Chapter 52 Assessment of the Musculoskeletal System
Safe and Effective Care Environment
1. Collaborate with the physical and occupational therapists to perform a complete musculoskeletal assessment, including functional status, as needed.
Health Promotion and Maintenance
3. Assess the patient’s and family’s reaction to change in body image caused by a major musculoskeletal health problem.
4. Recognize the importance of support systems and effective strategies for the patient with unexpected altered body image caused by a musculoskeletal health problem.
5. Recall the anatomy and physiology of the musculoskeletal system.
6. Conduct a musculoskeletal history using Gordon’s Functional Health Patterns.
7. Assess patients for mobility, gait, motor skills, pain, and the use of assistive devices.
8. Interpret assessment findings in a patient with a musculoskeletal health problem.
9. Assess patients regarding iodine allergy before imaging assessments.
10. Explain the use of laboratory testing for a patient with a musculoskeletal health problem.
11. Develop a teaching plan to educate the patient and family about diagnostic procedures.
http://evolve.elsevier.com/Iggy/
Animation: Classification of Joints: Condyloid Joint
Animation: Classification of Joints: Gliding Joint (Hand)
Animation: Classification of Joints: Hinge Joint
Answer Key for NCLEX Examination Challenges
Review Questions for the NCLEX® Examination
Video Clip: Muscular Development and Strength
Anatomy and Physiology Review
Skeletal System
The skeletal system consists of 206 bones and multiple joints. The growth and development of these structures occur during childhood and adolescence and are not discussed in this text. Common physical skeletal differences among ethnic groups are listed in Table 52-1.
TABLE 52-1 MUSCULOSKELETAL DIFFERENCES IN SELECTED GROUPS
| GROUP | MUSCULOSKELETAL DIFFERENCES |
|---|---|
| African Americans | Greater bone density than Europeans, Asians, and Hispanics. Accounts for decreased incidence of osteoporosis. |
| Amish | Greater incidence of dwarfism than in other populations. |
| Chinese Americans | Bones are shorter and smaller with less bone density. Increased incidence of osteoporosis. |
| Egyptian Americans | Shorter in stature than Euro-Americans and African Americans. |
| Filipino/Vietnamese | Short in stature; adult height about 5 feet. |
| Irish Americans | Taller and broader than other Euro-Americans. Less bone density than African Americans. |
| Navajo American Indians | Taller and thinner than other American Indians. |
Bones
Types and Structure
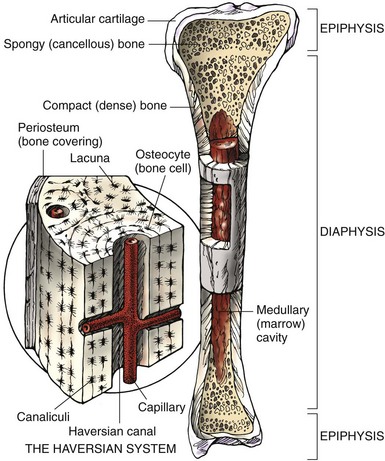
The second way bone is classified is by structure or composition. As shown in Fig. 52-1, the outer layer of bone, or cortex, is composed of dense, compact bone tissue. The inner layer, in the medulla, contains spongy, cancellous tissue. Almost every bone has both tissue types but in varying quantities. The long bone typically has a shaft, or diaphysis, and two knoblike ends, or epiphyses.
The structural unit of the cortical compact bone is the haversian system, which is detailed in Fig. 52-1. The haversian system is a complex canal network containing microscopic blood vessels that supply nutrients and oxygen to bone, as well as lacunae, which are small cavities that house osteocytes (bone cells). The canals run vertically within the hard cortical bone tissue.
Function
• Provides a framework for the body and allows the body to be weight bearing, or upright
• Supports the surrounding tissues (e.g., muscle and tendons)
• Assists in movement through muscle attachment and joint formation
• Protects vital organs, such as the heart and lungs
• Manufactures blood cells in red bone marrow
• Provides storage for mineral salts (e.g., calcium and phosphorus)
Numerous minerals and hormones affect bone growth and metabolism, including:
Vitamin D and its metabolites are produced in the body and transported in the blood to promote the absorption of calcium and phosphorus from the small intestine. They also seem to enhance PTH activity to release calcium from the bone. A decrease in the body’s vitamin D level can result in osteomalacia (softening of bone) in the adult. Vitamin D metabolism and osteomalacia are described in Chapter 53.
Growth hormone secreted by the anterior lobe of the pituitary gland is responsible for increasing bone length and determining the amount of bone matrix formed before puberty. During childhood, an increased secretion results in gigantism and a decreased secretion results in dwarfism. In the adult, an increase causes acromegaly, which is characterized by bone and soft-tissue deformities (see Chapter 65).
Joints
There are three types of joints in the body:
• Synarthrodial, or completely immovable, joints (e.g., in the cranium)
• Amphiarthrodial, or slightly movable, joints (e.g., in the pelvis)
• Diarthrodial (synovial), or freely movable, joints (e.g., the elbow and knee)
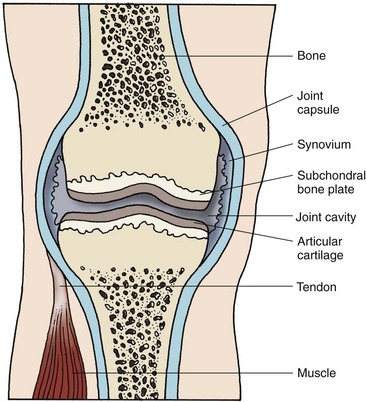
The diarthrodial, or synovial, joint is the most common type of joint in the body. Synovial joints are the only type lined with synovium, a membrane that secretes synovial fluid for lubrication and shock absorption. As shown in Fig. 52-2, the synovium lines the internal portion of the joint capsule but does not normally extend onto the surface of the cartilage at the spongy bone ends. Articular cartilage consists of a collagen fiber matrix impregnated with a complex ground substance. Patients with inflammatory types of arthritis often have synovitis (synovial inflammation) and breakdown of the cartilage. Bursae, small sacs lined with synovial membrane, are located at joints and bony prominences to prevent friction between bone and structures adjacent to bone. These structures can also become inflamed, causing bursitis.
Musculoskeletal Changes Associated with Aging
Osteopenia, or decreased bone density (bone loss), occurs as one ages. Many older adults, especially white, thin women, have severe osteopenia, a disease called osteoporosis. This condition causes postural and gait changes and predisposes the person to fractures. Chapter 53 discusses this health problem in detail.
Synovial joint cartilage can become less elastic and compressible as a person ages. As a result of these cartilage changes and continued use of joints, the joint cartilage becomes damaged, leading to osteoarthritis (OA). Genetic defects in cartilage may also contribute to joint disease. The most common joints affected are the weight-bearing joints of the hip, knee, and cervical and lumbar spine, but joints in the shoulder and upper extremity, feet, and hands can be affected. Refer to Chapter 20 for a complete discussion of OA.
As one ages, muscle tissue atrophies. Increased activity and exercise can slow the progression of atrophy and restore muscle strength. Musculoskeletal changes cause decreased coordination, loss of muscle strength, gait changes, and a risk for falls with injury. (See Chapter 3 for discussion on fall prevention.) Chart 52-1 lists the major anatomic and physiologic changes and implications for nursing care.
Chart 52-1 Nursing Focus on the Older Adult
Changes in the Musculoskeletal System Related to Aging
| PHYSIOLOGIC CHANGE | NURSING INTERVENTIONS | RATIONALES |
|---|---|---|
| Decreased bone density | Teach safety tips to prevent falls. | Porous bones are more likely to fracture. |
| Reinforce need to exercise, especially weight-bearing exercise. | Exercise slows bone loss. | |
| Increased bone prominence | Prevent pressure on bone prominences. | There is less soft tissue to prevent skin breakdown. |
| Kyphotic posture: widened gait, shift in the center of gravity | Teach proper body mechanics; instruct the patient to sit in supportive chairs with arms. | Correction of posture problems prevents further deformity; the patient should have support for bony structures. |
| Cartilage degeneration | Provide moist heat, such as a shower or warm, moist compresses. | Moist heat increases blood flow to the area. |
| Decreased range of motion (ROM) | Assess the patient’s ability to perform ADLs and mobility. | The patient may need assistance with self-care skills. |
| Muscle atrophy, decreased strength | Teach isometric exercises. | Exercises increase muscle strength. |
| Slowed movement | Do not rush the patient; be patient. | The patient may become frustrated if hurried. |
Assessment Methods
Patient History
In the assessment of a patient with an actual or potential musculoskeletal problem, a detailed and accurate history is helpful in identifying priority problems and nursing interventions (Chart 52-2). The history reveals information about the patient that can direct the physical assessment.
Based on Gordon, M. (2011). Manual of nursing diagnosis (12th ed.). New York: Jones & Bartlett.
Musculoskeletal Assessment
Using Gordon’s Functional Health Patterns
| Activity-Exercise Pattern | |
| Cognitive-Perceptual Pattern | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree