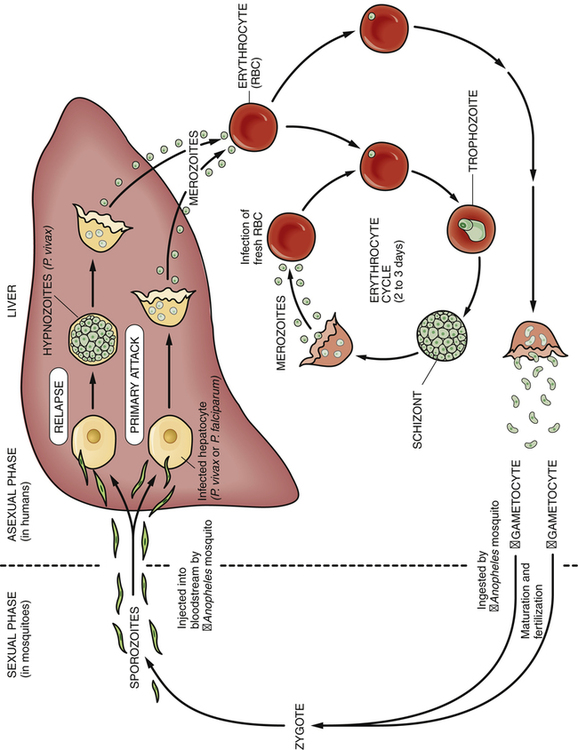
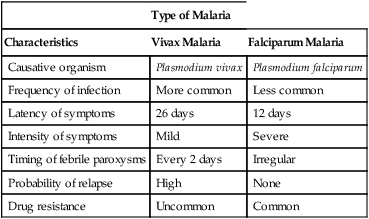
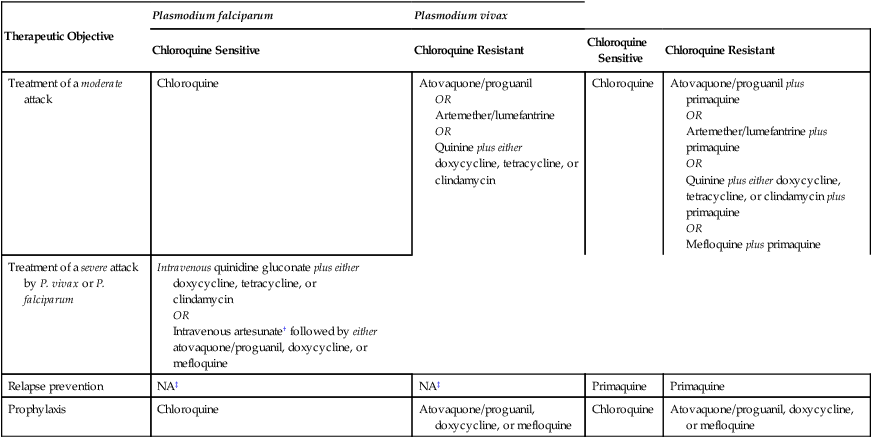
CHAPTER 98 In order to understand the actions and specific applications of antimalarial drugs, we must first understand the life cycle of the malaria parasite. As indicated in Figure 98–1, the cycle takes place in two hosts: humans and the female Anopheles mosquito. Asexual reproduction occurs in humans. Sexual reproduction occurs in the mosquito. Sexual reproduction begins with the formation of gametocytes, which differentiate from some of the merozoites in red blood cells (see Figure 98–1). Following their release from red cells, gametocytes enter a female Anopheles mosquito when she ingests blood while feeding. Within the mosquito, the gametocytes differentiate into mature forms, after which fertilization takes place. The resulting zygote then produces sporozoites, thus completing sexual reproduction. Malaria is caused by four different species of Plasmodium. In this chapter, we limit discussion to the two species encountered most: Plasmodium vivax and Plasmodium falciparum. Malaria caused by either species is characterized by high fever, chills, and profuse sweating. However, despite similarity of symptoms, these forms of malaria are very different—especially with regard to severity of symptoms, relapse, and drug resistance. These and other differences are summarized in Table 98–1. TABLE 98–1 Comparison of Vivax Malaria and Falciparum Malaria Selection of antimalarial drugs is based largely on two factors: (1) the goal of treatment and (2) drug resistance of the causative strain of Plasmodium. Drugs of choice for treatment and prophylaxis are discussed below and summarized in Table 98–2. TABLE 98–2 *All drugs are given orally except where noted otherwise. †Artesunate is available from the Centers for Disease Control and Prevention. ‡Not applicable. Malaria caused by P. falciparum does not relapse following successful treatment of the acute attack.
Antiprotozoal drugs I: antimalarial agents
Life cycle of the malaria parasite
Types of malaria

Type of Malaria
Characteristics
Vivax Malaria
Falciparum Malaria
Causative organism
Plasmodium vivax
Plasmodium falciparum
Frequency of infection
More common
Less common
Latency of symptoms
26 days
12 days
Intensity of symptoms
Mild
Severe
Timing of febrile paroxysms
Every 2 days
Irregular
Probability of relapse
High
None
Drug resistance
Uncommon
Common
Principles of antimalarial therapy
Therapeutic objectives
Drug selection

Therapeutic Objective
Plasmodium falciparum
Plasmodium vivax
Chloroquine Sensitive
Chloroquine Resistant
Chloroquine Sensitive
Chloroquine Resistant
Treatment of a moderate attack
Chloroquine
Atovaquone/proguanil
OR
Artemether/lumefantrine
OR
Quinine plus either doxycycline, tetracycline, or clindamycin
Chloroquine
Atovaquone/proguanil plus primaquine
OR
Artemether/lumefantrine plus primaquine
OR
Quinine plus either doxycycline, tetracycline, or clindamycin plus primaquine
OR
Mefloquine plus primaquine
Treatment of a severe attack by P. vivax or P. falciparum
Intravenous quinidine gluconate plus either doxycycline, tetracycline, or clindamycin
OR
Intravenous artesunate† followed by either atovaquone/proguanil, doxycycline, or mefloquine
Relapse prevention
NA‡
NA‡
Primaquine
Primaquine
Prophylaxis
Chloroquine
Atovaquone/proguanil, doxycycline, or mefloquine
Chloroquine
Atovaquone/proguanil, doxycycline, or mefloquine
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Antiprotozoal drugs I: antimalarial agents
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access