skin manifestations with regard to skin color, texture, warmth, and moisture.
11. Use the ABCDE method of assessing skin lesions for cancer.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
The integumentary system includes the skin, hair, and nails. The skin plays a major role in the concept of body protection. As shown in Fig. 26-1, the skin protects against foreign invasion by providing a first line of defense (the moat), a second line of defense (the castle wall), and even a third line of defense (the knights and soldiers). The normal flora on the surfaces of skin and mucous membranes repels some of the more harmful microorganisms. Intact skin has barrier functions, alarm functions, and even combat functions. Specialized cells called Langerhans’ cells, present in the skin, engulf foreign substances (antigens) that invade the body when the skin is injured. These cells then alert the immune system to the presence of the invader.
The skin is the largest organ of the body and plays a major role in homeostasis. When intact, it helps regulate body temperature and maintains fluid and electrolyte balance. Changes in the skin can communicate information about a person’s health and well-being (Anderson et al., 2007).
Anatomy and Physiology Review
Structure of the Skin
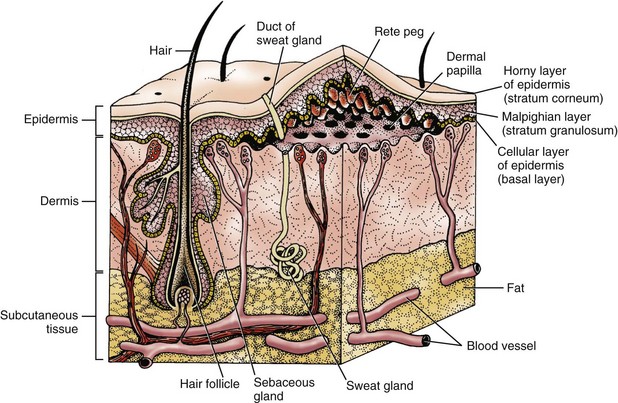
As shown in Fig. 26-2, the skin has three layers: subcutaneous tissue (fat), dermis, and epidermis. Each layer has unique properties that contribute to the skin’s ability to maintain its complex functions.
Structure of the Skin Appendages
Hair follicles are located in the dermal layer of the skin but are actually extensions of the epidermal layer (see Fig. 26-2). Within each hair follicle, a round column of keratin forms the hair shaft. Hair keratin is tougher than skin keratin. Hair color is genetically determined by a person’s rate of melanin production.
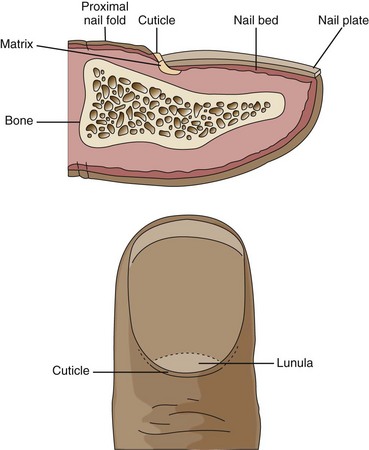
The white, crescent-shaped portion of the nail at the lower end of the nail plate is called the lunula and is the location of the nail matrix, where nail keratin is formed and nail growth begins (Fig. 26-3). Nail growth is a continuous but slow process. Fingernail replacement requires 3 to 4 months. Toenail replacement may take up to 12 months.
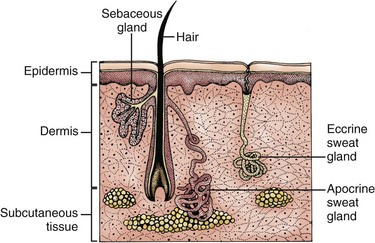
Sebaceous glands are distributed over the entire skin surface except for the palms of the hands and soles of the feet. Most of these glands are connected directly to the hair follicles (Fig. 26-4). The sebaceous glands of the eyelids, nipple areolae, and genitalia are freestanding.
Functions of the Skin
The skin is a complex organ responsible for the regulation of many body functions throughout the life span (Table 26-1) (McCance et al., 2010). In addition to the skin’s protective and regulatory functions, its location on the outside of the body makes it an important way to communicate a patient’s state of health and body image.
TABLE 26-1 FUNCTIONS OF THE SKIN
| EPIDERMIS | DERMIS | SUBCUTANEOUS TISSUE |
|---|---|---|
| Protection | ||
| Keratin provides protection from injury by corrosive materials Inhibits proliferation of microorganisms because of dry external surface Mechanical strength through intercellular bonds | Provides fibroblasts for wound healing Provides mechanical strength Collagen fibers Elastic fibers Ground substance Sensory nerve endings signal skin injury and inflammation | Mechanical shock absorber Energy reserve Insulation |
| Homeostasis (Water Balance) | ||
| Low permeability to water and electrolytes prevents systemic dehydration and electrolyte loss | Lymphatic and vascular tissues respond to inflammation, injury, and infection | No real function in water balance |
| Temperature Regulation | ||
| Eccrine sweat glands allow dissipation of heat through evaporation of sweat secreted onto the skin surface | Cutaneous vasculature, through dilation or constriction, promotes or inhibits heat conduction from the skin surface | Fat cells act as insulators and assist in retention of body heat |
| Sensory Organ | ||
| Transmits a variety of sensations through the neuroreceptor system | Encloses an extensive network of nerve endings for relaying sensations to the brain | Contains large pressure receptors |
| Vitamin Synthesis | ||
| 7-Dehydrocholesterol is present in large concentrations in malpighian cells, allowing photoconversion to active vitamin D | No function | No function |
| Psychosocial | ||
| Body image alterations occur with many epidermal diseases, such as generalized psoriasis | Body image alterations occur with many dermal diseases, such as scleroderma | Body image alterations may result from increases, decreases, and redistribution of body fat stores |
Skin Changes Associated with Aging
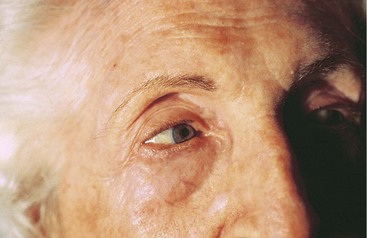
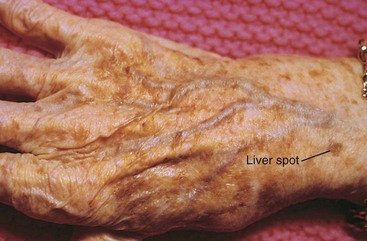
The process of aging begins at birth. As changes in physiology progress with aging, the skin also undergoes age-related changes in both structure and function (Chart 26-1). Figs. 26-5 through 26-12 show some common age-related skin changes (Bianchi & Cameron, 2009).
Chart 26-1 Nursing Focus on the Older Adult
Changes in the Integumentary System Related to Aging
| PHYSICAL CHANGES | CLINICAL FINDINGS | NURSING ACTIONS |
|---|---|---|
| Epidermis | ||
| Decreased thickness in epidermal layer | Increased skin transparency and fragility | Handle patients carefully to minimize friction and shear to the skin. Assess for excessive dryness or moisture. Avoid taping the skin. |
| Decreased epidermal mitotic activity | Delayed wound healing | Protect open areas; use moisture-retentive dressings to promote wound healing. |
| Decreased epidermal mitotic homeostasis | Skin hyperplasia, such as hyperkeratoses and skin cancers (especially in sun-exposed areas) | Assess non–sun-exposed areas to determine baseline skin features. Assess exposed skin areas for sun-induced changes. |
| Increased epidermal permeability | Increased susceptibility to irritant reactions | Teach patients how to avoid exposure to skin irritants. |
| Decreased number of Langerhans’ cells | Decreased cutaneous inflammatory response | Do not rely on redness and swelling to indicate skin damage. |
| Decreased number of active melanocytes | Increased sensitivity to sun exposure | Teach patients to wear hats and protective clothing. Teach patients to avoid sun exposure from 10 AM to 4 PM and to use sunscreen when outside. |
| Hyperplasia of melanocytes at the dermal-epidermal junction (especially in sun-exposed areas) | Mottled hyperpigmentation and hypopigmentation (e.g., liver spots, age spots) | Teach patients to keep track of such spots, but help them to differentiate these “normal” spots from those that need evaluation for malignancy. |
| Decreased vitamin D production | Increased susceptibility to osteomalacia | Urge patients to take a multiple vitamin or a calcium supplement that contains vitamin D. |
| Flattening of the dermal-epidermal junction | Increased susceptibility to shearing forces, with resultant blisters, purpura, skin tears, and pressure-related skin problems | Avoid pulling or dragging patients. Assist patients confined to bed or chairs to change positions at least every 2 hours. Avoid or use care when removing adhesive wound dressings. |
| Dermis | ||
| Decreased dermal blood flow | Increased susceptibility to dry skin (xerosis) | Teach patients to apply moisturizers when the skin is still moist and to avoid agents that promote skin dryness. |
| Decreased vasomotor responsiveness | Increased thermoregulatory alterations (predisposition to heat stroke and hypothermia) | Teach patients to dress for the environmental temperatures and not to rely on skin sensations to tell them they are too hot or too cold. |
| Decreased dermal thickness | Paper-thin, transparent skin with an increased susceptibility to trauma | Handle patients gently, and avoid the use of tape or tight dressings. Use lift sheets when positioning patients. |
| Degeneration of elastic fibers | Decreased tone and elasticity (wrinkles) | Use the forehead or chest to test skin turgor. |
| Benign proliferation of capillaries | Cherry hemangiomas | Teach patients that these are benign. |
| Reduced number and function of nerve endings | Alterations in sensory perception | Instruct patients to use bath thermometer and to lower the water heater temperature to prevent scalds. |
| Subcutaneous Layer | ||
| Thinning of subcutaneous fat layer | Increased susceptibility to hypothermia | Teach patients to dress warmly in cold weather and to wear hats and gloves when outdoors. |
| Decreased resistance to mechanical injury (especially pressure necrosis) | Assist patients confined to bed or chairs to change positions at least every 2 hours. | |
| Hair | ||
| Decreased number of hair follicles and rate of growth | Increased hair thinning | Suggest wearing hats in cold weather to prevent body heat loss and when in the sun to prevent burning the scalp. |
| Decreased number of active melanocytes in follicle | Gradual loss of hair color (graying) | Although associated with aging, inform patients that hair color loss can occur at any age. |
| Nails | ||
| Decreased rate of growth | Increased susceptibility to fungal infections | Inspect the nails (including toenails) of all older adults. Instruct patients to wear socks and to keep the feet clean, warm, and dry. |
| Decreased blood flow beneath the nail bed | Longitudinal nail ridges | Use the oral mucosa to assess for cyanosis. |
| Thickening of the nail | Toenails (especially) thicken and may overhang the toes | Use fingernails to assess capillary refill. Cut toenails straight across rather than on a curve. Do not use nail appearance alone to determine the presence of a fungal infection. Assess skin in contact with the nail to determine whether the thick nail is irritating it. |
| Glands | ||
| Decreased sebum production despite sebaceous gland hyperplasia | Increased size of pores (especially on nose); large comedones in malar region | Teach patients not to squeeze the pores or comedones to prevent traumatizing the skin. |
| Decreased eccrine and apocrine gland activity | Increased susceptibility to dry skin | Urge patients to avoid deodorant soaps and to use soaps with a high fat content. Teach patients to apply moisturizers immediately after bathing when skin is moist. |
| Decreased perspiration, leading to decreased cooling effect | Do not use sweat production as an indicator of hyperthermia. | |
Individual differences exist in how quickly and to what degree the skin ages (Helfrich et al., 2008). Although genetic background, hormonal changes, and systemic disease may change the appearance of the skin over time, chronic sun exposure is the single most important factor leading to degeneration of the skin components.
Physiological Integrity
Assessment Methods
Patient History
Before examining the skin, take an accurate history from the patient so that actual and potential skin problems can be readily identified. Important data to collect include demographic and socioeconomic information. Chart 26-2 highlights specific questions to ask during a skin assessment.
Chart 26-2 Best Practice for Patient Safety & Quality Care
Obtaining an Accurate Nursing History of the Patient with a Skin Problem
Medication History
• Is the patient allergic to any systemic or topical drug? If so, have the patient describe the reaction.
• What prescription drugs has the patient taken recently? When was the drug started? What is the dose or frequency of administration? When was the last dose taken?
• What over-the-counter drugs has the patient taken recently? When was the drug started? What is the dose or frequency of administration? When was the last dose taken?
Social History
• What is the patient’s occupation?
• What recreational activities does the patient enjoy?
• Has the patient traveled recently?
• What is the patient’s nutritional status?
• Does the patient use tobacco or recreational drugs, or drink alcohol?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree