Chapter 72 Assessment of the Reproductive System
Health Promotion and Maintenance
1. Teach patients about recommended guidelines for selected reproductive screening tests.
2. Teach pre- and post-test care for diagnostic testing for the reproductive system.
4. Briefly review the anatomy and physiology of the male and the female reproductive systems.
5. Identify reproductive changes associated with aging and their implications for nursing care.
6. Perform a focused physical assessment of the patient with male or female reproductive system problems.
7. Explain the use of laboratory testing for patients with suspected or actual reproductive health problems.
8. Develop a teaching plan for a patient undergoing endoscopic studies for reproductive health problems.
http://evolve.elsevier.com/Iggy/
Animation: Lymphatic Drainage of the Breast
Animation: The Menstrual Cycle
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Video Clip: Bimanual Examination
Video Clip: External Genitalia
Video Clip: Inguinal Hernia Evaluation
Video Clip: Inspection (Standing)
Video Clip: Speculum Examination
Anatomy and Physiology Review
Structure and Function of the Female Reproductive System
The female reproductive system is located both outside (external) and inside (internal) the body.
Internal Genitalia
The internal female genitalia are shown in Fig. 72-1. The vagina is a hollow tube that extends from the vestibule to the uterus. In addition to being the channel for the passage of the menstrual flow, the vagina allows for insertion of the penis during intercourse and passage of the fetus during a vaginal birth. Reduced estrogen levels occurring during menopause cause the vaginal wall to become dry, thinner, and smoother. The vagina then atrophies and is prone to pathogenic growth, resulting in a variety of types of infections.
Breasts
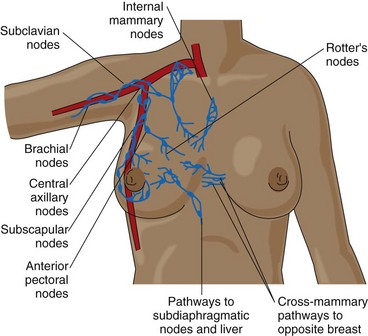
Breast tissue is composed of a network of glandular and ductal tissue, fibrous tissue, and fat. The proportion of each component of breast tissue depends on genetic factors, nutrition, age, and obstetric history. The breasts are supported by ligaments that are attached to underlying muscles. They have abundant blood supply and lymph flow that drains from an extensive network toward the axilla (Fig. 72-2).
Structure and Function of the Male Reproductive System
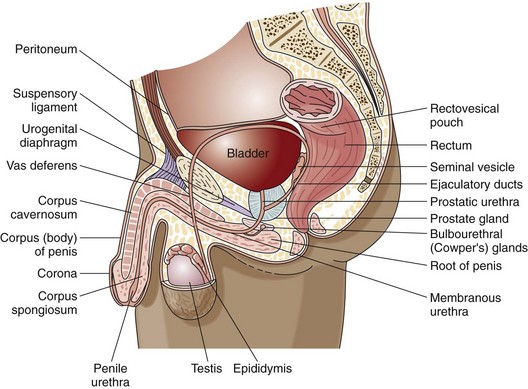
The internal male genitalia are shown in Fig. 72-3. The major organs are the testes and prostate gland. The testes are a pair of oval organs in the scrotum that produce sperm and testosterone. Each testis is suspended in the scrotum by the spermatic cord, which provides blood, lymphatic, and nerve supply to the testis. Sympathetic nerve fibers are located on the arteries in the cord, and sympathetic and parasympathetic fibers are on the vas deferens. When the testes are damaged, these autonomic nerve fibers transmit excruciating pain and a sensation of nausea.
Reproductive Changes Associated with Aging
Age affects the function of both the male and the female reproductive systems. Many changes in the reproductive system occur as people age (Chart 72-1).
Chart 72-1 Nursing Focus on the Older Adult
Changes in the Reproductive System Related to Aging
| PHYSIOLOGIC CHANGE | NURSING INTERVENTIONS | RATIONALES |
|---|---|---|
| Women | ||
| Graying and thinning of the pubic hairDecreased size of the labia majora and clitoris | Discuss changes with the patient (applies to all structures for both women and men). | Education helps prevent problems with body image (applies to all structures for both women and men). |
| Drying, smoothing, and thinning of the vaginal walls | Provide information about vaginal estrogen therapy and water-soluble lubricants. | Education enables the patient to make informed decisions about the treatment of vaginal dryness, which can cause painful intercourse. |
| Decreased size of the uterusAtrophy of the endometriumDecreased size and marked convolution of the ovariesLoss of tone and elasticity of the pelvic ligaments and connective tissue | Provide information about Kegel exercises to strengthen pelvic muscles. Urinary incontinence can be a major problem. | Strengthening exercises may prevent or reduce pelvic relaxation and urinary incontinence. |
| Increased flabbiness and fibrosis of the breasts, which hang lower on the chest wall; decreased erection of the nipples | Teach or reinforce the importance of breast self-awareness, clinical breast examinations, and mammography. | These methods can detect masses or other changes that may indicate the presence of cancer. |
| Men | ||
| Graying and thinning of the pubic hair | Teach or reinforce the importance of testicular self-examination (TSE). | TSE may detect changes that may indicate cancer. |
| Increased drooping of the scrotum and loss of rugae | ||
| Prostate enlargement, with an increased likelihood of urethral obstruction | Teach the patient the signs of urethral obstruction and the importance of prostate cancer screening. | Education helps the patient detect enlargement or obstruction, which may indicate the presence of cancer. |
Assessment Methods
Patient History
Establish a trusting relationship with the patient. Many patients are hesitant to share their reproductive history or concerns about sexuality. Respect their choice to refuse to answer questions and talk about their reproductive problems or sexual practices. Chart 72-2 describes questions to consider when assessing the patient’s sexuality and reproductive health using Gordon’s Functional Health Patterns.
Reproductive Assessment
Using Gordon’s Functional Health Patterns
Health Perception/Health Management Pattern
• Has anyone in your family had cancer of the breast or reproductive organs? Who and what type of cancer?
• If you engage in sexual activities, do you practice “safer” sex?
• What do you do to keep healthy—regular health checkups, self-examination (breast, genital [vulvar, testicular]), healthy diet, exercise, use of medications or alternative therapies?
Sexuality-Reproductive Pattern
Male and Female
• Are you sexually active? Do you find your sexual relationship satisfying? Have there been any changes in your relationship? Are you having any problems in your sexual relationship?
• Do you use contraceptives? If so, do you have any problems with the method of contraception?
• Have you had any sexually transmitted diseases? If yes, when and what type did you have?
Based on Gordon, M. (2011). Manual of nursing diagnosis (12th ed.). New York: Jones & Bartlett.
Data about sexual activity are important to obtain as part of the history. Heterosexual activity should not be assumed. Lesbian, gay, bisexual, and transgender (LGBT) issues are often not assessed by health care professionals or shared by the patient. Table 4-3 in Chapter 4 suggests sensitive ways to ask questions about sexual activity.
Nutrition History
A nutrition history is often critical for an accurate assessment of reproductive system problems. For example, fatigue and low libido may occur with poor diet and anemia. Obesity raises the risk for uterine cancer. High-fat diets may increase the risk for cancer of the breast, ovary, and prostate gland (American Cancer Society [ACS], 2010). Ask the patient to recall his or her dietary intake for a recent 24-hour period to assess quality.
Women have special nutrition needs. Those who use oral contraceptives need increased sources of folic acid and vitamins B6, B12, and C. Heavy menstrual bleeding, particularly in women who have intrauterine devices, may require oral iron supplements. Teach all women of any age about their body’s need for calcium. Although adequate calcium intake throughout life is needed, it is especially important during and after menopause to help prevent osteoporosis due to decreased estrogen production (see Chapter 53).
Family History and Genetic Risk
Specific BRCA1 and BRCA2 gene mutations increase the overall risk for breast or ovarian cancer (ACS, 2010). Men with first-degree relatives (e.g., father, brother) with prostate cancer are at greater risk for the disease than men in the general population. Testicular cancer can also be familial (ACS, 2010). More information about genetic risks is discussed with specific health problems in later chapters of this unit.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



 inch (1 cm) into the rectal lumen.
inch (1 cm) into the rectal lumen.