Chapter 48 Assessment of the Eye and Vision
Safe and Effective Care Environment
1. Use aseptic technique when touching the eyelids or external eye structures.
2. Use appropriate technique when instilling eyedrops or eye ointments.
3. Verify that informed consent has been obtained before invasive tests of the eye or vision are performed.
Health Promotion and Maintenance
4. Teach all people about the use of eye protection equipment and strategies.
5. Perform health history and risk assessment for eye and vision problems.
6. Teach patients who have systemic health problems that may affect eye health and vision to adhere to prescribed therapies and to have yearly eye examinations by an ophthalmologist.
7. Teach patients and family members about what to expect during tests and procedures to assess vision and eye problems.
8. Provide the opportunity for the patient and family to express their concerns about a possible change in vision.
9. Explain the concept of refraction in relation to how the cornea, lens, aqueous humor, and vitreous humor contribute to vision.
10. Explain the relationship between intraocular pressure and eye health.
11. Use knowledge of anatomy and psychomotor skills when assessing the eye and vision.
12. Explain the eye changes associated with aging and their impact on vision.
13. Interpret the findings of visual acuity by the Snellen chart.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Anatomy and Physiology Review
Structure
Layers of the Eyeball
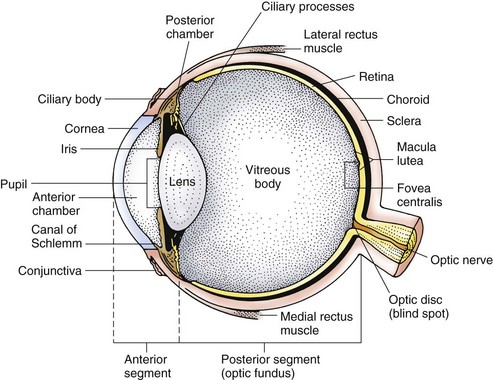
The eye has three layers, or coats (Fig. 48-1). The external layer is the sclera (the opaque tissue making up the “white” of the eye) and the transparent cornea on the front of the eye.
Refractive Structures and Media
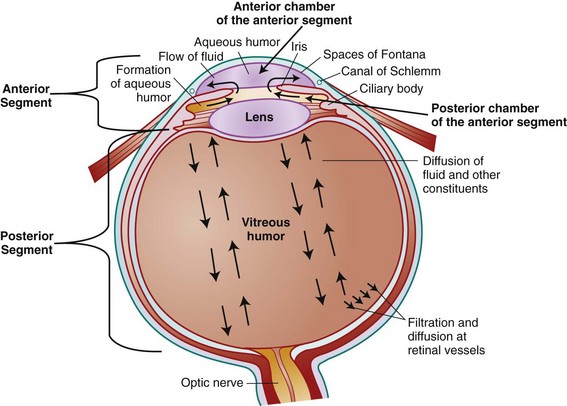
The cornea is the clear layer that forms the external bump on the front of the eye (see Fig. 48-1). The aqueous humor is a clear, watery fluid that fills the anterior and posterior chambers of the eye. Aqueous humor is continually produced by the ciliary processes and passes from the posterior chamber, through the pupil, and into the anterior chamber. This fluid drains through the canal of Schlemm into the blood to maintain a balanced intraocular pressure (IOP), the pressure within the eye (Fig. 48-2).
The eye is a hollow organ and must be kept in the shape of a ball for vision to occur. To maintain this shape, the gel in the posterior segment (vitreous humor) and the fluid in the anterior segment (aqueous humor) must be present in set amounts that apply pressure inside the eye to keep it inflated (McCance et al., 2010). This pressure is known as intraocular pressure or IOP. IOP has to be just right. If the pressure is too low, the eyeball is soft and collapses, preventing light from getting to the light-sensitive photoreceptors in the back of the eye on the retina. If the pressure becomes too high, the extra pressure compresses capillaries and nerve fibers in the eye. Pressure on retinal blood vessels prevents blood from flowing through them, and as a result the photoreceptors and nerve fibers become hypoxic. Compression of the fine nerve fibers prevents intracellular fluid flow, which also reduces nourishment to the distal portions of these thin nerve fibers. The increased intraocular pressure and resulting hypoxia of the photoreceptors and their synapsing nerve fibers is a condition called glaucoma. Continued hypoxia inside the eye result in photoreceptor necrosis and death and permanent nerve fiber damage. With extensive photoreceptor loss and nerve fiber damage, vision is lost and the person is permanently blind.
External Structures
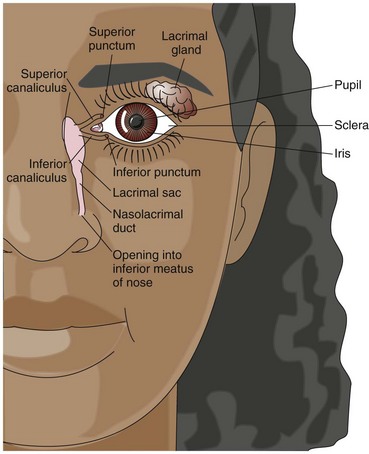
Tears are produced by a small lacrimal gland, which is located in the upper outer part of each orbit (Fig. 48-3). Tears flow across the front of the eye, toward the nose, and into the inner canthus. They drain through the punctum (an opening at the nasal side of the lid edges), into the lacrimal duct and sac, and then into the nose through the nasolacrimal duct.
Muscles, Nerves, and Blood Vessels
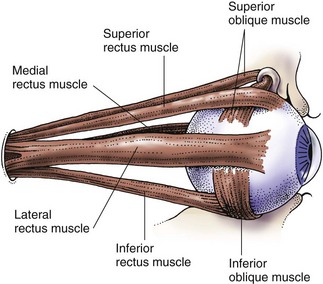
Six voluntary muscles rotate the eye and coordinate eye movements (Fig. 48-4 and Table 48-1). Coordinated eye movements ensure that the retina of each eye receives an image at the same time so only a single image is seen.
TABLE 48-1 FUNCTIONS OF OCULAR MUSCLES
| Superior Rectus Muscle |
| Lateral Rectus Muscle |
| Medial Rectus Muscle |
| Inferior Rectus Muscle |
| Superior Oblique Muscle |
| Inferior Oblique Muscle |
Function
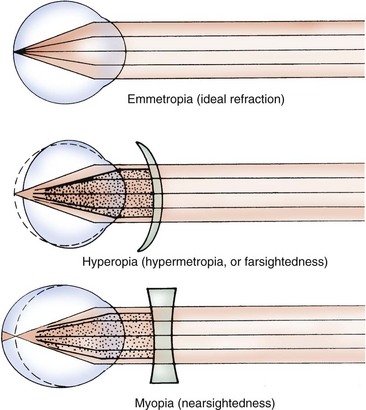
Refraction involves bending light rays from the outside world into the eye. The different curved surfaces and refractive media of the eye allow light to pass through to the retina. Each surface and media bends (refracts) light differently to focus an image on the retina. Emmetropia is the perfect refraction of the eye: with the lens at rest, light rays from a distant source (20 feet [6 m] or more) are focused into a sharp image on the retina. Fig. 48-5 shows the normal refraction of light within the eye. Images fall on the retina inverted and reversed left to right. For example, an object in the lower nasal visual field strikes the upper outer area of the retina.
Errors of refraction are common. Hyperopia (farsightedness or hypermetropia) occurs when the eye does not refract light enough. As a result, images actually fall (converge) behind the retina (see Fig. 48-5). Vision beyond 20 feet is normal, but near vision is poor. Hyperopia is corrected with a convex lens in eyeglasses or contact lenses.
Myopia (nearsightedness) occurs when the eye overbends the light and images converge in front of the retina (see Fig. 48-5). Near vision is normal, but distance vision is poor. Myopia is corrected with a biconcave lens in eyeglasses or contact lenses.
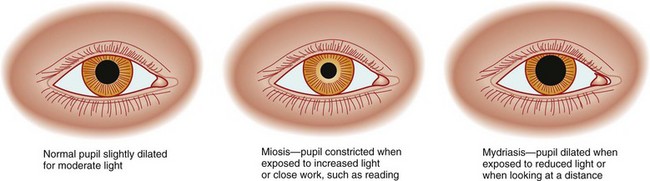
Pupillary constriction and dilation control the amount of light that enters the eye. If the level of light to one or both eyes is increased, both pupils constrict (become smaller). The amount of constriction depends on how much light is available and how well the retina can adapt to light changes. Pupillary constriction is called miosis, and pupillary dilation is called mydriasis (Fig. 48-6). Drugs can alter pupillary constriction.
Eye Changes Associated with Aging
Changes inside the eye cause visual acuity to decrease with age (Touhy & Jett, 2010). Age-related changes of the nervous system and in the eye support structures also reduce visual function (Chart 48-1).
Chart 48-1 Nursing Focus On The Older Adult
Changes in the Eye and Vision Related to Aging
| STRUCTURE/FUNCTION | CHANGE | IMPLICATION |
|---|---|---|
| Appearance | Eyes appear “sunken.” | Do not use eye appearance as an indicator for hydration status. |
| Arcus senilis forms. | Reassure patient that this change does not affect vision. | |
| Sclera yellows or appears blue. | Do not use sclera to assess for jaundice. | |
| Cornea | Cornea flattens, which blurs vision. | Encourage older adults to have regular eye examinations and wear prescribed corrective lenses for best vision. |
| Ocular muscles | Muscle strength is reduced, making it more difficult to maintain an upward gaze or maintain a single image. | Reassure patient that this is a normal happening and to re-focus gaze frequently to maintain a single image. |
| Lens | Elasticity is lost, increasing the near point of vision (making the near point of best vision farther away). | Encourage patient to wear corrective lenses for reading. |
| Lens hardens, compacts, and forms a cataract. | Stress the importance of yearly vision checks and monitoring for when intervention is needed. | |
| Iris | Decrease in ability to dilate results in small pupil size and poor adaptation to darkness. | Teach older adults the need for good lighting for best vision to avoid tripping and bumping into objects. |
| Pupil | Pupil size is smaller, reducing the ability to see in dim light. | Teach older adults the need for good lighting for best vision to avoid tripping and bumping into objects. |
| Color vision | Discrimination among greens, blues, and violets decreases. | The patient may not be able to use “dipstick” or other color-indicator monitors of health status. |
| Tears | Tear production is reduced, resulting in dry eyes, discomfort, and increased risk for corneal damage or eye infections. | Teach patient to use saline eyedrops on a schedule to reduce dryness. Teach patient to increase humidity in the home. |
Arcus senilis, an opaque, bluish white ring within the outer edge of the cornea, is caused by fat deposits (Fig. 48-7). Although very common, this change does not affect vision.
Health Promotion and Maintenance
Eye infections can lead to vision loss. Although the eye surface is not sterile, the sclera and cornea have no separate blood supply and thus are at risk for infection because the immunities in the blood do not reach these structures. Teach everyone to wash their hands before touching the eye or eyelid. Teach people who use eyedrops about the proper technique to use these drugs (Chart 48-2) and to not share eyedrops with others. If an eye has a discharge, teach the patient to use a separate eyedrop bottle for this eye and to wash the unaffected eye before washing the affected eye.
Chart 48-2 Patient And Family Education
Preparing For Self-Management: Using Eyedrops
• Check the name, strength, expiration date, color, and clarity of the eyedrops to be instilled.
• If both eyes are to receive the same drug and one eye is infected, use two separate bottles and carefully label each bottle with “right” or “left” for the correct eye.
• Remove the cap from the bottle.
• Tilt your head backward, open your eyes, and look up at the ceiling.
• Using your nondominant hand, gently pull the lower lid down against your cheek, forming a small pocket.
• Hold the eyedrop bottle (with the cap off) like a pencil, with the tip pointing down, with your dominant hand.
• Rest the wrist holding the bottle against your mouth or upper lip.
• Without touching any part of the eye or lid with the tip of the bottle, gently squeeze the bottle and release the prescribed number of drops into the pocket you have made with your lower lid.
• Gently release the lower lid.
• Close your eye gently (without squeezing the lids tightly).
• Gently press and hold the corner of the eye nearest the nose to close off the punctum and prevent the drug from being absorbed systemically.
• Without pressing on the lid, gently blot away any excess drug or tears with a tissue.
• Keep the eye closed for about 1 minute.
• Place the cap back on the bottle.
• Check to see whether the drug needs to be kept in the refrigerator.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree