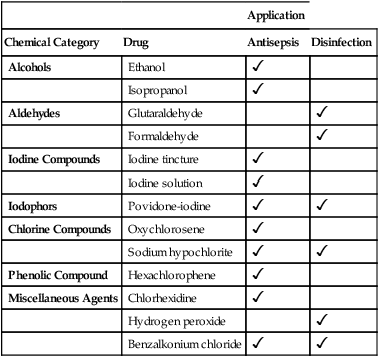
CHAPTER 96 Antiseptics and disinfectants derive from a variety of chemical families, ranging from alcohols to iodine compounds to phenols. The various antiseptics and disinfectants differ from one another with respect to mechanism of action, time course, and antimicrobial spectrum. In almost all cases, the drugs employed as disinfectants are not used for antisepsis and vice versa. The more commonly employed antiseptics and disinfectants are listed in Table 96–1. For each drug, the table indicates chemical family and clinical use (antisepsis, disinfection, or both). TABLE 96–1 Antiseptics and Disinfectants: Chemical Category and Application
Antiseptics and disinfectants
Properties of individual antiseptics and disinfectants

Application
Chemical Category
Drug
Antisepsis
Disinfection
Alcohols
Ethanol

Isopropanol

Aldehydes
Glutaraldehyde

Formaldehyde

Iodine Compounds
Iodine tincture

Iodine solution

Iodophors
Povidone-iodine


Chlorine Compounds
Oxychlorosene

Sodium hypochlorite


Phenolic Compound
Hexachlorophene

Miscellaneous Agents
Chlorhexidine

Hydrogen peroxide

Benzalkonium chloride



Antiseptics and disinfectants
Get Clinical Tree app for offline access


