Chapter 50 Assessment of the Ear and Hearing
Safe and Effective Care Environment
Health Promotion and Maintenance
2. Teach all people how to perform ear hygiene safely.
3. Teach all people to use ear protection equipment and strategies.
4. Teach patients and family members about what to expect during tests and procedures to assess ear and hearing problems.
5. Provide opportunities for the patient and family to express feelings and concerns about a possible change in hearing.
6. Identify people at risk for hearing problems as a result of drug therapy, genetic predisposition, or exposure to environmental hazards.
7. Perform a clinical ear and hearing assessment, including health history and psychosocial assessment.
8. Describe adaptations needed when caring for patients who have age-related changes in the structure of the ear and hearing.
9. Identify 10 common drugs that affect hearing.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Anatomy and Physiology Review
Structure
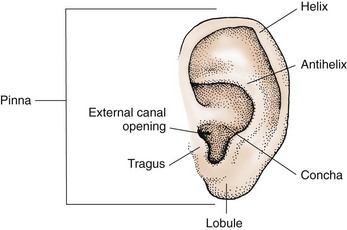
External Ear
The pinna is the part of the external ear that is composed of cartilage covered by skin and attached to the head at about a 10-degree angle. It is embedded in the temporal bone on both sides of the head at the level of the eyes. The external ear also includes the mastoid process, which is the bony ridge located over the temporal bone behind the pinna. The external ear extends from the pinna through the external ear canal to the tympanic membrane (eardrum) (Fig. 50-1). The ear canal is slightly S-shaped and lined with cerumen (wax)-producing glands, sebaceous glands, and hair follicles. Cerumen helps protect and lubricate the ear canal. The hair follicles and cerumen protect the eardrum and the middle ear. The distance from the opening of the ear canal to the eardrum in an adult is 1 to  inches (2.5 to 3.75 cm).
inches (2.5 to 3.75 cm).
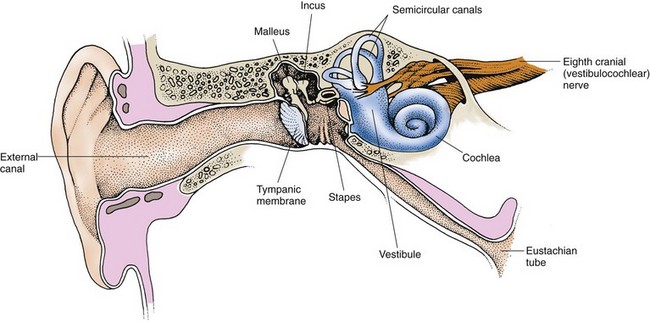
Middle Ear
The middle ear consists of a compartment called the epitympanum. Located in the epitympanum are the top opening of the eustachian tube and three small bones known as the bony ossicles, which are the malleus (hammer), the incus (anvil), and the stapes (stirrup) (Fig. 50-2). The bony ossicles are joined loosely, thereby moving with vibrations created when sound waves hit the eardrum.
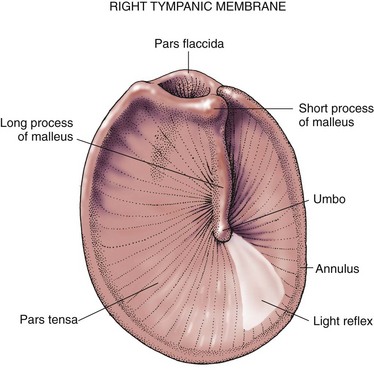
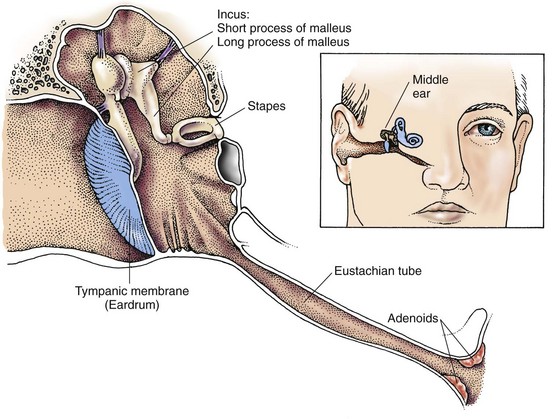
The eardrum, a thick sheet of tissue, is transparent, opaque, or pearly gray and moves when air is injected into the external canal. The landmarks on the eardrum include the annulus, the pars flaccida, and the pars tensa. These correspond to the parts of the malleus that can be seen through the transparent eardrum. The eardrum is attached to the first bony ossicle, the malleus, at the umbo (Fig. 50-3). The umbo is seen through the eardrum membrane as a white dot and is one end of the long process of the malleus. The pars flaccida is that portion of the eardrum above the short process of the malleus. The pars tensa is that portion surrounding the long process of the malleus.
The middle ear is separated from the inner ear by the round window and the oval window. The eustachian tube begins at the floor of the middle ear and extends to the throat. The tube opening in the throat is surrounded by adenoid lymphatic tissue (Fig. 50-4). The eustachian tube allows the pressure on both sides of the eardrum to equalize. Secretions from the middle ear drain through the tube into the throat.
Inner Ear
The inner ear is on the other side of the oval window and contains the semicircular canals, the cochlea, the vestibule, and the distal end of the eighth cranial nerve (see Fig. 50-2). The semicircular canals are tubes made of cartilage and contain fluid and hair cells. These canals are connected to the sensory nerve fibers of the vestibular portion of the eighth cranial nerve. The fluid and hair cells within the canals help maintain the sense of balance.
Ear and Hearing Changes Associated with Aging
Ear and hearing changes related to aging are listed in Chart 50-1, along with implications for care of older patients who have these changes. Some of the ear changes, such as an increase in ear size, are harmless. Other changes to ear structures may pose threats to the hearing ability of older adults.
Chart 50-1 Nursing Focus on the Older Adult
Age-Related Changes in the Ear and Hearing
Assessment Methods
Patient History
During the interview, sit in adequate light and face the patient to allow him or her to see you speak. Use short, simple language the patient is comfortable with rather than long medical terms. Obtain data on demographics, personal and family history, socioeconomic status, current health problems, and the use of remedies for ear problems. Chart 50-2 lists important questions to ask about functional hearing.
Ear and Hearing Assessment
Using Gordon’s Functional Health Patterns
Cognitive-Perceptual Pattern
• Do you have any hearing difficulty?
• Do you use any type of hearing aid?
• Do you notice that you have the volume of the television or radio set at an increased level?
• Are you sitting closer to the television or radio to hear more clearly?
• Do you have difficulty in your ability to hear or follow conversations in a noisy environment, such as a restaurant?
• Do you have difficulty hearing high-pitched sounds like the doorbell?
Health Perception–Health Management Pattern
• Have you had your hearing checked?
• If you are or were exposed to environmental noise, have you consistently used appropriate hearing protection?
• Do you avoid cleaning your ear canals with foreign objects such as toothpicks or paper clips?
• Have you discussed with your health care provider the side effects of any drugs you may be taking that might affect your ear and hearing?
Based on Gordon, M. (2011). Manual of nursing diagnosis (12th ed.). New York: Jones & Bartlett.
• Any invasive instruments routinely used to clean the ear (e.g., Q-Tip, match, bobby pin, key)
• Type and pattern of ear hygiene
• Exposure to loud noise or music
• Air travel (especially in unpressurized aircraft)
• Swimming and whether ear protection is used
• History of hereditary factors that can cause progressive hearing loss
• History of health problems that can decrease the blood supply to the ear such as heart disease, hypertension, or diabetes
• History of vitiligo (a pigment disorder in which there may be a loss of melanin-containing cells in the inner ear, resulting in hearing loss)
• History of smoking (reduces oxygenation of the cochlea)
• History of vitamin B12 and folate deficiency (associated with age-related hearing loss)
If the patient uses foreign objects to clean the ear canal (e.g., bobby-pins, Q-tips, toothpicks, keys), explain the danger in using these objects. They can scrape the skin of the canal, push cerumen up against the eardrum, and even puncture the eardrum. If the patient says that cerumen buildup is a problem, teach him or her to use an ear irrigation syringe and proper solutions to remove it. Chart 50-3 describes techniques to teach patients how to remove cerumen safely.
Chart 50-3 Patient and Family Education
Preparing for Self-Management: Self–Ear Irrigation for Cerumen Removal
• Do not attempt to remove ear wax or irrigate the ears if you have ear tubes or if you have blood, pus, or other drainage from the ear.
• Use an ear syringe designed for the purpose of wax removal. These are inexpensive, available at most drug stores, reusable, and can be used by more than one person when cleaned properly between uses.
• The safest type of ear syringe to use is one that has a right-angle or “elbow” in the tip.
• Irrigating your ears in the shower is an easy method.
• Always use tap water that feels just barely warm to you. If you are using a thermometer, keep the water temperature as close as possible to 98° or 99° F. Water that is warmer or colder can make you feel dizzy and nauseated.
• If your ear wax is thick and sticky, you may need to place a few drops of a warm ceruminolytic (commercial eardrops that soften ear wax) into the ear an hour or so before you irrigate the ear. Other substances that can be used for this purpose include baby oil or mineral oil.
• Fill the syringe with the lukewarm tap water.
• If you are using a syringe with an elbow tip, place only the last part of the tip into your ear and aim it toward the roof of your ear canal.
• If you are using a straight-tipped syringe, insert the tip only about  – to
– to  -inch into your ear canal, aiming toward the roof of the canal.
-inch into your ear canal, aiming toward the roof of the canal.
• Hold your head at a 30-degree angle to the side you are irrigating.
• Use one hand to hold the syringe and the other to push the plunger or squeeze the bulb.
• Apply gentle but firm continuous pressure, allowing the water to flow against the top of the canal.
• Do not use blasts or bursts of sudden pressure.
• The ear canal should fill, and water will begin to flow out, bringing ear wax and debris with it.
• If a dental water-pressure irrigator is used, put it on the lowest possible setting.
• This process should not be painful! If pain occurs, decrease the pressure. If pain persists, stop the irrigation.
• Continue the irrigation until at least a cup of solution has washed into and out from your ear canal. (You may have to refill the syringe.)
• Tilting your head at a 90-degree angle to the side should allow most, if not all, of the water to drain out of your ear.
• Repeat the procedure on the other ear.
• If you feel that water is still in the canal, hold a hair dyer on a low setting near the ear.
• Irrigate your ears anytime from weekly to monthly, depending on how fast your ear wax collects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree