Chapter 43 Assessment of the Nervous System
Safe and Effective Care Environment
Health Promotion and Maintenance
2. Identify factors that place patients at risk for neurologic health problems.
3. Explain pre-test and post-test care associated with neurologic diagnostic testing.
5. Briefly review the anatomy and physiology of the nervous system.
6. Describe common physiologic changes associated with aging that affect the nervous system.
7. Interpret findings from a comprehensive neurologic physical assessment.
8. Identify how to perform a rapid neurologic assessment and interpret findings.
9. Assess patients for complications of neurologic diagnostic tests.
http://evolve.elsevier.com/Iggy/
Animation: Motor Pathways and Clinical Evaluation of the CNS
Animation: Physiology of the Brain
Animation: Sensory Pathways and Clinical Evaluation of the CNS
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Video Clip: Deep Tendon Reflex
Video Clip: Fine Motor Coordination
Video Clip: Sensory Evaluation
Anatomy and Physiology Review
Nervous System Cells: Structure and Function
Neurons
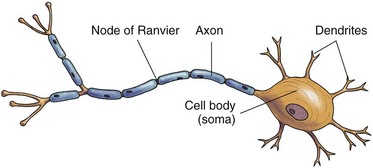
The basic unit of the nervous system, the neuron, transmits impulses, or “messages.” Some neurons are motor (causing movement or mobility), and some are sensory (causing sensation). Some process information, and some retain information. When a neuron receives an impulse from another neuron, the effect may be excitation or inhibition. Each neuron has a cell body, or soma; short, branching processes called dendrites; and a single axon (Fig. 43-1).
Many axons are covered by a myelin sheath—a white, lipid covering. Myelinated axons appear whitish and therefore are also called white matter. Nonmyelinated axons have a grayish cast and are called gray matter. Myelinated axons have gaps in the myelin called nodes of Ranvier. The nodes of Ranvier play a major role in impulse conduction (see Fig. 43-1). When the myelin is impaired, the impulses cannot travel from the brain to the rest of the body, such as in patients with multiple sclerosis.
Central Nervous System: Structure and Function
Brain
Major Parts of the Brain
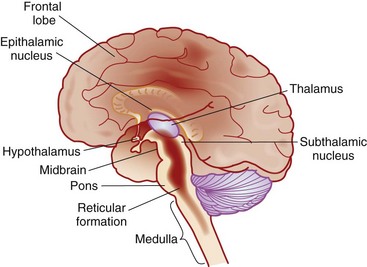
The diencephalon, which lies below the cerebrum, includes the thalamus, hypothalamus, and epithalamus (Fig. 43-2). The thalamus is the major “relay station,” or “central switchboard,” for the CNS. The hypothalamus plays a major role in autonomic nervous system control (controlling temperature and other functions) and intellectual function (cognition). The epithalamus contains the roof of the third ventricle and the pineal gland.
Located in the frontal lobe, the motor cortex controls voluntary movement. Corticospinal tracts, also called pyramidal tracts, begin in the motor cortex and travel through the brain before crossing in the medulla. This crossing explains how right motor cortex damage affects the movement in the left side of the body and vice versa, such as in many patients who have cerebral strokes. The cerebrum is divided into lobes by sulci (fissures). These lobes work together and are connected by nerve fibers. The name and main function of each lobe is listed in Table 43-1.
TABLE 43-1 CEREBRAL LOBE MAIN FUNCTIONS
| Frontal Lobe |
• The primary motor area (also known as the motor “strip” or cortex) • Broca’s speech center on the dominant side • Access to current sensory data • Access to past information or experience • Affective response to a situation • Regulates behavior based on judgment and foresight • Ability to develop long-term goals |
| Parietal Lobe |
| Temporal Lobe |
| Occipital Lobe |
| Limbic Lobe |
• Keep an extremity from overshooting an intended target
• Move from one skilled movement to another in an orderly sequence
• Predict distance or gauge the speed with which one is approaching an object
The brainstem includes the midbrain, pons, and medulla. The functions of these structures are presented in Table 43-2. Throughout the brainstem are special cells that constitute the reticular activating system (RAS), which controls awareness and alertness. For example, this tissue awakens a person from sleep when presented with a stimulus such as loud noise or pain or when it is time to awaken. The reticular formation area has many connections with the cerebrum, the rest of the brainstem, and the cerebellum.
TABLE 43-2 BRAINSTEM FUNCTIONS
| Medulla |
| Pons |
| Midbrain |
Circulation in the Brain
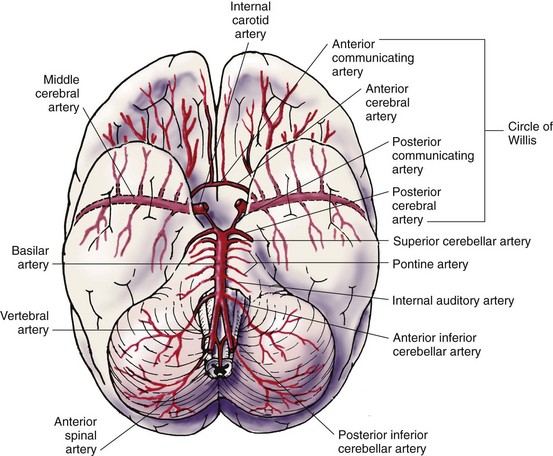
Circulation in the brain originates from the carotid and vertebral arteries (Fig. 43-3). The internal carotid arteries branch into the anterior cerebral artery (ACA) and middle cerebral arteries (MCA), the largest ones. The two posterior vertebral arteries become the basilar artery, which then divides into two posterior cerebral arteries. The anterior, middle, and posterior cerebral arteries are joined together by small communicating arteries to form a ring at the base of the brain known as the circle of Willis.
Spinal Cord
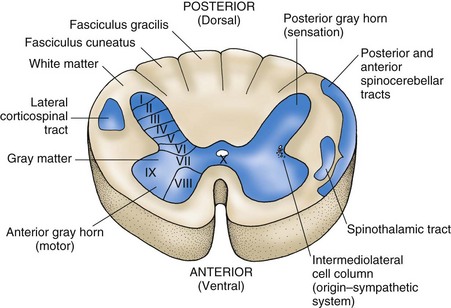
The spinal cord controls body movement (mobility); regulates organ function; processes sensory information from the extremities, trunk, and many internal organs (sensation); and transmits information to and from the brain. It contains H-shaped gray matter (neuron cell bodies) that is surrounded by white matter (myelinated axons). The white matter is divided into posterior, lateral, and anterior columns. Groups of cells in the white matter (ascending and descending tracts) have been fairly well identified (Fig. 43-4).
Ascending Tracts
The posterior white columns transmit this information to the thalamus:
Peripheral Nervous System: Structure and Function
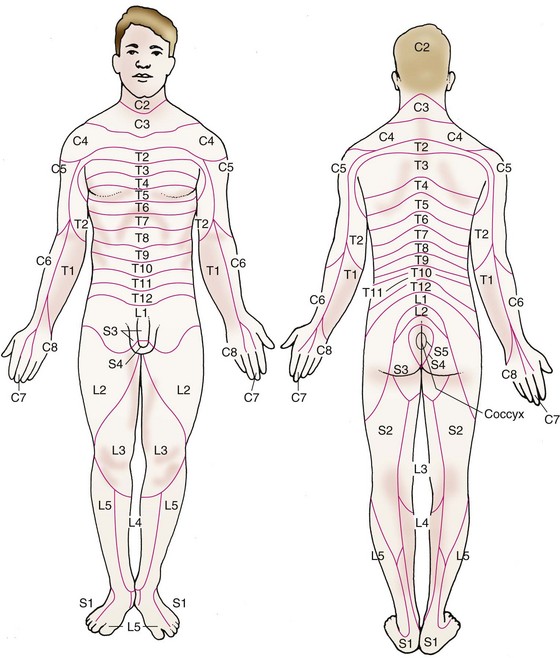
Each spinal nerve is responsible for the muscle innervation and sensory reception of a given area of the body. The cervical and thoracic spinal nerves are relatively close to their areas of responsibility, whereas the lumbar and sacral spinal nerves are some distance from theirs. Because the spinal cord ends between L1 and L2, the axons of the lumbar and sacral cord extend downward before exiting at the appropriate intervertebral foramen. The area controlled by each spinal nerve is roughly reflected in the dermatomes. Dermatomes represent sensory input from spinal nerves to specific areas of the skin (Fig. 43-5). For example, the patient with an injury to cervical spinal nerves C6 and C7 has sensory changes in the thumb, index finger, middle finger, middle of the palm, and back of the hand.
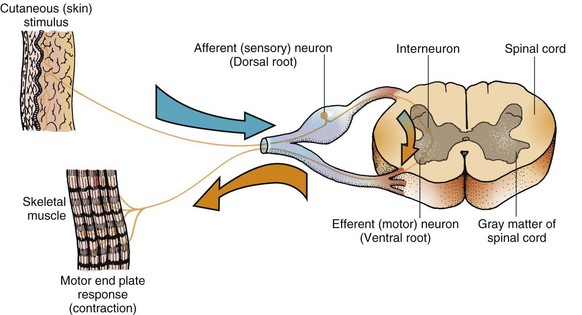
The reflex arc is a closed circuit of spinal and peripheral nerves and therefore requires no control by the brain (Fig. 43-6).
Reflexes consist of sensory input from:
• Skeletal muscles, tendons, skin, organs, and special senses
• Small cells in the spinal cord lying between the posterior and anterior gray matter (interneurons)
• Anterior motor neurons, along with the muscles they innervate
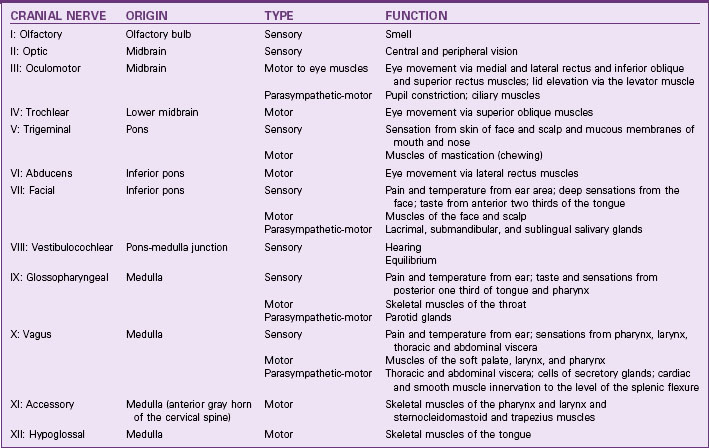
There are 12 cranial nerves. Their name, number, origin, type, and function are summarized in Table 43-3. Cranial nerve function is an important part of the nursing assessment of the patient with a neurologic problem. For example, cranial nerves II, III, IV, and VI are important for assessment of the patient with a stroke.
Neurologic Changes Associated with Aging
Neurologic changes associated with aging often affect mobility and sensation. Motor changes in late adulthood can cause slower movement and response time and decreased sensation (Chart 43-1). Any problems that affect the nerves, bones, muscles, or joints also affect motor and therefore ADL ability.
Chart 43-1 Nursing Focus on the Older Adult
Changes in the Nervous System Related to Aging
| PHYSIOLOGIC CHANGES | NURSING IMPLICATIONS | RATIONALES |
|---|---|---|
| Slower processing time | ||
| Recent memory loss | ||
| Decreased touch sensation | ||
| Change in perception of pain | ||
| Change in sleep patterns | ||
| Altered balance and/or decreased coordination | ||
| Increased risk for infection |
Sensory changes in older adults can also affect their daily activities. Pupils decrease in size, which restricts the amount of light entering the eye, and adapt more slowly. Older adults need increased lighting to see. Touch sensation decreases, which may lead to falls because the older person may not feel small objects or a step underfoot. Vibration sense may be lost in the ankles and feet. These changes can contribute to falls. (See the discussion on fall prevention in Chapter 3.) Hearing also decreases, especially for high-pitched sounds.
Intellect does not decline as a result of aging. However, a person with certain health problems may have a decrease in cognitive level. Cognitive decline is frequently caused by drug interactions or toxicity or by an inadequate oxygen supply to the brain. Some older adults may need more time than a younger person to process questions, learn and process new information, solve problems, or complete analogies (Vance, 2009).
Assessment Methods
Patient History
• The patient may be somewhat stronger on the dominant side, which is expected.
• The effects of cerebral injury or disease are more pronounced if the dominant hemisphere is involved.
Current Health Problems
Obtain information from the patient about current health problems as outlined in Charts 43-2 and 43-3.
Chart 43-2 Best Practice for Patient Safety & Quality Care
Establishing a Nursing Database: History