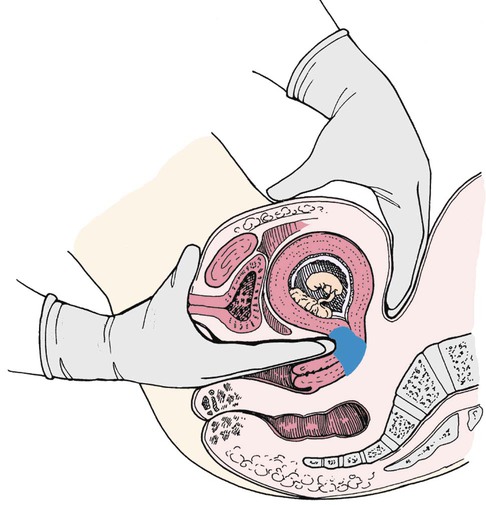
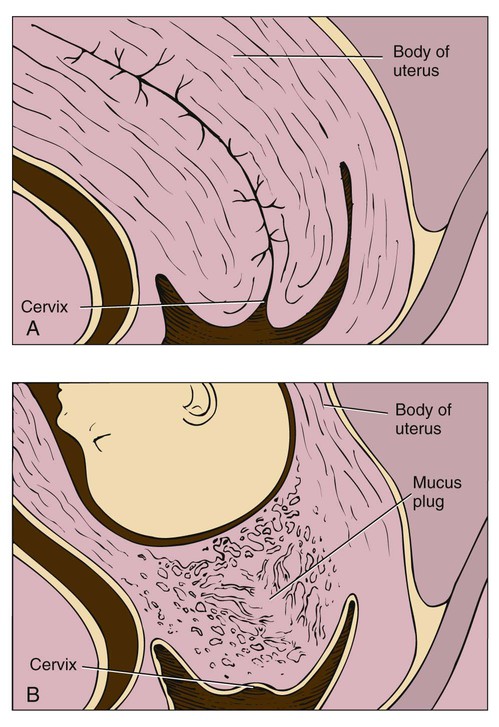
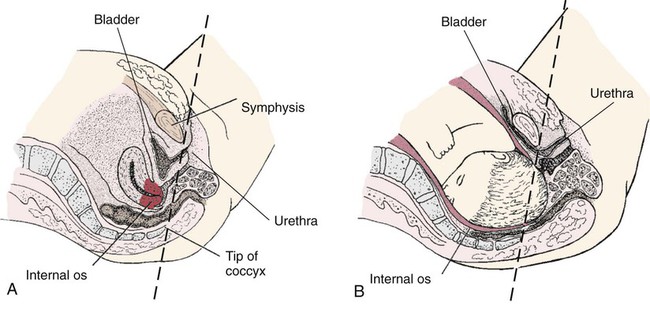
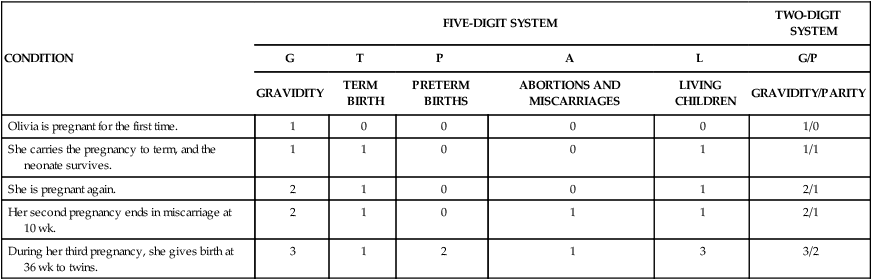
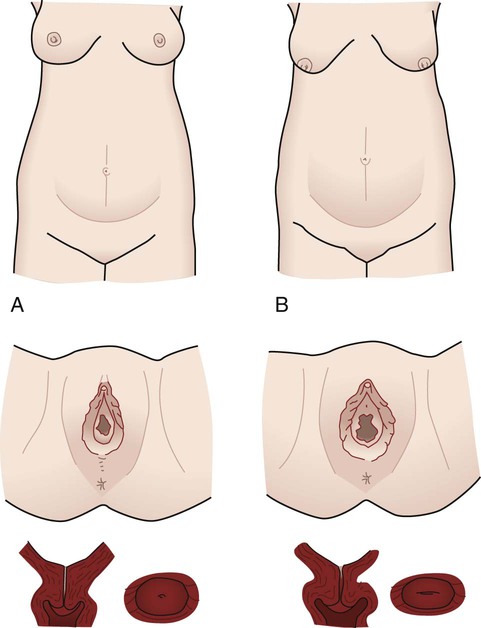
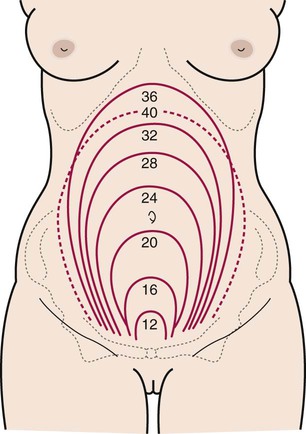
Chapter 7 On completion of this chapter, the reader will be able to: • Determine gravidity and parity using the two- and five-digit systems. • Describe the various types of pregnancy tests, including the timing of tests and interpretation of results. • Explain the expected maternal anatomic and physiologic adaptations to pregnancy. • Differentiate among presumptive, probable, and positive signs of pregnancy. • Identify maternal hormones produced during pregnancy, their target organs, and their major effects on pregnancy. • Compare the characteristics of the abdomen, vulva, and cervix of the nullipara and multipara. An understanding of the following terms used to describe pregnancy and the pregnant woman (Cunningham, Leveno, Bloom, et al., 2010) is essential to the study of maternity care: Gravida—A woman who is pregnant Multigravida—A woman who has had two or more pregnancies Multipara—A woman who has completed two or more pregnancies to 20 weeks of gestation or more Nulligravida—A woman who has never been pregnant and is not currently pregnant Nullipara—A woman who has not completed a pregnancy with a fetus or fetuses beyond 20 weeks of gestation Parity—The number of pregnancies in which the fetus or fetuses have reached 20 weeks of gestation, not the number of fetuses (e.g., twins) born. Parity is not affected by whether the fetus is born alive or is stillborn (i.e., showing no signs of life at birth). Postdate or postterm—A pregnancy that goes beyond 42 weeks of gestation Preterm—A pregnancy that has reached 20 weeks of gestation but ends before completion of 37 weeks of gestation Primigravida—A woman who is pregnant for the first time Primipara—A woman who has completed one pregnancy with a fetus or fetuses who have reached 20 weeks of gestation Term—A pregnancy from the beginning of week 38 of gestation to the end of week 42 of gestation Viability—The capacity to live outside the uterus; there are no clear limits of gestational age or weight. Infants born at 22 to 25 weeks of gestation are considered to be on the threshold of viability and are especially vulnerable to brain injury if they survive. Gravidity and parity information is obtained during history-taking interviews. Obtaining and documenting this information accurately is important in planning care for the pregnant woman. Two commonly used systems of summarizing the obstetric history are discussed here. Gravidity and parity can be described with only two digits: the first digit indicates the number of pregnancies the woman has had, including the present one, and parity the number of pregnancies that have reached 20 weeks of gestation. For example, the abbreviation gravida 1 para 0 (1/0) means that a woman is pregnant for the first time (primigravida) and has not carried a pregnancy to 20 weeks (nullipara). If a woman had twins at 36 weeks with her first pregnancy, she would also be gravida 1, para 1 (remember that para refers to pregnancies, not fetuses) (Cunningham, Leveno, Bloom, et al., 2010). Another system, consisting of five digits separated by hyphens, is commonly used in maternity centers. This system provides more information about the woman’s obstetric history, although it may not provide accurate information about parity since it provides information about births and not pregnancies reaching 20 weeks of gestation (Beebe, 2005). The first digit represents gravidity; the second digit represents the total number of term births; the third indicates the number of preterm births; the fourth identifies the number of abortions (miscarriage or elective termination of pregnancy); and the fifth is the number of children currently living. The acronym GTPAL (gravidity, term, preterm, abortions, living children) may be helpful in remembering this system of notation. For example, if a woman pregnant only once gives birth at week 35 and the infant survives, the abbreviation that represents this information is “1-0-1-0-1.” During her next pregnancy the abbreviation is “2-0-1-0-1.” Additional examples are in Table 7-1. TABLE 7-1 OBSTETRIC HISTORY USING FIVE-DIGIT AND TWO-DIGIT SYSTEM Early detection of pregnancy allows for early initiation of care. Human chorionic gonadotropin (hCG) is the earliest biologic marker for pregnancy. Pregnancy tests are based on the recognition of hCG or a beta (β) subunit of hCG. Production of β-hCG begins as early as the day of implantation and can be detected in maternal serum or urine as early as 7 to 8 days after ovulation. The level of hCG rises until it peaks at 60 to 70 days and then declines until about 16 weeks. Plasma levels of hCG remain at this lower level for the remainder of the pregnancy. Higher-than-normal levels of hCG are associated with abnormal gestation (e.g., fetus with Down syndrome, gestational trophoblastic disease) or multiple gestation. Abnormally slow increase in hCG or lower levels can indicate impending miscarriage or ectopic pregnancy (Cunningham, Leveno, Bloom, et al., 2010). Serum and urine pregnancy tests are performed in clinics, offices, women’s health centers, and laboratory settings. Urine pregnancy tests may be performed at home (see Community Focus box). Both serum and urine tests can provide accurate results. A 7- to 10-mL sample of venous blood is collected for serum testing. Most urine tests require a first-voided morning urine specimen because it contains levels of hCG approximately the same as those in serum. Random urine samples usually have lower levels. Urine tests are less expensive and provide more immediate results than serum tests. Many different pregnancy tests are available (Fig. 7-1). The wide variety of tests precludes discussion of each. The nurse should read the manufacturer’s directions for the test to be used and determine if the woman understands the directions. A study by Wallace, Zite, and Homewood (2009) reported that instructions for most home pregnancy tests do not comply with the recommended guidelines for use of plain language and that most instructions were written at a seventh-grade level or above. Enzyme-linked immunosorbent assay (ELISA) testing is the most popular method of testing for pregnancy. It uses a specific monoclonal antibody (anti-hCG) with enzymes that bond with hCG in urine. ELISA technology is the basis for most over-the-counter home pregnancy tests. With these one-step tests, the woman usually applies urine to a strip or absorbent-tipped applicator and reads the results. The test kits come with directions for collection of the specimen, the testing procedure, and reading of results. A positive test result is indicated by a simple color change reaction or a digital reading. Most manufacturers of the kits provide a toll-free telephone number to call if users have concerns and questions about test procedures or results. A common error in performing home pregnancy tests is doing the test too early in pregnancy before a significant rise in hCG level; this can cause a false negative result (Pagana and Pagana, 2011). Interpreting the results of pregnancy tests requires some judgment. The type of pregnancy test and its degree of sensitivity (the ability to detect low levels of a substance) and specificity (the ability to discern the absence of a substance) must be considered in conjunction with the woman’s history. This includes the date of her last normal menstrual period, her usual cycle length, and results of previous pregnancy tests. It is important to know if the woman abuses substances and what medications she is taking. Medications such as anticonvulsants and tranquilizers can cause false-positive results, whereas diuretics and promethazine can cause false-negative results (Pagana and Pagana, 2011). Improper collection of the specimen, hormone-producing tumors, and laboratory errors can also cause inaccurate results. Women who use a home pregnancy test should be advised about the variations in accuracy and to use caution when interpreting results. Whenever there is any question, further evaluation or retesting may be appropriate (see Patient Teaching box). Maternal physiologic adaptations are attributed to the hormones of pregnancy and to mechanical pressures arising from the enlarging uterus and other tissues. These adaptations protect the woman’s normal physiologic functioning, meet the metabolic demands that pregnancy imposes on her body, and provide a nurturing environment for fetal development and growth (see Critical Thinking Case Study). Although pregnancy is a normal phenomenon, problems can occur. • Presumptive—those changes felt by the woman (e.g., amenorrhea, fatigue, breast changes) • Probable—those changes observed by an examiner (e.g., Hegar sign, ballottement, pregnancy tests) • Positive—those signs attributed only to the presence of the fetus (e.g., hearing fetal heart tones, visualizing the fetus, palpating fetal movements) Table 7-2 summarizes these signs of pregnancy in relation to when they might occur and gives other possible causes for their occurrence. TABLE 7-2 The pregnancy may “show” after the fourteenth week, although this depends to some degree on the woman’s height and weight. Abdominal enlargement may be less apparent in the nullipara with good abdominal muscle tone (Fig. 7-2). Posture also influences the type and degree of abdominal enlargement that occurs. In normal pregnancies, the uterus enlarges at a predictable rate. As the uterus grows, it may be palpated above the symphysis pubis sometime between the twelfth and fourteenth weeks of pregnancy (Fig. 7-3). The uterus rises gradually to the level of the umbilicus at 22 to 24 weeks of gestation and nearly reaches the xiphoid process at term. Between weeks 38 and 40, fundal height decreases as the fetus begins to descend and engage in the pelvis (lightening) (see Fig. 7-3, dashed line). Generally, lightening occurs in the nullipara about 2 weeks before the onset of labor and in the multipara at the start of labor. Uterine enlargement is determined by measuring fundal height (see Fig. 8-7). This measurement is commonly used to estimate the duration of pregnancy. However, variation in the position of the fundus or the fetus, variations in the amount of amniotic fluid present, the presence of more than one fetus, maternal obesity, and variation in examiner technique can reduce the accuracy of this estimation. Generally the uterus rotates to the right as it elevates, probably because of the presence of the rectosigmoid colon on the left side. However, the extensive hypertrophy (enlargement) of the round ligaments keeps the uterus in the midline. Eventually the growing uterus touches the anterior abdominal wall and displaces the intestines to either side of the abdomen (Fig. 7-4). When a pregnant woman is standing, most of her uterus rests against the anterior abdominal wall and contributes to altering her center of gravity. At approximately 6 weeks of gestation, softening and compressibility of the lower uterine segment (uterine isthmus) occurs (Hegar sign) (Fig. 7-5). This results in exaggerated uterine anteflexion during the first 3 months of pregnancy. In this position, the uterine fundus presses on the urinary bladder, causing the woman to have urinary frequency. Placental perfusion depends on the maternal blood flow to the uterus. Blood flow increases rapidly as the uterus increases in size. Although uterine blood flow increases twentyfold, the fetoplacental unit grows even more rapidly. Consequently, more oxygen is extracted from the uterine blood during the latter part of pregnancy (Cunningham, Leveno, Bloom, et al., 2010). In a normal term pregnancy, one sixth of the total maternal blood volume is within the uterine vascular system. The rate of blood flow through the uterus averages 450 to 650 mL/min at term, and oxygen consumption of the gravid uterus increases to meet fetal needs. Three factors known to decrease uterine blood flow are low maternal arterial pressure, contractions of the uterus, and maternal supine position. Estrogen stimulation may increase uterine blood flow. Doppler ultrasound examination can be used to measure uterine blood flow velocity, especially in pregnancies at risk because of conditions associated with decreased placental perfusion (e.g., hypertension, intrauterine growth restriction, diabetes mellitus, multiple gestation) (Blackburn, 2013). Using an ultrasound device or a fetal stethoscope, the examiner may hear the uterine souffle or bruit, a rushing or blowing sound of maternal blood flowing through uterine arteries to the placenta that is synchronous with the maternal pulse. The funic souffle, which is synchronous with the fetal heart rate and is caused by fetal blood coursing through the umbilical cord, may also be heard, as well as the actual heartbeat of the fetus (see Fig. 8-8). Pregnancy can also cause the squamocolumnar junction, the site for obtaining cells for cervical cancer screening, to be located away from the cervix. Because of these changes, evaluation of abnormal Papanicolaou (Pap) tests during pregnancy can be complicated. However, careful assessment of all pregnant women is important because approximately 3% of all invasive cervical cancers occur during pregnancy (Salani, Eisenhauer, and Copeland, 2012). The cervix of the nullipara is rounded. Lacerations of the cervix almost always occur during the birth process. After childbirth, with or without lacerations, the cervix becomes more oval in the horizontal plane and the external os appears as a transverse slit (see Fig. 7-2). Pregnancy hormones prepare the vagina for stretching during labor and birth by causing the vaginal mucosa to thicken, the connective tissue to loosen, the smooth muscle to hypertrophy, and the vaginal vault to lengthen. Increased vascularity results in a violet-bluish color of the vaginal mucosa and cervix. The deepened color, termed Chadwick sign, can be evident as early as the sixth week but is easily noted by the eighth week of pregnancy (Blackburn, 2013). Leukorrhea is a white or slightly gray mucoid discharge with a faint musty odor. This copious mucoid fluid occurs in response to cervical stimulation by estrogen and progesterone. The fluid is whitish because of the presence of many exfoliated vaginal epithelial cells caused by the hyperplasia of normal pregnancy. This vaginal discharge is never pruritic or blood stained. The mucus fills the endocervical canal, resulting in the formation of the mucus plug (operculum) (Fig. 7-6). The operculum acts as a barrier against bacterial invasion during pregnancy. During pregnancy, the pH of vaginal secretions is more acidic, ranging from about 3.5 to about 6.0 (nonpregnant, 4.0 to 5.0), because of increased production of lactic acid (Cunningham, Leveno, Bloom, et al., 2010). Although this acidic environment provides more protection from some organisms, the pregnant woman is more vulnerable to other infections, especially yeast infections, because the glycogen-rich environment of the vagina is more susceptible to Candida albicans (Duff, Sweet, and Edwards, 2009). External structures of the perineum are enlarged during pregnancy because of an increase in vasculature, hypertrophy of the perineal body, and deposition of fat (Fig. 7-7). The labia majora of nullipara women approximate (come together) and obscure the vaginal introitus; those of the parous woman separate and gape after childbirth and perineal or vaginal injury. See Fig. 7-2 for a comparison of the nullipara and the multipara in relation to the pregnant abdomen, vulva, and cervix.
Anatomy and Physiology of Pregnancy
Gravidity and Parity
CONDITION
FIVE-DIGIT SYSTEM
TWO-DIGIT SYSTEM
G
T
P
A
L
G/P
GRAVIDITY
TERM BIRTH
PRETERM BIRTHS
ABORTIONS AND MISCARRIAGES
LIVING CHILDREN
GRAVIDITY/PARITY
Olivia is pregnant for the first time.
1
0
0
0
0
1/0
She carries the pregnancy to term, and the neonate survives.
1
1
0
0
1
1/1
She is pregnant again.
2
1
0
0
1
2/1
Her second pregnancy ends in miscarriage at 10 wk.
2
1
0
1
1
2/1
During her third pregnancy, she gives birth at 36 wk to twins.
3
1
2
1
3
3/2
Pregnancy Tests

Adaptations to Pregnancy
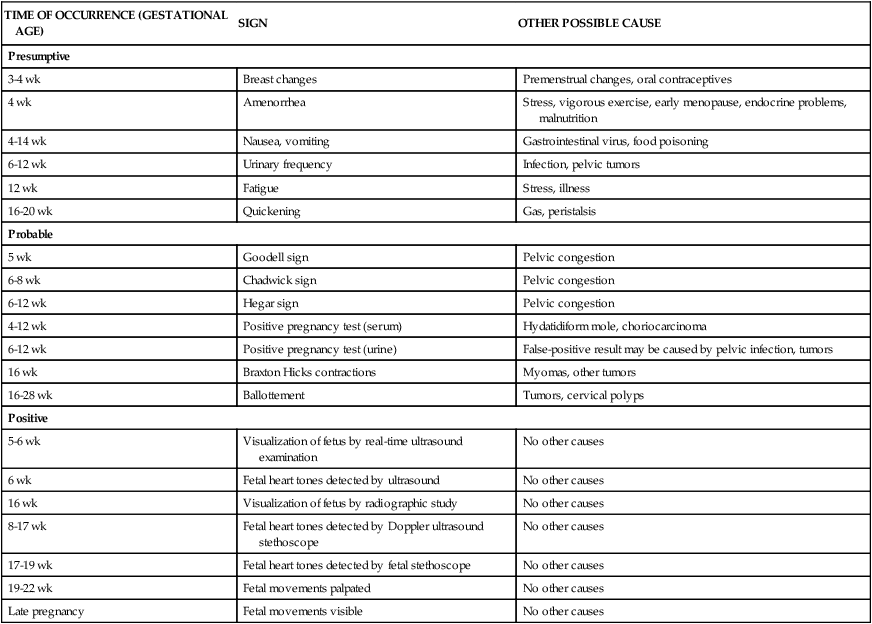
Signs of Pregnancy
TIME OF OCCURRENCE (GESTATIONAL AGE)
SIGN
OTHER POSSIBLE CAUSE
Presumptive
3-4 wk
Breast changes
Premenstrual changes, oral contraceptives
4 wk
Amenorrhea
Stress, vigorous exercise, early menopause, endocrine problems, malnutrition
4-14 wk
Nausea, vomiting
Gastrointestinal virus, food poisoning
6-12 wk
Urinary frequency
Infection, pelvic tumors
12 wk
Fatigue
Stress, illness
16-20 wk
Quickening
Gas, peristalsis
Probable
5 wk
Goodell sign
Pelvic congestion
6-8 wk
Chadwick sign
Pelvic congestion
6-12 wk
Hegar sign
Pelvic congestion
4-12 wk
Positive pregnancy test (serum)
Hydatidiform mole, choriocarcinoma
6-12 wk
Positive pregnancy test (urine)
False-positive result may be caused by pelvic infection, tumors
16 wk
Braxton Hicks contractions
Myomas, other tumors
16-28 wk
Ballottement
Tumors, cervical polyps
Positive
5-6 wk
Visualization of fetus by real-time ultrasound examination
No other causes
6 wk
Fetal heart tones detected by ultrasound
No other causes
16 wk
Visualization of fetus by radiographic study
No other causes
8-17 wk
Fetal heart tones detected by Doppler ultrasound stethoscope
No other causes
17-19 wk
Fetal heart tones detected by fetal stethoscope
No other causes
19-22 wk
Fetal movements palpated
No other causes
Late pregnancy
Fetal movements visible
No other causes
Reproductive System and Breasts
Uterus
Changes in Size, Shape, and Position.
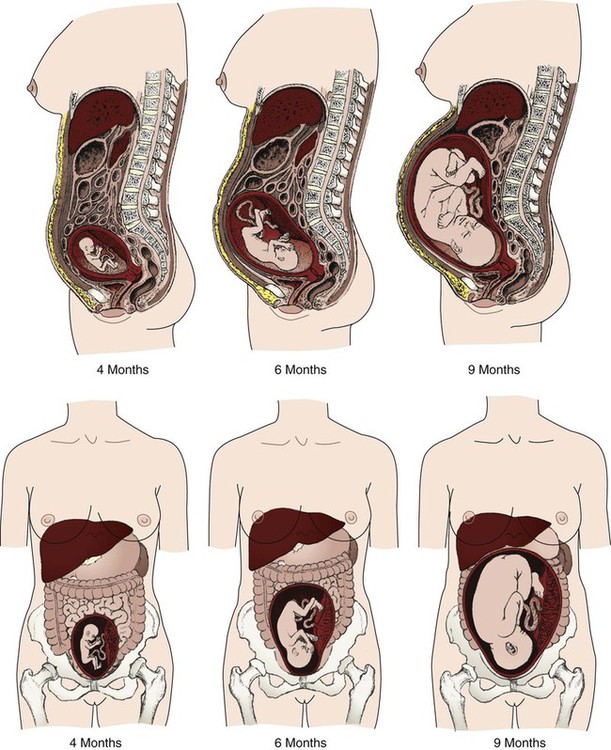
Uteroplacental Blood Flow.
Cervical Changes.
Vagina and Vulva
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Anatomy and Physiology of Pregnancy
Get Clinical Tree app for offline access