Chapter 55 Assessment of the Gastrointestinal System
Safe and Effective Care Environment
1. Assess patients for complications of diagnostic tests.
2. Prioritize post-test care for patients having endoscopic procedures.
Health Promotion and Maintenance
3. Identify factors that place patients at risk for GI problems.
4. Teach pre-test and post-test care for diagnostic GI testing to patients and families.
6. Briefly review the anatomy and physiology of the GI system.
7. Describe GI system changes associated with aging.
8. Perform a GI history using selected Gordon’s Functional Health Patterns.
9. Perform focused physical assessment for patients with suspected or actual GI health problems.
10. Explain and interpret common laboratory tests for a patient with a GI health problem.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Video Clip: Abdomen, Bowel Sounds
Video Clip: Palpation of Abdomen
Video Clip: Percussion, Abdomen
Video Clip: Percussion, Liver, Spleen
The GI system includes the GI tract (alimentary canal), consisting of the mouth, esophagus, stomach, small and large intestines, and rectum. The salivary glands, liver, gallbladder, and pancreas secrete substances into this tract to form the GI system (Fig. 55-1). The main function of the GI tract, with the aid of organs such as the pancreas and the liver, is the digestion of food to meet the body’s nutritional needs and the elimination of waste resulting from digestion. Adequate nutrition is required for proper functioning of the body’s organs and other cells (see the Concept Overview). The GI tract is susceptible to many health problems, including structural or mechanical alterations, impaired motility, infection, and cancer.
Anatomy and Physiology Review
Esophagus
The esophagus is a muscular canal that extends from the pharynx (throat) to the stomach and passes through the center of the diaphragm. Its primary function is to move food and fluids from the pharynx to the stomach. At the upper end of the esophagus is a sphincter referred to as the upper esophageal sphincter (UES). When at rest, the UES is closed to prevent air into the esophagus during respiration. The portion of the esophagus just above the gastroesophageal (GE) junction is referred to as the lower esophageal sphincter (LES). When at rest, the LES is normally closed to prevent reflux of gastric contents into the esophagus. If the LES does not work properly, gastroesophageal reflux disease (GERD) can develop (see Chapter 57).
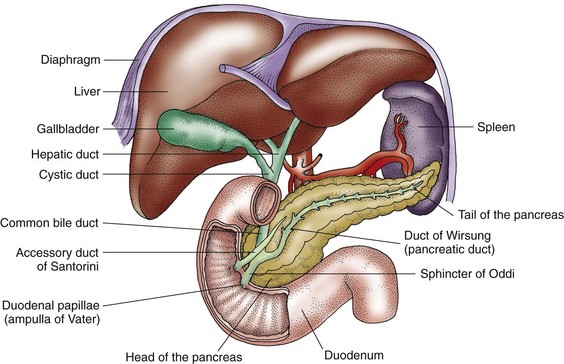
Pancreas
The pancreas is a fish-shaped gland that lies behind the stomach and extends horizontally from the duodenal C-loop to the spleen. The pancreas is divided into portions known as the head, the body, and the tail (Fig. 55-2).
Two major cellular bodies (exocrine and endocrine) within the pancreas have separate functions. The exocrine part is about 80% of the organ and consists of cells that secrete enzymes needed for digestion of carbohydrates, fats, and proteins (trypsin, chymotrypsin, amylase, and lipase). The endocrine part of the pancreas is made up of the islets of Langerhans, with alpha cells producing glucagon and beta cells producing insulin. These hormones produced are essential in the regulation of metabolism. Chapter 67 describes the endocrine function of the pancreas in detail.
Gastrointestinal Changes Associated with Aging
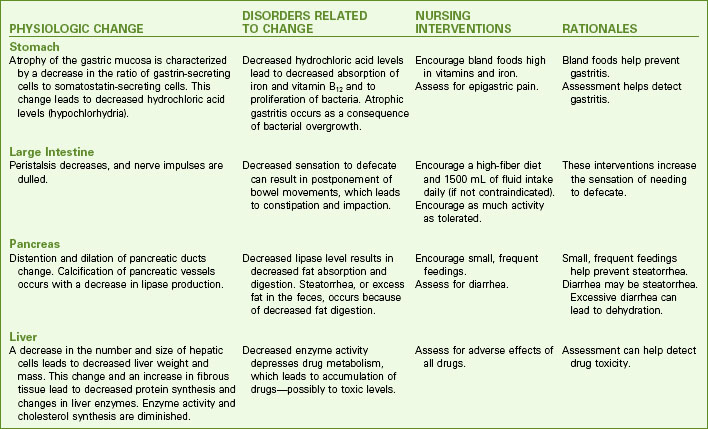
Physiologic changes occur as people age, especially ages 65 years and older. Changes in digestion and elimination that can affect nutrition are common. For example, decreased gastric hydrochloric acid (HCl) can lead to decreased absorption of essential minerals like iron. Chart 55-1 lists common GI changes and nursing implications when caring for older adults.
Assessment Methods
Patient History
The purpose of the health history is to determine the events related to the current health problem. One tool for assessing GI function is the nutritional-metabolic pattern and the elimination pattern assessment found in Chart 55-2. Focus questions about changes in appetite, weight, and stool. Determine the patient’s pain experience.
Gastrointestinal Assessment
Using Gordon’s Functional Health Patterns
Nutritional-Metabolic Pattern
• What is your typical daily food intake? Describe a day’s meals, snacks, and vitamins.
• How much salt do you typically add to your food? Do you use salt substitutes?
• How is your appetite? Any recent change?
• Do you have any difficulty chewing or swallowing?
• Do you wear dentures? How well do they fit?
• Do you ever experience indigestion or “heartburn”? How often? What seems to cause it? What helps it?
• Do you have pain, diarrhea, gas, or any other problems? Do any specific foods cause this for you?
• What is your typical daily fluid intake? What types of fluids (water, juices, soft drinks, coffee, tea)? How much?
• Have you had any recent change in your weight? Weight gain? Weight loss? How much?
• Have you noticed a change in the tightness of your rings or shoes? Tighter? Looser?
• Have you noticed any difference in the size of your abdomen?
Elimination Pattern
• What is your usual bowel elimination pattern? Frequency? Character? Discomfort? Laxatives?
• Do you have any pain or bleeding associated with bowel movements?
• Have you experienced any changes in your usual bowel pattern?
• When was your last rectal examination?
• Have you ever had an endoscopy or a colonoscopy?
• What is your usual urinary elimination pattern? Frequency? Amount? Color? Odor? Control?
Based on Gordon, M. (2011). Manual of nursing diagnosis (12th ed.). New York: Jones & Bartlett.
Family History and Genetic Risk
Ask about a family history of GI disorders. Some GI health problems have a genetic predisposition. For example, familial adenomatous polyposis (FAP) is an inherited autosomal dominant disorder that predisposes the patient to colon cancer (McCance et al., 2010). Specific genetic risks are discussed with the GI problems in later chapters.
Current Health Problems
Because GI clinical manifestations are often vague and difficult for the patient to describe, it is important to obtain a chronologic account of the current problem, symptoms, and any treatments taken. Furthermore, ask about the location, quality, quantity, timing (onset, duration), and factors that may aggravate or alleviate each symptom (see Chart 55-2).
• Color and consistency of the feces
• Occurrence of diarrhea or constipation
• Effective action taken to relieve diarrhea or constipation
• Presence of frank blood or tarry stools
Pain is a common concern of patients with GI tract disorders. The mnemonic PQRST may be helpful in organizing the current problem assessment (Jarvis, 2012):
P: Precipitating or palliative. What brings it on? What makes it better? Worse? When did you first notice it?
Q: Quality or quantity. How does it look, feel, or sound? How intense/severe is it?
R: Region or radiation. Where is it? Does it spread anywhere?
S: Severity scale. How bad is it (on a scale of 1 to 10)? Is it getting better, worse, or staying the same?
T: Timing. Onset—Exactly when did it first occur? Duration—How long did it last? Frequency—How often does it occur?
Physical Assessment
Physical assessment involves a comprehensive examination of the patient’s nutritional status, mouth, and abdomen. Nutritional assessment is discussed in detail in Chapter 63. Oral assessment is described in Chapter 56.
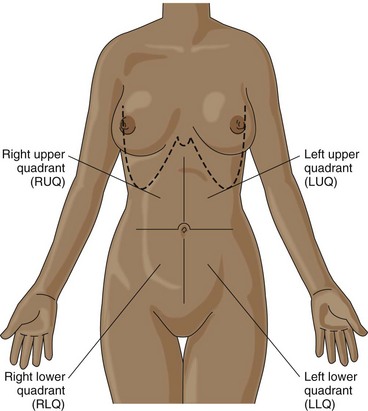
The abdominal examination usually begins at the patient’s right side and proceeds in a systematic fashion (Fig. 55-3):
Table 55-1 lists the organs that lie in each of these areas.
TABLE 55-1 LOCATION OF BODY STRUCTURES IN EACH ABDOMINAL QUADRANT
| Right Upper Quadrant (RUQ) |
| Right Lower Quadrant (RLQ) |
< div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
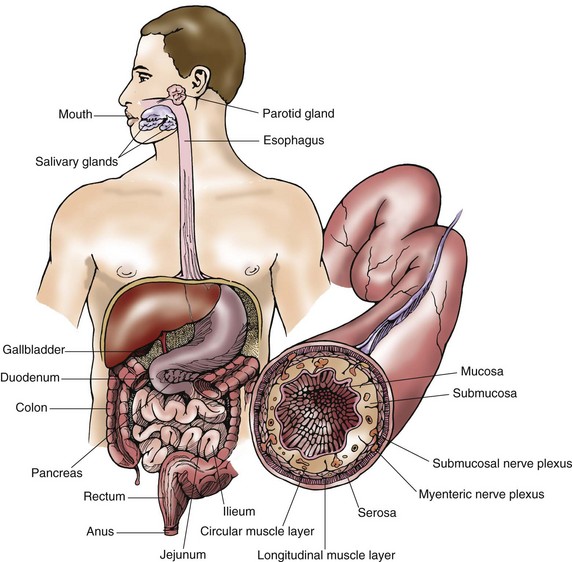
 inches (3 to 4 cm) of the large intestine is called the anal canal, which opens to the exterior of the body through the anus. Sphincter muscles surround the anal canal.
inches (3 to 4 cm) of the large intestine is called the anal canal, which opens to the exterior of the body through the anus. Sphincter muscles surround the anal canal.