Rachel L. Palmieri
Assessment of the Nervous System
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
5 Briefly review the anatomy and physiology of the nervous system.
6 Describe common physiologic changes associated with aging that affect the nervous system.
7 Interpret findings from a comprehensive neurologic physical assessment.
8 Identify how to perform a rapid neurologic assessment and interpret findings.
9 Assess patients for complications of neurologic diagnostic tests.

http://evolve.elsevier.com/Iggy/
Animation: Cranial Nerves
Animation: Motor Pathways and Clinical Evaluation of the CNS
Animation: Physiology of the Brain
Animation: Reflex Arc
Animation: Sensory Pathways and Clinical Evaluation of the CNS
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Key Points
Review Questions for the NCLEX® Examination
Video Clip: Central Vision
Video Clip: Deep Tendon Reflex
Video Clip: Fine Motor Coordination
Video Clip: Light Touch
Video Clip: Pupil Responses
Video Clip: Sensory Evaluation
Video Clip: Smell
The nervous system controls mobility, sensation, and cognition. In addition, through the autonomic nervous system (ANS), it innervates many other body systems to make them function. For example, the sacral spinal nerves (part of the ANS) stimulate the detrusor muscle to contract when the urinary bladder is full.
Health problems involving trauma and diseases of the brain can impair the human needs for mobility, sensation, and/or cognition. When the spine or peripheral nervous system is affected, mobility and/or sensation is often impaired. The primary role of the nurse is to help restore these human needs or to assist the patient to adapt to their deficits.
Anatomy and Physiology Review
The major divisions of the nervous system are the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS is composed of the brain and the spinal cord. The brain is contained within the cranium; the brain’s role is to direct the regulation and function of the nervous system and other systems of the body. The spinal cord is lodged in the vertebral canal. From the brain, the spinal cord descends down the middle of the back and is surrounded and protected by the boney vertebral column. The spinal cord is surrounded by a clear fluid called cerebrospinal fluid (CSF) that protects the delicate nerve tissues against damage from banging against the inside of the vertebrae.
The PNS is composed of 12 pairs of cranial nerves, 31 pairs of spinal nerves, and the autonomic nervous system. The autonomic nervous system is further subdivided into sympathetic and parasympathetic fibers.
The nervous system contains two types of cells: neurons, which transmit or conduct nerve impulses; and neuroglial cells, which have an interdependent role with the neuron.
Nervous System Cells: Structure and Function
Neurons
The basic unit of the nervous system, the neuron, transmits impulses, or “messages.” Some neurons are motor (causing movement or mobility), and some are sensory (causing sensation). Some process information, and some retain information. When a neuron receives an impulse from another neuron, the effect may be excitation or inhibition. Each neuron has a cell body, or soma; short, branching processes called dendrites; and a single axon (Fig. 43-1).
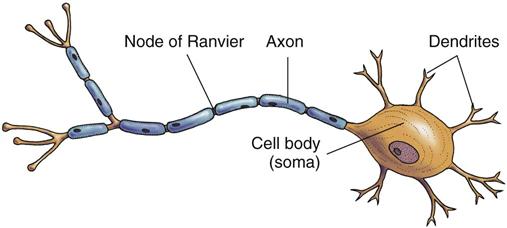
Afferent neurons, also known as sensory neurons, are specialized to send impulses toward the CNS, away from the PNS. Efferent neurons are motor nerve cells that carry signals from the CNS to the cells in the PNS. Each dendrite synapses with another cell body, axon, or dendrite and sends impulses along the efferent and afferent neuron pathways.
Many axons are covered by a myelin sheath—a white, lipid covering. Myelinated axons appear whitish and therefore are also called white matter. Nonmyelinated axons have a grayish cast and are called gray matter. Myelinated axons have gaps in the myelin called nodes of Ranvier. The nodes of Ranvier play a major role in impulse conduction (see Fig. 43-1). When the myelin is impaired, the impulses cannot travel from the brain to the rest of the body, such as in patients with multiple sclerosis.
The enlarged, distal end of each axon is called the synaptic or terminal knob. Within the synaptic knobs are the mechanisms for manufacturing, storing, and releasing a transmitter substance. Each neuron produces a specific neurotransmitter chemical (e.g., acetylcholine or serotonin) that can either enhance or inhibit the impulse but cannot do both. Other substances, although not specifically identified as neurotransmitters, are considered probable transmitters or neuromodulators.
Impulses are transmitted to their eventual destination through synapses, or spaces between neurons. There are two distinct types of synapses: neuron to neuron and neuron to muscle (or gland). Between the terminal knob and the next cell is a small space called the synaptic cleft. The knob, the cleft, and the portion of the cell to which the impulse is being transmitted make up the synapse.
Neuroglial Cells
Neuroglial cells, which vary in size and shape, provide protection, structure, and nutrition for the neurons. They are classified into four types: astroglial cells, ependymal cells, oligodendrocytes, and microglial cells. These cells are also part of the blood-brain barrier and help regulate cerebrospinal fluid (CSF).
Central Nervous System: Structure and Function
The central nervous system (CNS) is composed of the brain, which directs the regulation and function of the nervous system and all other systems of the body, and the spinal cord, which starts reflex activity and transmits impulses to and from the brain.
Brain
The meninges form the protective covering of the brain and the spinal cord. The outside layer is the dura mater. The subdural space is located between the dura mater and the middle layer, the arachnoid. The pia mater is the most inner layer. Situated between the arachnoid and pia mater is the subarachnoid space, where CSF circulates. A potential space, referred to as the epidural space, is located between the skull and the outer layer of the dura mater. This area also extends down the spinal cord and is used for the delivery of epidural analgesia and anesthesia.
The dura mater also lies between the cerebral hemispheres and the cerebellum and is called the tentorium. It helps decrease or prevent the transmission of force from one hemisphere to another and protect the lower brainstem when head trauma occurs. Clinical references may be made to a lesion (e.g., a tumor) as being supratentorial (above the tentorium) or infratentorial (below the tentorium).
Major Parts of the Brain.
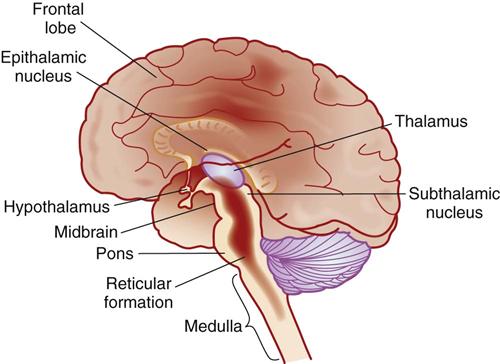
The brain consists of three main areas—the brainstem, the cerebellum, and the forebrain. The brainstem connects the rest of the brain with the CNS. It is concerned primarily with life support and basic functions such as movement.
The cerebellum is concerned with coordination of movement and works together with the brainstem to focus on the functionality of the muscles. This structure is found below the occipital lobe and adjacent to the brainstem.
The forebrain lies above the brainstem and cerebellum and is the most advanced in evolution. This area of the brain is further divided into three areas—the diencephalon, the cerebrum, and the cerebral cortex.
The diencephalon, which lies below the cerebrum, includes the thalamus, hypothalamus, and epithalamus (Fig. 43-2). The thalamus is the major “relay station,” or “central switchboard,” for the CNS. The hypothalamus plays a major role in autonomic nervous system control (controlling temperature and other functions) and intellectual function (cognition). The epithalamus contains the roof of the third ventricle and the pineal gland.
The cerebrum is the largest part of the brain and controls intelligence, creativity, and memory. The “gray matter” of the cerebrum is the central cortex—the center that receives information from the thalamus and all the lower areas of the brain. The cerebrum consists of two halves, referred to as the right hemisphere and the left hemisphere, which are joined by the corpus callosum. The left hemisphere is the dominant hemisphere in most people (even in many left-handed people). Within the deeper structures of the cerebrum are the right and left lateral ventricles. At the base of the cerebrum near the ventricles is a group of neurons called the basal ganglia, which help regulate the need for mobility.
The cerebral cortex is part of the cerebrum and is involved with almost all of the higher functions of the brain. This part of the brain processes and communicates all information coming from the peripheral nervous system (PNS). It also translates the impulses into understandable feelings and thoughts. The cerebral cortex is so complex that it is further divided into four lobes—the frontal lobe, parietal lobe, temporal lobe, and occipital lobe.
The frontal lobe is found at the front of the head near the temples and forehead. It processes voluntary muscle movements and higher functioning actions such as thought and speech. It also helps control mood, planning for the future, setting goals, and making judgments. The parietal lobe is found behind the frontal lobe. It processes spatial awareness and receives and processes information about temperature, taste, touch, and movement coming from the rest of the body. Reading and arithmetic are also processed in this lobe. The temporal lobes are located in the area of the brain parallel to the ears. They process hearing, memory, and language functions. The occipital lobe is located in the posterior of the brain and assists in the processing of visual information.
Located in the frontal lobe, the motor cortex controls voluntary movement. Corticospinal tracts, also called pyramidal tracts, begin in the motor cortex and travel through the brain before crossing in the medulla. This crossing explains how right motor cortex damage affects the movement in the left side of the body and vice versa, such as in many patients who have cerebral strokes. The cerebrum is divided into lobes by sulci (fissures). These lobes work together and are connected by nerve fibers. The name and main function of each lobe is listed in Table 43-1.
TABLE 43-1
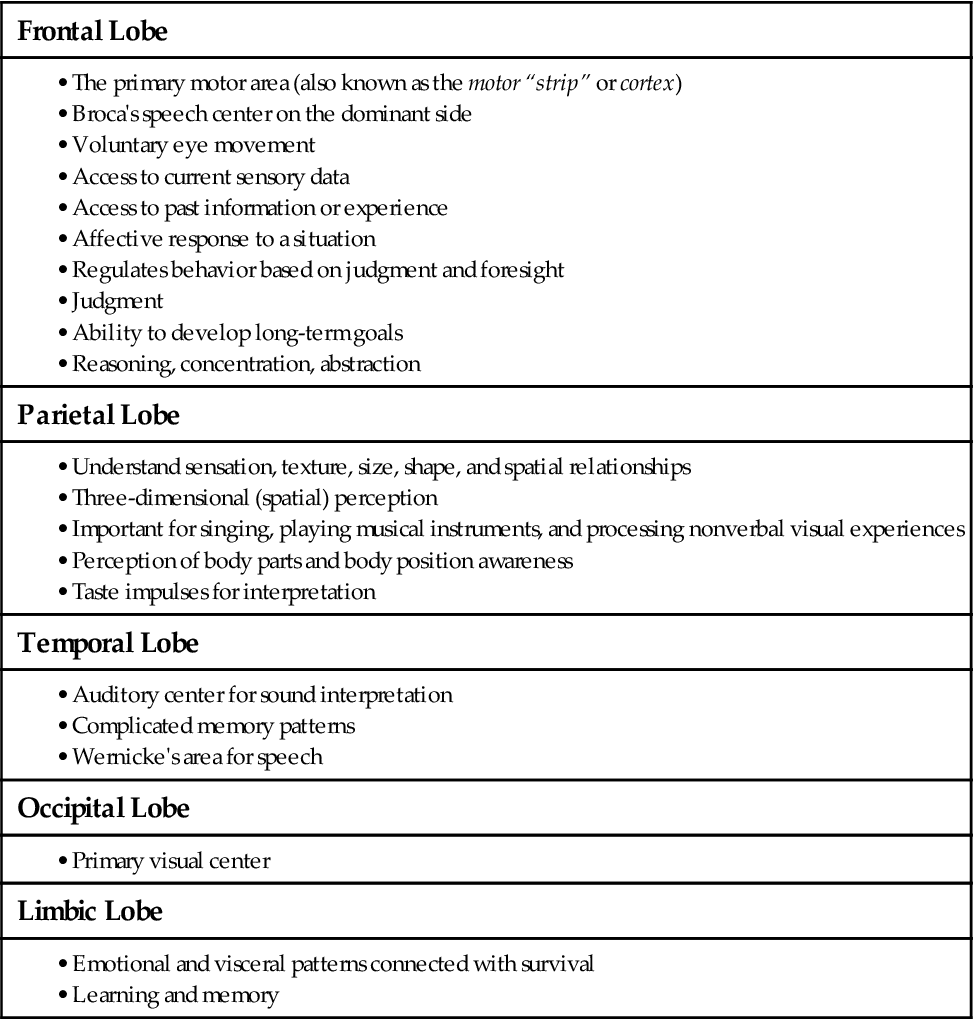
Two important speech areas of the cerebrum are Broca’s area and Wernicke’s area. Broca’s area (speech area), also located in the frontal lobe, is responsible for the formation of words, or speech. Wernicke’s area (language area) is located in the temporal lobe and allows processing of words into coherent thought and understanding of written or spoken words.
The hypophysis (pituitary gland) has two lobes, each releasing specific hormones into the circulation under the regulation of the hypothalamus. The pituitary is often referred to as the “master gland” because of its control of numerous hormonal functions. However, the hypothalamus actually controls its functions.
The cerebellum receives immediate and continuous information about the condition of the muscles, joints, and tendons. Cerebellar function enables a person to:
• Keep an extremity from overshooting an intended target
• Move from one skilled movement to another in an orderly sequence
• Predict distance or gauge the speed with which one is approaching an object
Unlike the motor cortex, cerebellar control of the body is ipsilateral (situated on the same side). The right side of the cerebellum controls the right side of the body, and the left cerebellum controls the left side of the body.
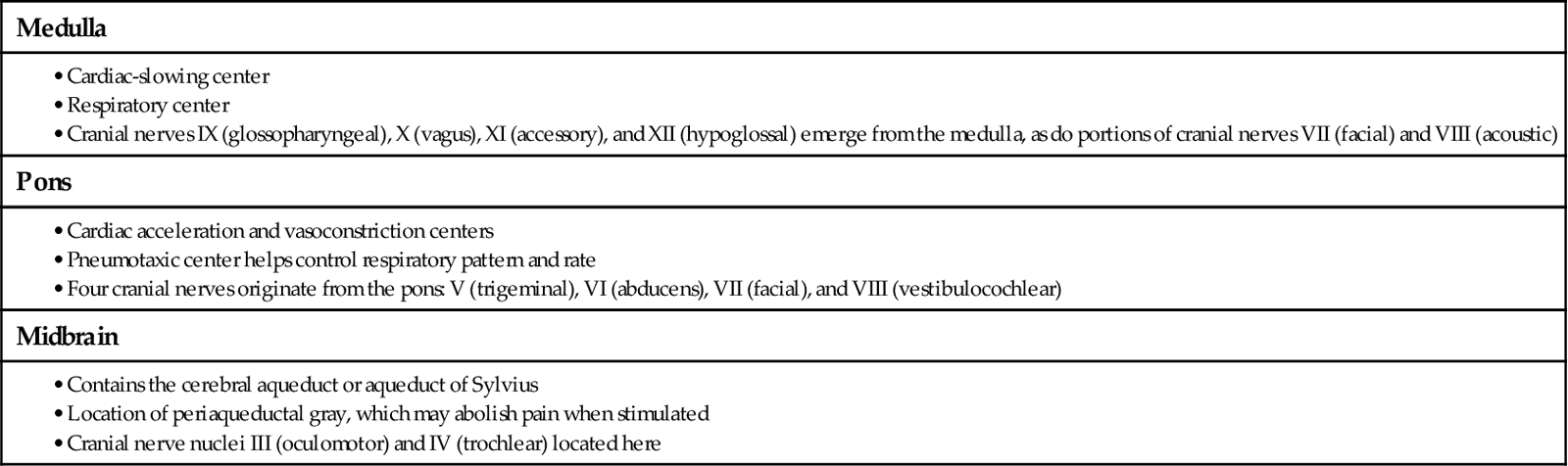
The brainstem includes the midbrain, pons, and medulla. The functions of these structures are presented in Table 43-2. Throughout the brainstem are special cells that constitute the reticular activating system (RAS), which controls awareness and alertness. For example, this tissue awakens a person from sleep when presented with a stimulus such as loud noise or pain or when it is time to awaken. The reticular formation area has many connections with the cerebrum, the rest of the brainstem, and the cerebellum.
Circulation in the Brain.
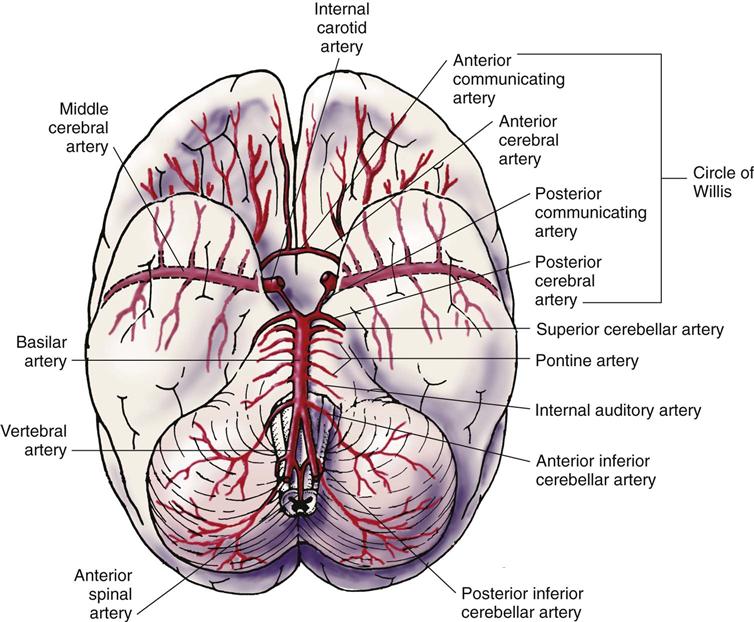
Circulation in the brain originates from the carotid and vertebral arteries (Fig. 43-3). The internal carotid arteries branch into the anterior cerebral artery (ACA) and middle cerebral arteries (MCA), the largest ones. The two posterior vertebral arteries become the basilar artery, which then divides into two posterior cerebral arteries. The anterior, middle, and posterior cerebral arteries are joined together by small communicating arteries to form a ring at the base of the brain known as the circle of Willis.
The middle cerebral artery supplies the lateral surface of the cerebrum from about the mid-temporal lobe upward (i.e., the area for hearing and upper body motor and sensory neurons). The anterior cerebral artery supplies the midline, or medial, aspect of the same area (i.e., the lower body motor and sensory neurons). The posterior cerebral arteries supply the area from the mid-temporal region down and back (occipital lobe), as well as much of the brainstem. When blood flow is interrupted in any of these arteries (e.g., by a clot), the area of the brain being supplied is affected and may not function as it should.
The blood-brain barrier (BBB) seems to exist because the endothelial cells of the cerebral capillaries are joined tightly together. This barrier keeps some substances in the bloodstream out of the cerebrospinal circulation and out of brain tissue. Substances that can pass through the BBB include oxygen, glucose, carbon dioxide, alcohol, anesthetics, and water. Large molecules such as albumin, any substance bound to albumin, and many antibiotics are prevented from crossing the barrier.
Cerebrospinal fluid (CSF) also circulates, surrounds, and cushions the brain and spinal cord. While moving through the subarachnoid space, the fluid is continuously produced by the choroid plexus, reabsorbed by the arachnoid villi, and then channeled into the superior sagittal sinus. Expanded areas of subarachnoid space, where there are large amounts of CSF, are called cisterns. The largest one is the lumbar cistern, the site of lumbar puncture, from the level of the second lumbar vertebra to the second sacral vertebra (L2-S2).
Spinal Cord
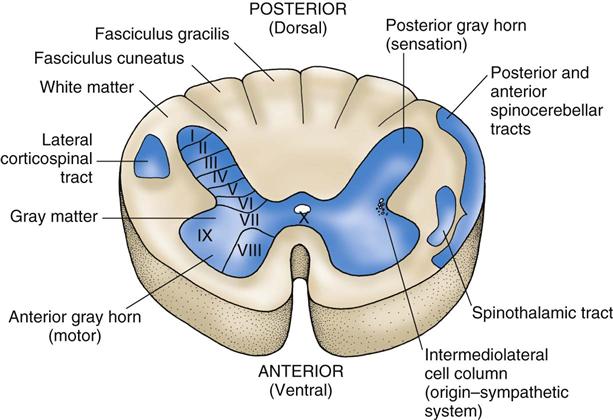
The spinal cord controls body movement (mobility); regulates organ function; processes sensory information from the extremities, trunk, and many internal organs (sensation); and transmits information to and from the brain. It contains H-shaped gray matter (neuron cell bodies) that is surrounded by white matter (myelinated axons). The white matter is divided into posterior, lateral, and anterior columns. Groups of cells in the white matter (ascending and descending tracts) have been fairly well identified (Fig. 43-4).
Ascending Tracts.
Ascending tracts originate in the spinal cord and end in the brain. Three groups of ascending tracts are important for understanding the patient with neurologic problems: spinothalamic tracts, spinocerebellar tracts, and fasciculi gracilis and cuneatus (posterior white columns).
As the name indicates, spinothalamic tracts begin in the spinal cord with most ending in the thalamus. These tracts carry sensations of pain, temperature, light touch, and pressure. The axon fibers from the cells cross to the opposite side and then continue up to the thalamus. Some branches end in the medulla and pons.
Spinocerebellar tracts begin in the spinal cord and end in the cerebellum. The posterior spinocerebellar tract transmits impulses of proprioception (awareness of position and movements of body parts) or movement, mostly from the lower extremities. The impulses enter the posterior gray horn and synapse with tract cells in lamina VII. Spinocerebellar axons then form the tract on the same, or ipsilateral, side. This tract begins at the second lumbar level and ascends to the medulla and then to the cerebellum.
The anterior spinocerebellar tract begins lower in the lumbar spine than does the posterior tract. These fibers cross immediately and ascend as an opposite-side tract, transmitting proprioceptive impulses from the lower extremities. The fibers cross again in the midbrain on their way to the cerebellum. Because these fibers have crossed the midline twice, the sensations end on the side on which they started.
The posterior white columns transmit this information to the thalamus:
Most of the fibers ascend on the same side as their origin to the medulla, where they cross and then synapse in the thalamus, with termination in the parietal lobe. This tract allows a person to feel an exact point of pressure on the skin. Recognition of pressure includes the shape of an object (with eyes closed), movement across the skin (a number being written), and awareness of two points of touch close together (two-point discrimination).
Descending Tracts.
Descending tracts begin in the brain and end in the spinal cord. The major descending tract of importance for understanding neurologic problems is the lateral corticospinal, or pyramidal, tract. The corticospinal tract originates in the motor cortex of the frontal lobe and portions of the parietal lobe. The lateral tract fibers cross to the opposite side at the level of the medulla. After crossing, the fibers descend and synapse with interneurons of the gray matter in the spinal cord. These few fibers connect directly with lower motor neurons (LMNs). The cervical spine has a high concentration of fibers synapsing with interneurons, which possibly reflects the complexity of hand and finger movements.
The motor neurons of the other descending tracts and the basal ganglia used to be referred to as an extrapyramidal system. It was thought that pyramidal neurons caused voluntary muscle activity and that extrapyramidal neurons caused automatic or involuntary muscle action. However, all of the descending tracts and the basal ganglia are necessary for mobility. The term extrapyramidal is still often used clinically, meaning abnormal spontaneous movement.
Peripheral Nervous System: Structure and Function
The peripheral nervous system (PNS) is composed of the spinal nerves, cranial nerves, and autonomic nervous system.
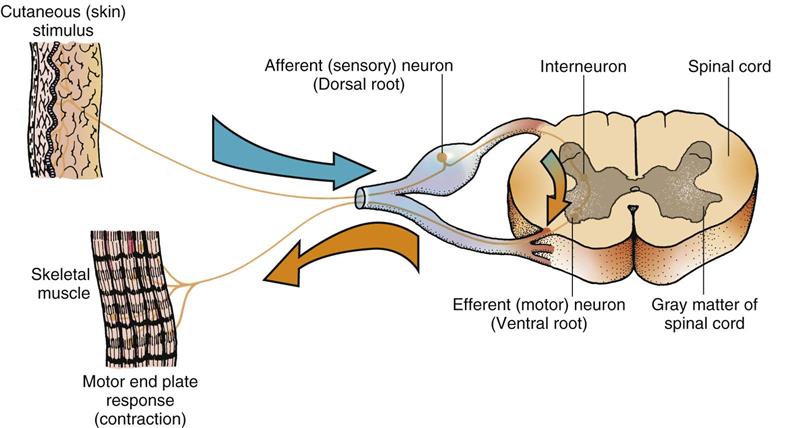
There are 31 pairs of spinal nerves (8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal) exiting from the spinal cord. Each of the nerves has a posterior and an anterior branch. The posterior branch carries sensory information (sensation) to the cord (afferent pathway). The anterior branch transmits motor impulses (mobility) to the muscles of the body (efferent pathway).
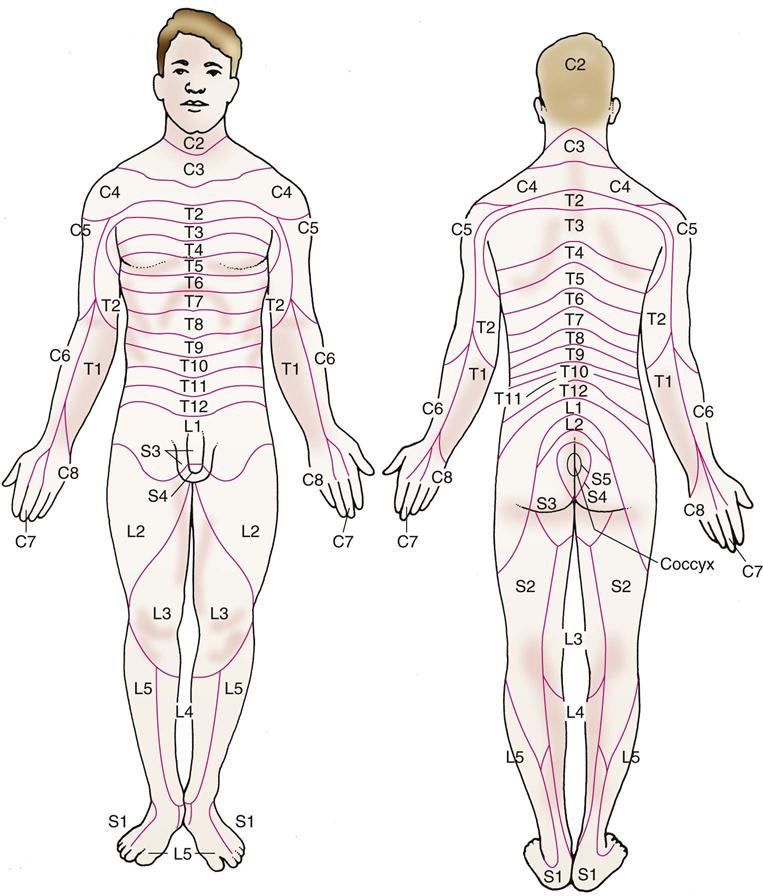
Each spinal nerve is responsible for the muscle innervation and sensory reception of a given area of the body. The cervical and thoracic spinal nerves are relatively close to their areas of responsibility, whereas the lumbar and sacral spinal nerves are some distance from theirs. Because the spinal cord ends between L1 and L2, the axons of the lumbar and sacral cord extend downward before exiting at the appropriate intervertebral foramen. The area controlled by each spinal nerve is roughly reflected in the dermatomes. Dermatomes represent sensory input from spinal nerves to specific areas of the skin (Fig. 43-5). For example, the patient with an injury to cervical spinal nerves C6 and C7 has sensory changes in the thumb, index finger, middle finger, middle of the palm, and back of the hand.
Sensory receptors throughout the body monitor and transmit impulses of pain, temperature, touch, vibration, pressure, visceral sensation, and proprioception. Sensory receptors also monitor and transmit the sensations of the special senses—vision, taste, smell, and hearing.
The cell bodies of the anterior spinal nerves are located in the anterior gray matter (anterior horn) of each level in the spinal cord. The anterior motor neurons are also referred to as lower motor neurons. As each nerve axon leaves the spinal cord, it joins other spinal nerves to form plexuses (clusters of nerves). Plexuses continue as trunks, divisions, and cords and finally branch into individual peripheral nerves.
The reflex arc is a closed circuit of spinal and peripheral nerves and therefore requires no control by the brain (Fig. 43-6).
Reflexes consist of sensory input from:
• Skeletal muscles, tendons, skin, organs, and special senses
• Small cells in the spinal cord lying between the posterior and anterior gray matter (interneurons)
• Anterior motor neurons, along with the muscles they innervate
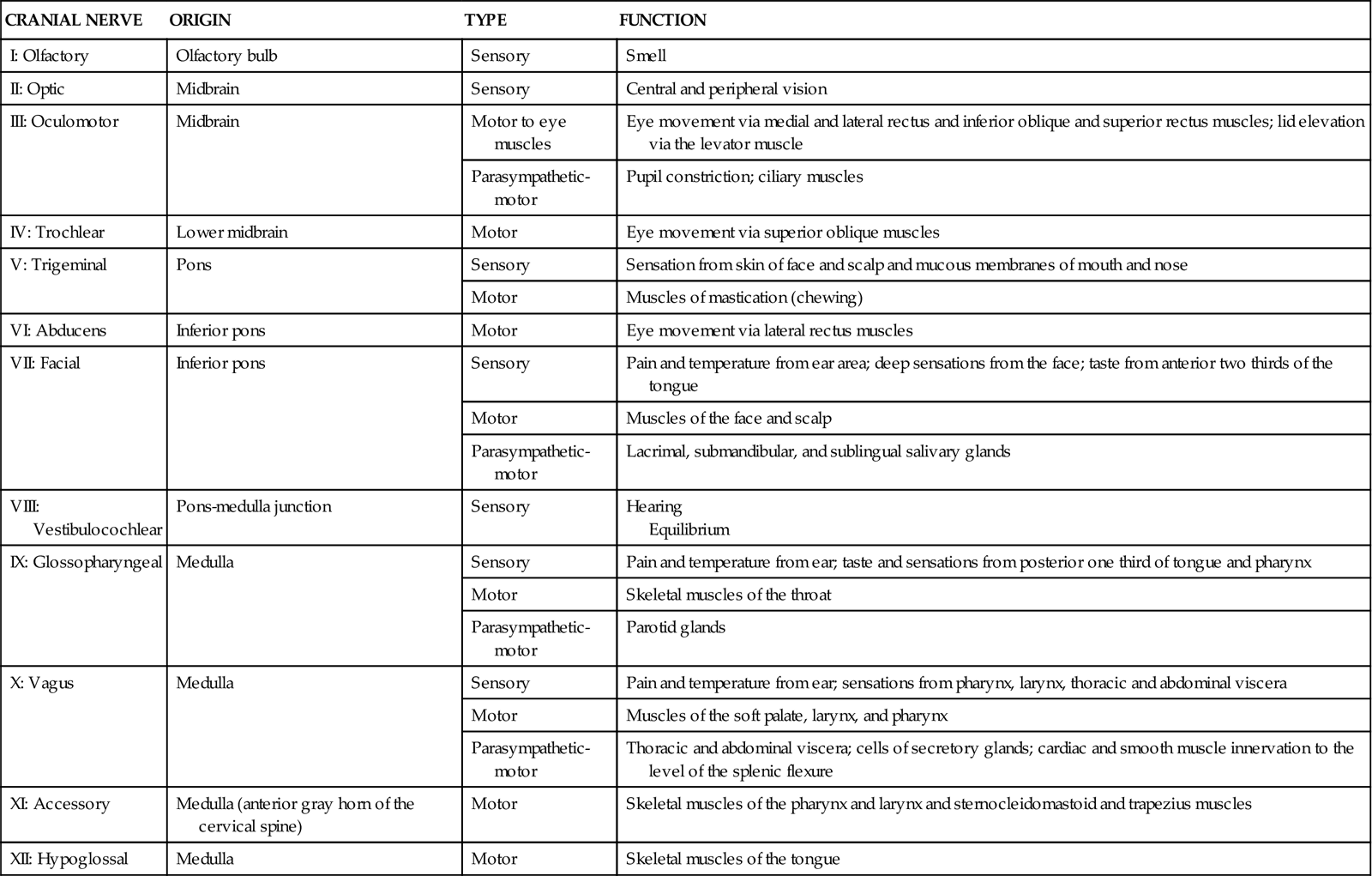
There are 12 cranial nerves. Their name, number, origin, type, and function are summarized in Table 43-3. Cranial nerve function is an important part of the nursing assessment of the patient with a neurologic problem. For example, cranial nerves II, III, IV, and VI are important for assessment of the patient with a stroke.
TABLE 43-3
ORIGINS, TYPES, AND FUNCTIONS OF THE CRANIAL NERVES
| CRANIAL NERVE | ORIGIN | TYPE | FUNCTION |
| I: Olfactory | Olfactory bulb | Sensory | Smell |
| II: Optic | Midbrain | Sensory | Central and peripheral vision |
| III: Oculomotor | Midbrain | Motor to eye muscles | Eye movement via medial and lateral rectus and inferior oblique and superior rectus muscles; lid elevation via the levator muscle |
| Parasympathetic-motor | Pupil constriction; ciliary muscles | ||
| IV: Trochlear | Lower midbrain | Motor | Eye movement via superior oblique muscles |
| V: Trigeminal | Pons | Sensory | Sensation from skin of face and scalp and mucous membranes of mouth and nose |
| Motor | Muscles of mastication (chewing) | ||
| VI: Abducens | Inferior pons | Motor | Eye movement via lateral rectus muscles |
| VII: Facial | Inferior pons | Sensory | Pain and temperature from ear area; deep sensations from the face; taste from anterior two thirds of the tongue |
| Motor | Muscles of the face and scalp | ||
| Parasympathetic-motor | Lacrimal, submandibular, and sublingual salivary glands | ||
| VIII: Vestibulocochlear | Pons-medulla junction | Sensory | Hearing Equilibrium |
| IX: Glossopharyngeal | Medulla | Sensory | Pain and temperature from ear; taste and sensations from posterior one third of tongue and pharynx |
| Motor | Skeletal muscles of the throat | ||
| Parasympathetic-motor | Parotid glands | ||
| X: Vagus | Medulla | Sensory | Pain and temperature from ear; sensations from pharynx, larynx, thoracic and abdominal viscera |
| Motor | Muscles of the soft palate, larynx, and pharynx | ||
| Parasympathetic-motor | Thoracic and abdominal viscera; cells of secretory glands; cardiac and smooth muscle innervation to the level of the splenic flexure | ||
| XI: Accessory | Medulla (anterior gray horn of the cervical spine) | Motor | Skeletal muscles of the pharynx and larynx and sternocleidomastoid and trapezius muscles |
| XII: Hypoglossal | Medulla | Motor | Skeletal muscles of the tongue |
Autonomic Nervous System: Structure and Function
The autonomic nervous system (ANS) is composed of two parts: the sympathetic nervous system (SNS), or the “fight or flight system”; and the parasympathetic nervous system. ANS functions are not usually under conscious control but may be altered in some people by using biofeedback and other methods.
The SNS cells originate in the gray matter of the spinal cord from T1 through L2 or L3. This part of the ANS is considered thoracolumbar because of its anatomic location. The SNS stimulates the functions of the body needed for “fight or flight” (e.g., heart and respiratory rate). It also inhibits those functions not needed in this situation.
The parasympathetic cells originate in the gray matter of the sacral area of the spinal cord (from S2 through S4) plus portions of cranial nerves III, VII, IX, and X (craniosacral). The parasympathetic nervous system can slow body functions when needed.
Parasympathetic fibers to the organs have some sensory ability in addition to motor function. Sensations of irritation, stretching of an organ, or a decrease in tissue oxygen are transmitted to the thalamus through pathways not yet fully understood. Because pain from internal organs is often felt below the body wall innervated by the spinal nerve, it is presumed that there are connections between the viscera and body structure that relay pain sensations.
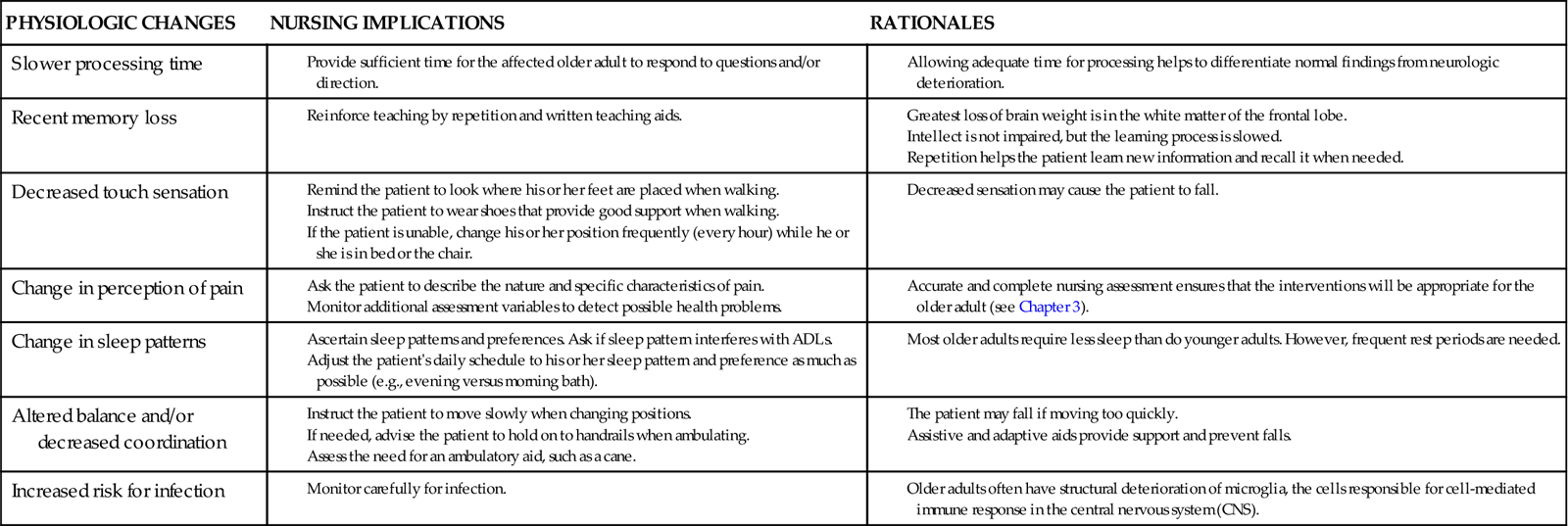
Neurologic Changes Associated with Aging
Neurologic changes associated with aging often affect mobility and sensation. Motor changes in late adulthood can cause slower movement and response time and decreased sensation (Chart 43-1). Any problems that affect the nerves, bones, muscles, or joints also affect motor and therefore ADL ability.
Sensory changes in older adults can also affect their daily activities. Pupils decrease in size, which restricts the amount of light entering the eye, and adapt more slowly. Older adults need increased lighting to see. Touch sensation decreases, which may lead to falls because the older person may not feel small objects or a step underfoot. Vibration sense may be lost in the ankles and feet. These changes can contribute to falls. (See the discussion on fall prevention in Chapter 3.) Hearing also decreases, especially for high-pitched sounds.
Cognitive functions of perceiving, registering, storing, and using information often change as a normal part of aging. Therefore it is important to differentiate between these expected findings and those of dementia, depression, and delirium (3Ds). Failure to correctly diagnosis pathologic cognitive problems may lead to a poor patient outcome.
Intellect does not decline as a result of aging. However, a person with certain health problems may have a decrease in cognitive level. Cognitive decline is frequently caused by drug interactions or toxicity or by an inadequate oxygen supply to the brain. Some older adults may need more time than a younger person to process questions, learn and process new information, solve problems, or complete analogies (Vance, 2009).
Subtle memory changes are typical for many older people. Long-term memory seems better than recall (recent) or immediate (registration) memory. Older adults may need more time to retrieve information. These changes may be partly due to the loss of cerebral neurons, which is associated with the aging process.
Circadian rhythm disorders may lead to wakefulness until later at night, with extended sleeping in the morning (a pattern opposite that of most health care facility routines). Many older adults require less sleep than do their younger counterparts.
Mental status may also decline as a result of infection. Often this change in mental status is a key early sign of an infectious process in the older patient, especially urinary tract infection.
Assessment Methods
Patient History
During your introduction, note the patient’s appearance and assess his or her speech, affect, and motor function. If he or she seems to have cognitive deficits or has trouble speaking or hearing, ask a family member or significant other to stay during the interview to help obtain an accurate history. Be sure that glasses, contact lenses, and hearing aids are available if the patient wears any of these aids.
Ask the patient about his or her medical history to determine its association with the current health problem. Inquire about the ability to perform ADLs. Knowing the level of daily activity helps establish a baseline for later comparison as the patient improves or worsens. Ask whether the patient is right-handed or left-handed. This information is important for several reasons:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree