Chapter 64 Assessment of the Endocrine System
Safe and Effective Care Environment
1. Ensure that agency laboratory procedures for collecting and handling specimens for endocrine function studies are followed.
Health Promotion and Maintenance
2. Identify factors that place patients at risk for endocrine health problems.
3. Teach everyone about the dangers of misusing or abusing hormones or steroids.
4. Encourage the patient to express concerns about a change in appearance, sexuality, or fertility.
5. Assess whether the patient has experienced recent changes in behavior or responses to stress.
6. Teach patients and family members about what to expect during tests and procedures to assess for endocrine problems.
7. Describe the relationship between hormones and receptor sites.
8. Explain negative feedback as a control mechanism for hormone secretion.
9. Apply the principles of anatomy and physiology to understand the role of the endocrine system in homeostasis.
10. Identify adaptations in nursing assessment or interventions needed because of age-related changes in endocrine function.
11. Interpret laboratory test findings and clinical manifestations for patients with possible endocrine problems.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
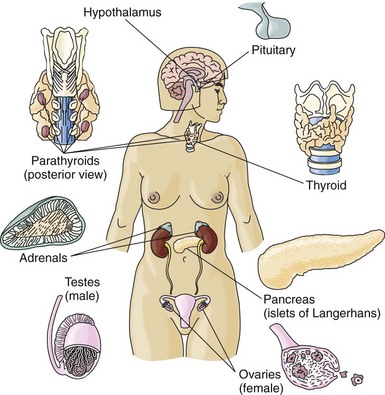
The endocrine system is made up of glands in many tissues and organs in a variety of body areas (Fig. 64-1). The purpose of all endocrine glands is to secrete hormones, which are natural chemicals that exert their effects on specific tissues known as target tissues. Target tissues are usually located some distance from the endocrine gland, with no direct physical connection between the endocrine gland and its target tissue. For this reason, endocrine glands are called “ductless” glands and must use the blood to transport secreted hormones to the target tissues (McCance et al., 2010). Endocrine glands include:
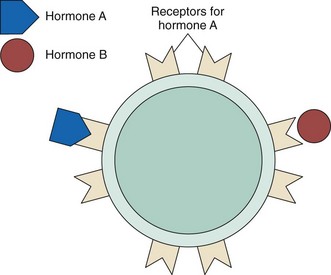
Table 64-1 lists hormones secreted by various endocrine glands. Hormones travel through the blood to all body areas but exert their actions only on target tissues. They recognize their target tissues and exert their actions by binding to receptors on or within the target tissue cells. In general, each receptor site type is specific for only one hormone. Hormone-receptor actions work in a “lock and key” manner in that only the correct hormone (key) can bind to and activate the receptor site (lock) (Fig. 64-2). Binding a hormone to its receptor causes the target tissue to change its activity, producing specific responses.
TABLE 64-1 PRINCIPAL HORMONES OF THE ENDOCRINE GLANDS
| GLAND | HORMONES |
|---|---|
| Hypothalamus | Corticotropin-releasing hormone (CRH) |
| Thyrotropin-releasing hormone (TRH) | |
| Gonadotropin-releasing hormone (GnRH) | |
| Growth hormone–releasing hormone (GHRH) | |
| Growth hormone–inhibiting hormone (somatostatin GHIH) | |
| Prolactin-inhibiting hormone (PIH) | |
| Melanocyte-inhibiting hormone (MIH) | |
| Anterior pituitary | Thyroid-stimulating hormone (TSH), also known as thyrotropin |
| Adrenocorticotropic hormone (ACTH, corticotropin) | |
| Luteinizing hormone (LH), also known as Leydig cell–stimulating hormone (LCSH) | |
| Follicle-stimulating hormone (FSH) | |
| Prolactin (PRL) | |
| Growth hormone (GH) | |
| Melanocyte-stimulating hormone (MSH) | |
| Posterior pituitary | Vasopressin (antidiuretic hormone [ADH]) |
| Oxytocin | |
| Thyroid | Triiodothyronine (T3) |
| Thyroxine (T4) | |
| Calcitonin | |
| Parathyroid | Parathyroid hormone (PTH) |
| Adrenal cortex | Glucocorticoids (cortisol) |
| Mineralocorticoids (aldosterone) | |
| Ovary | Estrogen |
| Progesterone | |
| Testes | Testosterone |
| Pancreas | Insulin |
| Glucagon | |
| Somatostatin |
Disorders of the endocrine system usually are related to:
Anatomy and Physiology Review
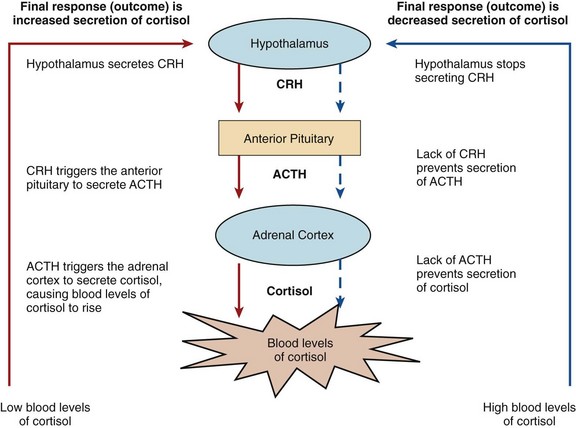
• The central nervous system receives and reacts to various sensory inputs transmitted to the hypothalamus as stimuli.
• The hypothalamus responds to the stimuli with the production and release of either releasing or inhibiting factors, which are transported to the pituitary.
• In the pituitary gland, the releasing or inhibiting factors either stimulate or inhibit the release of specific hormones.
• The anterior pituitary hormones then control the secretion of hormones in other endocrine glands. These glands then secrete hormones into the blood that then act on their target organs or tissues, resulting in a change of at least one function.
An example of complex control is the interaction of the hypothalamus and the anterior pituitary with the adrenal cortex (Fig. 64-3). Low blood levels of cortisol from the adrenal cortex stimulate the secretion of corticotropic-releasing hormone (CRH) in the hypothalamus. CRH stimulates the anterior pituitary gland to secrete adrenocorticotropic hormone (ACTH). ACTH then triggers the release of cortisol from the adrenal cortex. The rising blood levels of cortisol inhibit CRH release from the hypothalamus. Without CRH, the anterior pituitary gland stops secretion of ACTH. In response, normal blood cortisol levels are maintained.
Hypothalamus and Pituitary Glands
The endocrine function of the hypothalamus is to produce regulatory hormones (see Table 64-1). Some of these hormones are released into the blood and travel to the anterior pituitary, where they either stimulate or inhibit the release of anterior pituitary hormones.
The pituitary gland is located at the base of the brain in a protective pocket of the sphenoid bone (see Fig. 64-1). The pituitary gland is about 1 cm in diameter and is divided into the anterior lobe (adenohypophysis) and the posterior lobe (neurohypophysis). Nerve fibers in the hypophysial stalk connect the hypothalamus to the posterior pituitary (Fig. 64-4).
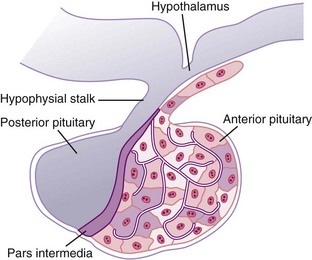
FIG. 64-4 The hypothalamus, hypophysial stalk, anterior pituitary gland, and posterior pituitary gland.
In response to the releasing hormones of the hypothalamus, the anterior pituitary secretes tropic hormones, which are hormones that stimulate other endocrine glands. Other pituitary hormones, such as prolactin, produce their effect directly on final target tissues (Table 64-2).
TABLE 64-2 PITUITARY HORMONES: TARGET TISSUES AND SUBSEQUENT ACTIONS
| HORMONE | TARGET TISSUE | ACTIONS |
|---|---|---|
| Anterior Pituitary | ||
| TSH (thyroid-stimulating hormone or thyrotropin) | Thyroid | Stimulates synthesis and release of thyroid hormone |
| ACTH (adrenocorticotropic hormone, corticotropin) | Adrenal cortex | Stimulates synthesis and release of corticosteroids and adrenocortical growth |
| LH (luteinizing hormone [known as Leydig cell–stimulating hormone in males]) | Ovary Testis | Stimulates ovulation and progesterone secretion Stimulates testosterone secretion |
| FSH (follicle-stimulating hormone [known as interstitial cell– or Sertoli cell–stimulating hormone in males]) | Ovary Testis | Stimulates estrogen secretion and follicle maturation Stimulates spermatogenesis |
| PRL (prolactin) | Mammary glands | Stimulates breast milk production |
| GH (growth hormone) | Bone and soft tissue | Promotes growth through lipolysis, protein anabolism, and insulin antagonism |
| MSH (melanocyte-stimulating hormone) | Melanocytes | Promotes pigmentation |
| Posterior Pituitary* | ||
| Vasopressin (antidiuretic hormone [ADH]) | Kidney | Promotes water reabsorption |
| Oxytocin | Uterus and mammary glands | Stimulates uterine contractions and ejection of breast milk |
* These hormones are synthesized in the hypothalamus and are stored in the posterior pituitary gland. They are transported from the hypothalamus down the hypothalamic stalk to the posterior pituitary while bound to proteins known as neurophysins.
Gonads
During puberty in the male, the increased secretion of gonadotropins (luteinizing hormone [LH] and follicle-stimulating hormone [FSH]) from the anterior pituitary gland stimulates maturation of the testes, production of testosterone, and maturation of the external genitalia. During puberty in the female, increased secretion of the same gonadotropins stimulates ovarian maturation, estrogen production, ovulation, and maturation of the external genitalia. The function of the testes and ovaries is detailed in Chapter 72.
Adrenal Glands
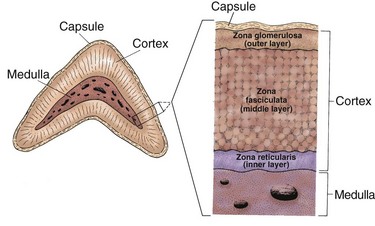
The adrenal glands are vascular, tent-shaped organs on the top of each kidney that have an outer cortex and an inner medulla (see Fig. 64-1). The adrenal hormones have effects throughout the body.
Adrenal Cortex
The adrenal cortex makes up about 90% of the adrenal gland and has cells divided into three layers (Fig. 64-5). Mineralocorticoids are the hormones produced in the zona glomerulosa and help control the body’s sodium and potassium content. Glucocorticoids, androgens, and estrogens are produced in the zona fasciculata and zona reticularis. The hormones secreted by the cortex are often called adrenal steroids or corticosteroids.
Renin is produced by specialized cells of the renal afferent arterioles. Its release is triggered by a decrease in extracellular fluid volume from blood loss, sodium loss, or posture changes. Renin converts renin substrate (formerly called angiotensinogen), a plasma protein, to angiotensin I. Angiotensin I is converted by a converting enzyme to form angiotensin II, the active form of angiotensin. In turn, angiotensin II stimulates the secretion of aldosterone. Chapter 13 (see Fig. 13-6) further explains the renin-angiotensin system. Aldosterone causes the kidney to reabsorb sodium and water to bring the plasma volume and osmolarity back to normal.
Cortisol also influences other important body processes. For example, it must be present for catecholamine action and maintaining the normal excitability of the heart muscle cells. Glucocorticoid functions are listed in Table 64-3.
TABLE 64-3 FUNCTIONS OF GLUCOCORTICOID HORMONES
As described earlier and shown in Fig. 64-3, when blood cortisol levels are low, the hypothalamus secretes CRH, which triggers the pituitary to release ACTH. Then ACTH triggers the adrenal cortex to secrete cortisol. Adequate or elevated blood levels of cortisol inhibit the release of CRH and ACTH. This inhibitory effect is an example of a negative feedback system.
Adrenal Medulla
Catecholamines exert their actions on many target organs (Table 64-4). Activation of the sympathetic nervous system, which then releases adrenal medullary catecholamines, is an important part of the body’s response to stress. Catecholamines are secreted in small amounts at all times to maintain homeostasis. Stress triggers increased secretion of these hormones. This sympathetic activation results in the “fight-or-flight” response, a state of heightened physical and emotional awareness.
TABLE 64-4 CATECHOLAMINE RECEPTORS AND EFFECTS OF ADRENAL MEDULLARY HORMONE STIMULATION ON SELECTED ORGANS AND TISSUES
| ORGAN OR TISSUE | RECEPTORS | EFFECTS |
|---|---|---|
| Heart | Beta1 | Increased heart rate |
| Increased contractility | ||
| Blood vessels | Alpha | Vasoconstriction |
| Beta2 | Vasodilation | |
| Gastrointestinal tract | Alpha | Increased sphincter tone |
| Beta | Decreased motility | |
| Kidneys | Beta2 | Increased renin release |
| Bronchioles | Beta2 | Relaxation; dilation |
| Bladder | Alpha | Sphincter contractions |
| Beta2 | Relaxation of detrusor muscle | |
| Skin | Alpha | Increased sweating |
| Fat cells | Beta | Increased lipolysis |
| Liver | Alpha | Increased gluconeogenesis and glycogenolysis |
| Pancreas | Alpha | Decreased glucagon and insulin release |
| Beta | Increased glucagon and insulin release | |
| Eyes | Alpha | Dilation of pupils |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree