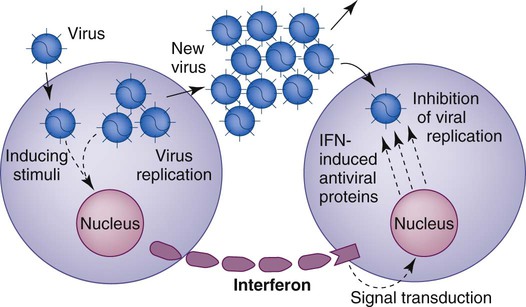
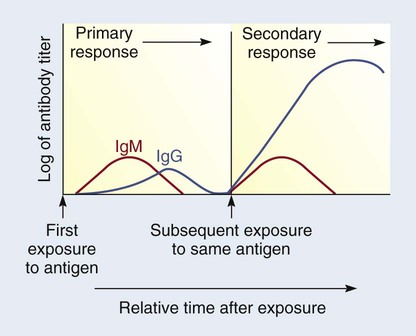
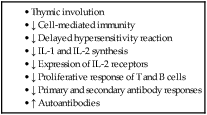
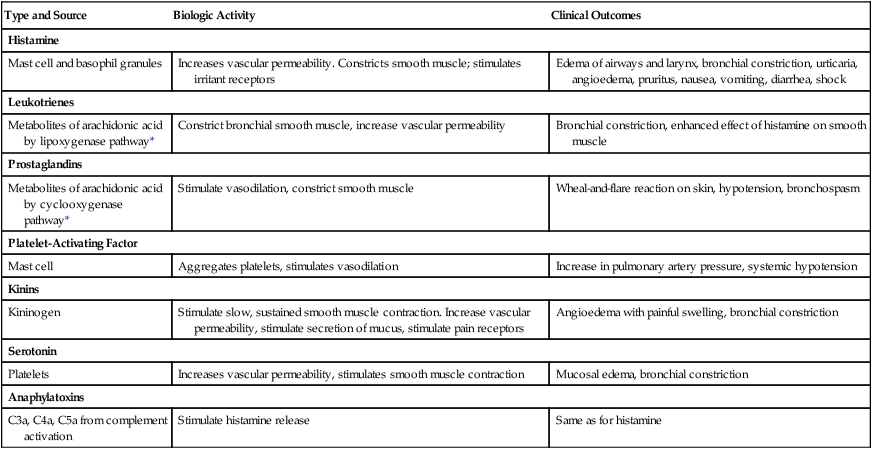
Chapter 14 1. Describe the functions and components of the immune system. 2. Compare and contrast humoral and cell-mediated immunity, including lymphocytes involved, types of reactions, and effects on antigens. 3. Characterize the five types of immunoglobulins. 4. Differentiate among the four types of hypersensitivity reactions in terms of immunologic mechanisms and resulting alterations. 5. Identify the clinical manifestations and emergency management of a systemic anaphylactic reaction. 6. Describe the assessment and collaborative care of a patient with chronic allergies. 7. Explain the relationship between the human leukocyte antigen system and certain diseases. 8. Describe the etiologic factors, clinical manifestations, and treatment modalities of autoimmune diseases. 9. Describe the etiologic factors and categories of immunodeficiency disorders. 10. Differentiate among the types of rejections following transplantation. 11. Identify the types and side effects of immunosuppressive therapy. 1. Defense: The body protects against invasions by microorganisms and prevents the development of infection by attacking foreign antigens and pathogens. 2. Homeostasis: Damaged cellular substances are digested and removed. Through this mechanism, the body’s different cell types remain uniform and unchanged. 3. Surveillance: Mutations continually arise in the body but are normally recognized as foreign cells and destroyed. eTABLE 14-1 eTABLE 14-2 Immunity is classified as innate or acquired. Acquired immunity is the development of immunity, either actively or passively (Table 14-1). TABLE 14-1 TYPES OF ACQUIRED SPECIFIC IMMUNITY The lymphoid system is composed of central (or primary) and peripheral lymphoid organs. The central lymphoid organs are the thymus gland and bone marrow. The peripheral lymphoid organs are the lymph nodes; tonsils; spleen; and gut-, genital-, bronchial-, and skin-associated lymphoid tissues (Fig. 14-1). The mononuclear phagocyte system includes monocytes in the blood and macrophages found throughout the body. Mononuclear phagocytes have a critical role in the immune system. They are responsible for capturing, processing, and presenting the antigen to the lymphocytes. This stimulates a humoral or cell-mediated immune response. Capturing is accomplished through phagocytosis. The macrophage-bound antigen, which is highly immunogenic, is presented to circulating T or B lymphocytes and thus triggers an immune response (Fig. 14-2). Lymphocytes are produced in the bone marrow (Fig. 14-3). They then differentiate into B and T lymphocytes.1 In the early research on B lymphocytes (bursa-equivalent lymphocytes) in birds, it was discovered that they mature under the influence of the bursa of Fabricius, hence the name B cells. However, this lymphoid organ does not exist in humans. The bursa-equivalent tissue in humans is the bone marrow. B cells differentiate into plasma cells when activated. Plasma cells produce antibodies (immunoglobulins) (Table 14-2). TABLE 14-2 CHARACTERISTICS OF IMMUNOGLOBULINS Dendritic cells make up a system of cells that are important to the immune system, especially the cell-mediated immune response. They have an atypical shape with extensive dendritic processes that form and retract. They are found in many places in the body, including the skin (where they are called Langerhans cells) and the lining of the nose, the lungs, the stomach, and the intestine. Especially in the immature state, they are found in the blood.2 Currently more than 100 different cytokines are known, and they can be classified into distinct categories. Some of these cytokines are listed in Table 14-3. In general, the interleukins act as immunomodulatory factors, colony-stimulating factors act as growth-regulating factors for hematopoietic cells, and interferons are antiviral and immunomodulatory. TABLE 14-3 TYPES AND FUNCTIONS OF CYTOKINES* NK, Natural killer; PMNs, polymorphonuclear neutrophils. *A more comprehensive presentation of cytokines is available at www.rndsystems.com/molecule_group.aspx?g=704&;r=4. The net effect of an inflammatory response is determined by a balance between proinflammatory and antiinflammatory mediators. Sometimes cytokines are classified as proinflammatory or antiinflammatory (see Table 14-3). However, it is not that clear-cut, since many other factors (e.g., target cells, environment) influence the inflammatory response to a given injury or insult. Cytokines have a beneficial role in hematopoiesis and immune function. They can also have detrimental effects such as those seen in chronic inflammation, autoimmune diseases, and sepsis. Cytokines such as erythropoietin (see Chapter 47), colony-stimulating factors (see Table 16-14), interferons (see Table 16-13), and interleukin-2 (see Table 16-13) are used clinically to (1) stimulate hematopoiesis, (2) stimulate the bone marrow to make WBCs, and (3) treat various malignancies. In addition, inhibitors of cytokines such as soluble tumor necrosis factor receptor antagonist and interleukin-1 are used as antiinflammatory agents. (Clinical uses of cytokines are listed in Table 14-4.) TABLE 14-4 *eFig. 14-1 on the website for this chapter shows how interferon is commercially made. Interferon helps the body’s natural defenses attack tumors and viruses. Three types of interferon have now been identified (see Table 14-3). In addition to their direct antiviral properties, interferons have immunoregulatory functions. These include enhancement of NK cell production and activation, and inhibition of tumor cell growth. Interferon is not directly antiviral but produces an antiviral effect in cells by reacting with them and inducing the formation of a second protein termed antiviral protein (Fig. 14-4). This protein mediates the antiviral action of interferon by altering the cell’s protein synthesis and preventing new viruses from becoming assembled. Humans need both humoral and cell-mediated immunity to remain healthy. Each type of immunity has unique properties, different methods of action, and reactions against particular antigens. Table 14-5 compares humoral and cell-mediated immunity. TABLE 14-5 COMPARISON OF HUMORAL AND CELL-MEDIATED IMMUNITY Humoral immunity consists of antibody-mediated immunity. The term humoral comes from the Greek word humor, which means body fluid. Since antibodies are produced by plasma cells (differentiated B cells) and found in plasma, the term humoral immunity is used. Production of antibodies is an essential component in a humoral immune response. Each of the five classes of immunoglobulins (Igs)—that is, IgG, IgA, IgM, IgD, and IgE—has specific characteristics (see Table 14-2). When a pathogen (especially bacteria) enters the body, it may encounter a B lymphocyte that is specific for antigens located on that bacterial cell wall. In addition, a monocyte or macrophage may phagocytize the bacteria and present its antigens to a B lymphocyte. The B lymphocyte recognizes the antigen because it has receptors on its cell surface specific for that antigen. When the antigen comes in contact with the cell surface receptor, the B cell becomes activated, and most B cells differentiate into plasma cells (see Fig. 14-3). The mature plasma cell secretes immunoglobulins. Some stimulated B lymphocytes remain as memory cells. The primary immune response becomes evident 4 to 8 days after the initial exposure to the antigen (Fig. 14-5). IgM is the first type of antibody formed. Because of the large size of the IgM molecule, this immunoglobulin is confined to the intravascular space. As the immune response progresses, IgG is produced, and it can move from intravascular to extravascular spaces. With advancing age, there is a decline in the function of the immune response (Table 14-6). The primary clinical evidence of immunosenescence is the high incidence of malignancies in older adults. Older people are also more susceptible to infections (e.g., influenza, pneumonia) from pathogens that they were relatively immunocompetent against earlier in life. Bacterial pneumonia is the leading cause of death from infections in older adults. The antibody response to immunizations (e.g., flu vaccine) in older adults is considerably lower than in younger adults. Hypersensitivity reactions can be classified according to the source of the antigen, the time sequence (immediate or delayed), or the basic immunologic mechanisms causing the injury. Four types of hypersensitivity reactions exist (Table 14-7). Types I, II, and III are immediate and are examples of humoral immunity. Type IV is a delayed hypersensitivity reaction and is related to cell-mediated immunity. TABLE 14-7 TYPES OF HYPERSENSITIVITY REACTIONS Anaphylactic reactions are type I reactions that occur only in susceptible people who are highly sensitized to specific allergens. IgE antibodies, produced in response to the allergen, have a characteristic property of attaching to mast cells and basophils (Fig. 14-6; see Fig. 29-2). Within these cells are granules containing potent chemical mediators (histamine, serotonin, leukotrienes, eosinophil chemotactic factor of anaphylaxis [ECF-A], kinins, and bradykinin). (Chemical mediators of inflammation are discussed in Chapter 12 and Table 12-1.) On the first exposure to the allergen, IgE antibodies are produced and bind to mast cells and basophils. On any subsequent exposures, the allergen links with the IgE bound to mast cells or basophils and triggers degranulation of the cells and the release of chemical mediators from the granules. In this process the mediators that are released attack target tissues, causing clinical allergy symptoms. These effects include smooth muscle contraction, increased vascular permeability, vasodilation, hypotension, increased secretion of mucus, and itching. Fortunately, the mediators are short acting and their effects are reversible. (The mediators and their effects are summarized in Table 14-8.) TABLE 14-8 MEDIATORS OF ALLERGIC RESPONSE*
Altered Immune Responses and Transplantation
Normal Immune Response
Type and Source
Biologic Activity
Clinical Outcomes
Histamine
Mast cell and basophil granules
Increases vascular permeability. Constricts smooth muscle; stimulates irritant receptors
Edema of airways and larynx, bronchial constriction, urticaria, angioedema, pruritus, nausea, vomiting, diarrhea, shock
Leukotrienes
Metabolites of arachidonic acid by lipoxygenase pathway*
Constrict bronchial smooth muscle, increase vascular permeability
Bronchial constriction, enhanced effect of histamine on smooth muscle
Prostaglandins
Metabolites of arachidonic acid by cyclooxygenase pathway*
Stimulate vasodilation, constrict smooth muscle
Wheal-and-flare reaction on skin, hypotension, bronchospasm
Platelet-Activating Factor
Mast cell
Aggregates platelets, stimulates vasodilation
Increase in pulmonary artery pressure, systemic hypotension
Kinins
Kininogen
Stimulate slow, sustained smooth muscle contraction. Increase vascular permeability, stimulate secretion of mucus, stimulate pain receptors
Angioedema with painful swelling, bronchial constriction
Serotonin
Platelets
Increases vascular permeability, stimulates smooth muscle contraction
Mucosal edema, bronchial constriction
Anaphylatoxins
C3a, C4a, C5a from complement activation
Stimulate histamine release
Same as for histamine
Types of Immunity
Acquired Immunity.
Type
Natural
Artificial
Active
Natural contact with antigen through clinical infection (e.g., recovery from chickenpox, measles, mumps)
Immunization with antigen (e.g., immunization with live or killed vaccines)
Passive
Transplacental and colostrum transfer from mother to child (e.g., maternal immunoglobulins in neonate)
Injection of serum from immune human (e.g., injection of human gamma globulin)
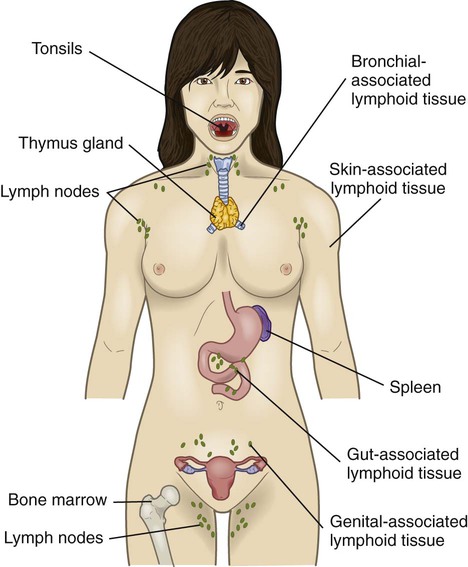
Lymphoid Organs
Cells Involved in Immune Response
Mononuclear Phagocytes.
Lymphocytes.
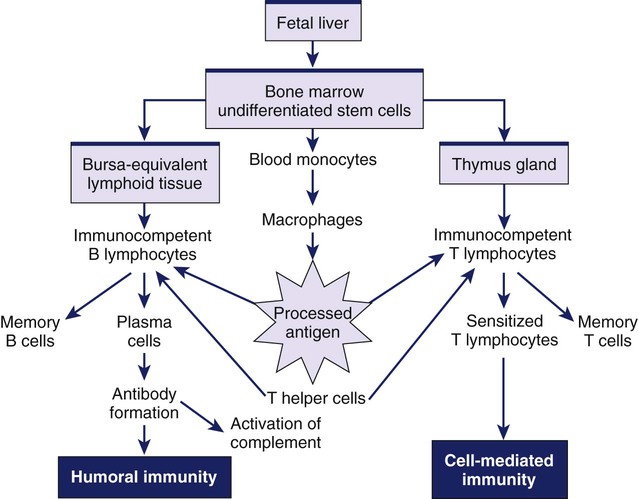
B Lymphocytes.
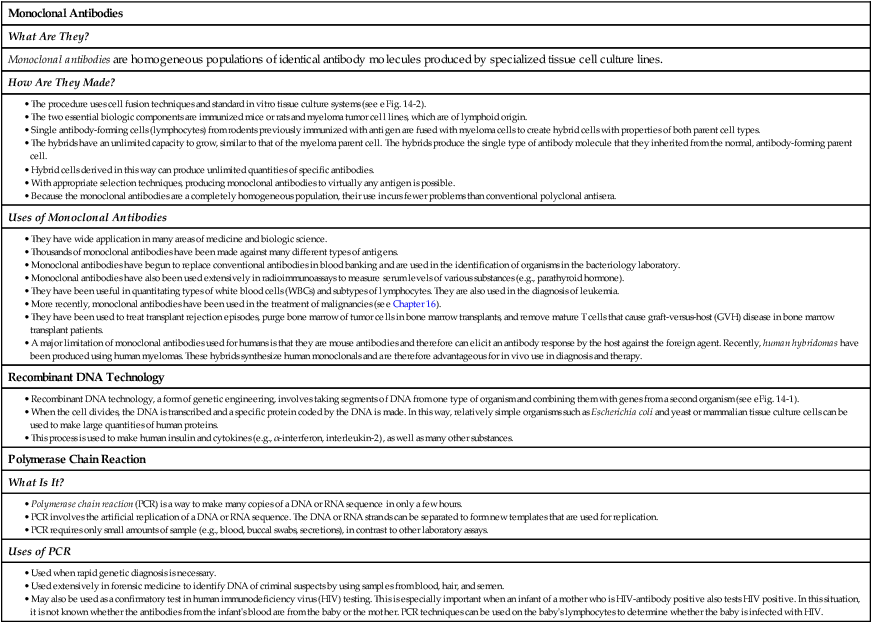
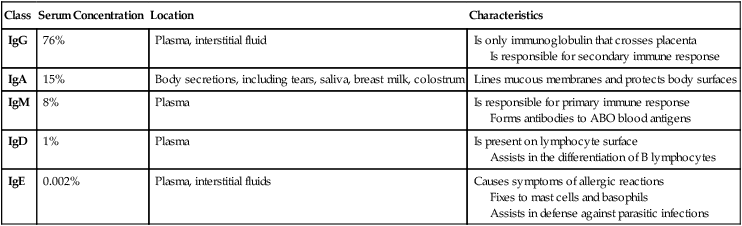
Class
Serum Concentration
Location
Characteristics
IgG
76%
Plasma, interstitial fluid
Is only immunoglobulin that crosses placenta
Is responsible for secondary immune response
IgA
15%
Body secretions, including tears, saliva, breast milk, colostrum
Lines mucous membranes and protects body surfaces
IgM
8%
Plasma
Is responsible for primary immune response
Forms antibodies to ABO blood antigens
IgD
1%
Plasma
Is present on lymphocyte surface
Assists in the differentiation of B lymphocytes
IgE
0.002%
Plasma, interstitial fluids
Causes symptoms of allergic reactions
Fixes to mast cells and basophils
Assists in defense against parasitic infections
Dendritic Cells.
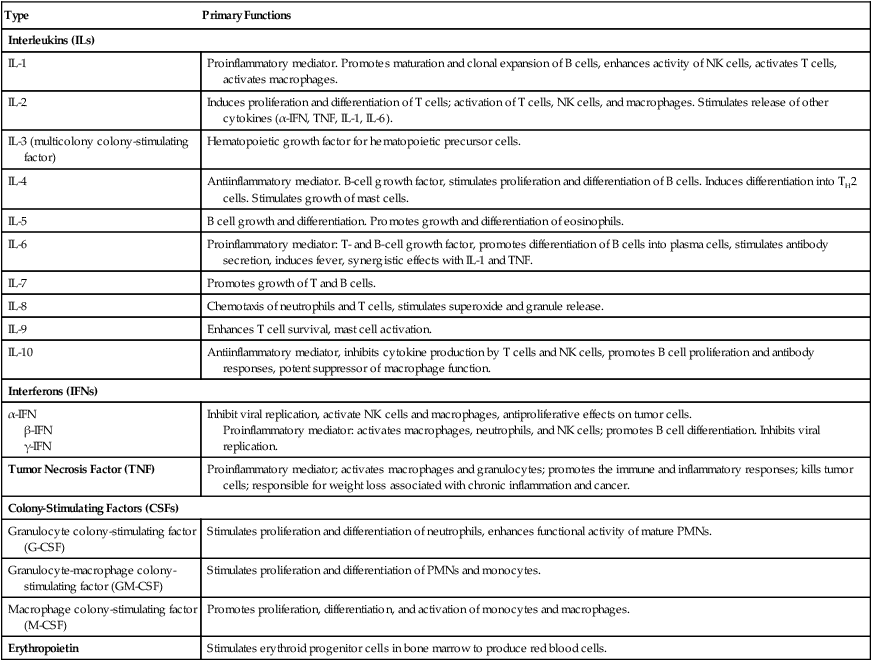
Cytokines
Type
Primary Functions
Interleukins (ILs)
IL-1
Proinflammatory mediator. Promotes maturation and clonal expansion of B cells, enhances activity of NK cells, activates T cells, activates macrophages.
IL-2
Induces proliferation and differentiation of T cells; activation of T cells, NK cells, and macrophages. Stimulates release of other cytokines (α-IFN, TNF, IL-1, IL-6).
IL-3 (multicolony colony-stimulating factor)
Hematopoietic growth factor for hematopoietic precursor cells.
IL-4
Antiinflammatory mediator. B-cell growth factor, stimulates proliferation and differentiation of B cells. Induces differentiation into TH2 cells. Stimulates growth of mast cells.
IL-5
B cell growth and differentiation. Promotes growth and differentiation of eosinophils.
IL-6
Proinflammatory mediator: T- and B-cell growth factor, promotes differentiation of B cells into plasma cells, stimulates antibody secretion, induces fever, synergistic effects with IL-1 and TNF.
IL-7
Promotes growth of T and B cells.
IL-8
Chemotaxis of neutrophils and T cells, stimulates superoxide and granule release.
IL-9
Enhances T cell survival, mast cell activation.
IL-10
Antiinflammatory mediator, inhibits cytokine production by T cells and NK cells, promotes B cell proliferation and antibody responses, potent suppressor of macrophage function.
Interferons (IFNs)
α-IFN
β-IFN
γ-IFN
Inhibit viral replication, activate NK cells and macrophages, antiproliferative effects on tumor cells.
Proinflammatory mediator: activates macrophages, neutrophils, and NK cells; promotes B cell differentiation. Inhibits viral replication.
Tumor Necrosis Factor (TNF)
Proinflammatory mediator; activates macrophages and granulocytes; promotes the immune and inflammatory responses; kills tumor cells; responsible for weight loss associated with chronic inflammation and cancer.
Colony-Stimulating Factors (CSFs)
Granulocyte colony-stimulating factor (G-CSF)
Stimulates proliferation and differentiation of neutrophils, enhances functional activity of mature PMNs.
Granulocyte-macrophage colony-stimulating factor (GM-CSF)
Stimulates proliferation and differentiation of PMNs and monocytes.
Macrophage colony-stimulating factor (M-CSF)
Promotes proliferation, differentiation, and activation of monocytes and macrophages.
Erythropoietin
Stimulates erythroid progenitor cells in bone marrow to produce red blood cells.
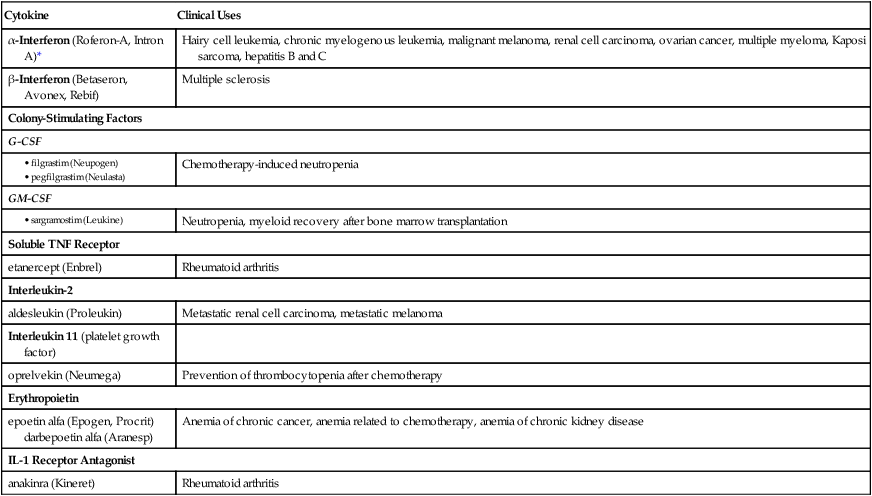
Cytokine
Clinical Uses
α-Interferon (Roferon-A, Intron A)*
Hairy cell leukemia, chronic myelogenous leukemia, malignant melanoma, renal cell carcinoma, ovarian cancer, multiple myeloma, Kaposi sarcoma, hepatitis B and C
β-Interferon (Betaseron, Avonex, Rebif)
Multiple sclerosis
Colony-Stimulating Factors
G-CSF
Chemotherapy-induced neutropenia
GM-CSF
Neutropenia, myeloid recovery after bone marrow transplantation
Soluble TNF Receptor
etanercept (Enbrel)
Rheumatoid arthritis
Interleukin-2
aldesleukin (Proleukin)
Metastatic renal cell carcinoma, metastatic melanoma
Interleukin 11 (platelet growth factor)
oprelvekin (Neumega)
Prevention of thrombocytopenia after chemotherapy
Erythropoietin
epoetin alfa (Epogen, Procrit)
darbepoetin alfa (Aranesp)
Anemia of chronic cancer, anemia related to chemotherapy, anemia of chronic kidney disease
IL-1 Receptor Antagonist
anakinra (Kineret)
Rheumatoid arthritis
Comparison of Humoral and Cell-Mediated Immunity
Characteristics
Humoral Immunity
Cell-Mediated Immunity
Cells involved
B lymphocytes
T lymphocytes, macrophages
Products
Antibodies
Sensitized T cells, cytokines
Memory cells
Present
Present
Protection
Bacteria
Viruses (extracellular)
Respiratory and GI pathogens
Fungus
Viruses (intracellular)
Chronic infectious agents
Tumor cells
Examples
Anaphylactic shock
Atopic diseases
Transfusion reaction
Bacterial infections
Tuberculosis
Fungal infections
Contact dermatitis
Graft rejection
Destruction of cancer cells
Humoral Immunity.
Gerontologic Considerations
Effects of Aging on the Immune System
Altered Immune Response
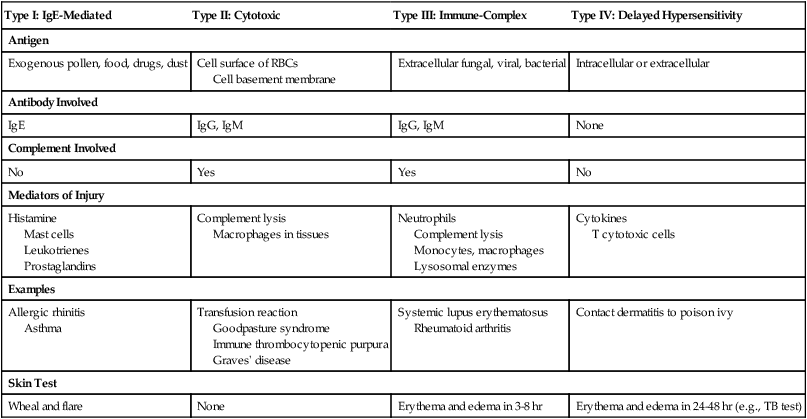
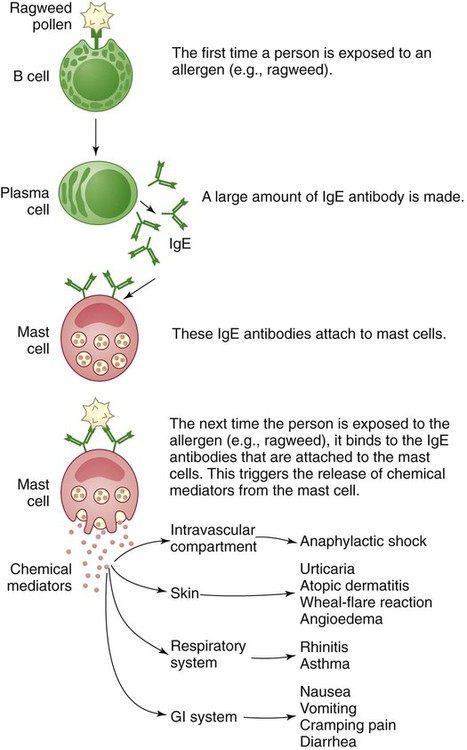
Hypersensitivity Reactions
Type I: IgE-Mediated
Type II: Cytotoxic
Type III: Immune-Complex
Type IV: Delayed Hypersensitivity
Antigen
Exogenous pollen, food, drugs, dust
Cell surface of RBCs
Cell basement membrane
Extracellular fungal, viral, bacterial
Intracellular or extracellular
Antibody Involved
IgE
IgG, IgM
IgG, IgM
None
Complement Involved
No
Yes
Yes
No
Mediators of Injury
Histamine
Mast cells
Leukotrienes
Prostaglandins
Complement lysis
Macrophages in tissues
Neutrophils
Complement lysis
Monocytes, macrophages
Lysosomal enzymes
Cytokines
T cytotoxic cells
Examples
Allergic rhinitis
Asthma
Transfusion reaction
Goodpasture syndrome
Immune thrombocytopenic purpura
Graves’ disease
Systemic lupus erythematosus
Rheumatoid arthritis
Contact dermatitis to poison ivy
Skin Test
Wheal and flare
None
Erythema and edema in 3-8 hr
Erythema and edema in 24-48 hr (e.g., TB test)
Type I: IgE-Mediated Reactions.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

Altered Immune Responses and Transplantation
Get Clinical Tree app for offline access