Alcohol, Tobacco, and Other Drug Problems
Objectives
After reading this chapter, the student should be able to do the following:
1. Analyze personal attitudes toward alcohol, tobacco, and other drug problems.
2. Differentiate among these terms: substance use, abuse, dependence, and addiction.
Key Terms
addiction treatment, p. 820
Alcoholics Anonymous (AA), p. 822
alcoholism, p. 808
biopsychosocial model, p. 813
blood alcohol concentration, p. 809
brief interventions, p. 814
codependency, p. 819
cross-tolerance, p. 821
denial, p. 815
depressants, p. 808
detoxification, p. 819
drug addiction, p. 808
drug dependence, p. 807
enabling, p. 819
fetal alcohol syndrome, p. 809
hallucinogens, p. 808
harm reduction, p. 807
injection drug users, p. 817
mainstream smoke, p. 811
polysubstance use or abuse, p. 813
prohibition, p. 805
psychoactive drugs, p. 807
set, p. 812
setting, p. 812
sidestream smoke, p. 811
stimulants, p. 808
substance abuse, p. 805
tolerance, p. 811
withdrawal, p. 808
—See Glossary for definitions
 Mary Lynn Mathre, RN, MSN, CARN
Mary Lynn Mathre, RN, MSN, CARN
Mary Lynn Mathre has 36 years of experience as an acute care nurse and has worked in the field of alcohol, tobacco, and other drugs for the past 25 years. From 1991 to 2003, she worked as the addictions consult nurse for the University of Virginia Health System. This role required much interaction with community resources to provide appropriate referrals and aftercare for the client population. From 2004 to 2007 she worked in an outpatient opioid treatment program as the executive director. Currently she works as an independent consultant on substance abuse prevention and brief interventions. She is an active member of the International Nurses Society on Addictions and serves on the editorial board for the Journal of Addictions Nursing.
Substance abuse is the number one national health problem, causing more deaths, illnesses, and disabilities than any other health condition. The substance abuser is not only at risk for personal health problems, but may also be a threat to the health and safety of family members, co-workers, and other members of the community.
Substance abuse and addiction affect all ages, races, sexes, and segments of society. As seen in Healthy People 2020 (USDHHS, 2010), tobacco use and substance abuse are two major topic areas, with many objectives and sub-objectives, as well as related objectives in other priority areas. The newer phrase of alcohol, tobacco, and other drug (ATOD) problems rather than substance abuse reminds us that alcohol and tobacco represent the major drugs of abuse when discussing substance abuse, drug addiction, or chemical dependency.
This chapter begins by providing a broad perspective of ATOD problems to clarify the relevant issues. A historical overview of ATOD problems and attitudes toward ATOD users and addicts is examined. Relevant terms are defined to decrease the confusion caused by frequent misuse of terms. The major drug categories are described, including information on commonly used substances and current ATOD use trends. The remainder of the chapter examines the role of the nurse in primary, secondary, and tertiary prevention and describes how the nurse can improve the outcomes for individuals, families, and various populations with ATOD problems when using a harm reduction model. The reader is encouraged to consider possible nursing strategies to apply the Healthy People 2020 objectives for ATOD problems.
Alcohol, Tobacco, and Other Drug Problems in Perspective
ATOD abuse and addiction can cause multiple health problems for individuals. Heavy ATOD use has been associated with many problems, including neonates with low birth weight and congenital abnormalities; accidents, homicides, and suicides; chronic diseases, such as cardiovascular diseases, cancer, lung disease, hepatitis, HIV/AIDS, and mental illness; violence; and family disruption. Factors that contribute to the substance abuse problem include lack of knowledge about the use of drugs; the war on drugs’ emphasis on illicit drugs and law enforcement rather than the prevention and treatment of abuse and addiction of ATODs; lack of quality control of illegal drugs; and drug laws that label certain drug users as criminals, which encourages the negative attitudes and stigma toward these persons.
Historical Overview
Psychoactive drug use has been part of most cultures since the beginning of humanity. Often a culture encourages use of some drugs while discouraging the use of others. Caffeine, alcohol, and tobacco are socially acceptable drugs in the United States and Canada, whereas other cultures prohibit their use. Conversely, marijuana, cocaine, and opium use are not accepted in mainstream U.S. society, although these substances are considered sacred or beneficial and their use is accepted in various other cultures.
The United States’ primary solution to various “drug problems” has been prohibition. During alcohol prohibition from 1920 to 1933, the United States experienced a sharp increase in violent crime and corruption among law officials as a result of the illicit marketing of alcohol. Distilled beverages were pushed because of the higher profit margin per bottle of liquor than for beer or wine. The high alcohol content in illicit moonshine caused severe health problems. The alcohol prohibition was eventually recognized as a failure and repealed (Rose, 1996).
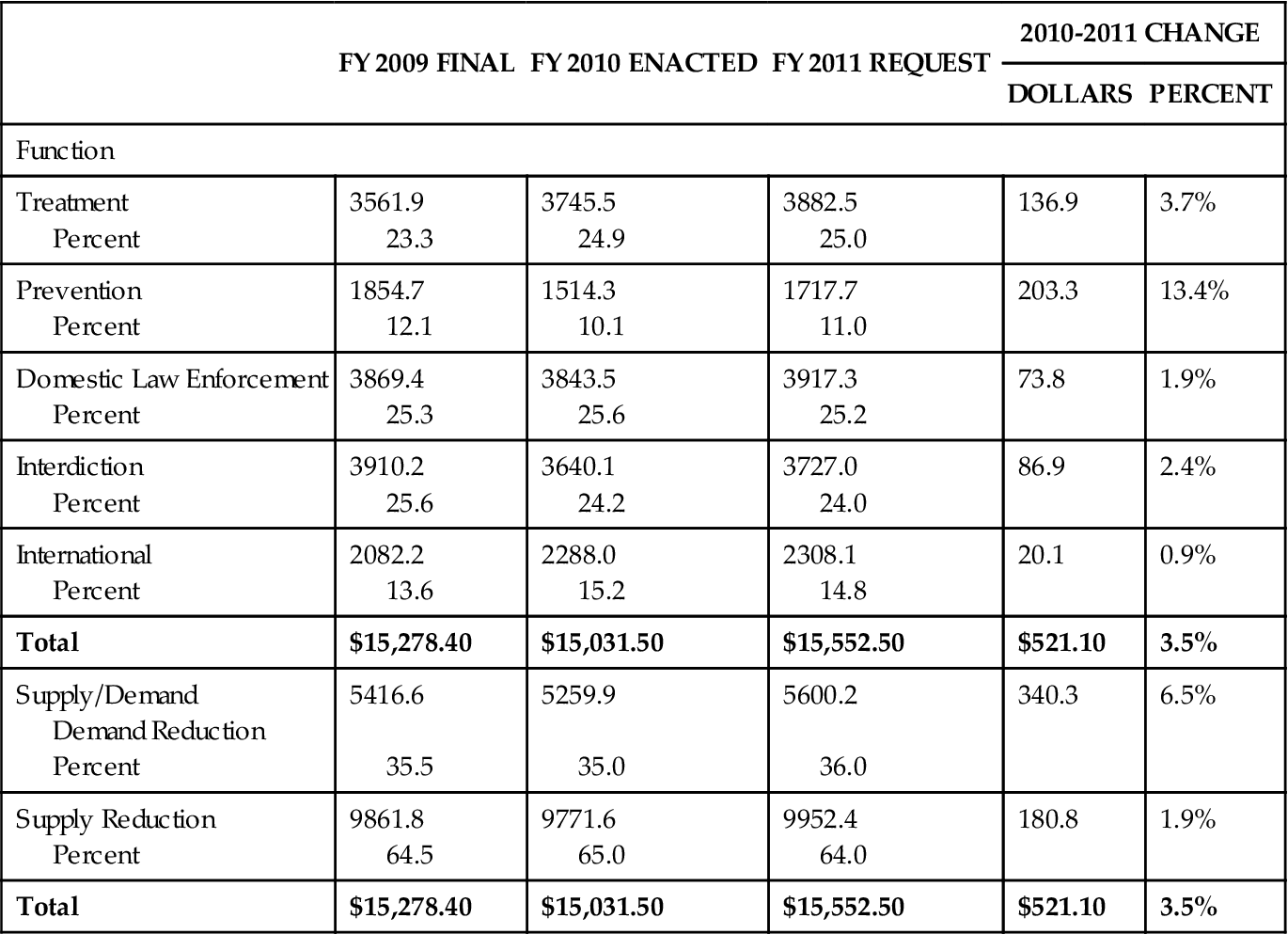
Similar problems are occurring with the current war on drugs and the newer prohibition on marijuana, cocaine, and other drugs. An increase in both violent crime and reports of corruption among law officials as a result of the illicit market has become a major national problem (Common Sense for Drug Policy, 2007). Stronger drugs are pushed because of their greater profits. Some would say that drug prohibition laws have created mandatory sentences for drug offenders, violated civil liberties, and put more resources into law enforcement than into drug education and treatment (Common Sense for Drug Policy, 2007). As the drug war budget grows each year, most of that budget goes to law enforcement and punishment, leaving only a third for prevention and treatment. See Table 37-1 for a historical overview of the drug war budget.
TABLE 37-1
FEDERAL DRUG CONTROL SPENDING BY FUNCTION
| FY 2009 FINAL | FY 2010 ENACTED | FY 2011 REQUEST | 2010-2011 CHANGE | ||
| DOLLARS | PERCENT | ||||
| Function | |||||
| Treatment Percent | 3561.9 23.3 | 3745.5 24.9 | 3882.5 25.0 | 136.9 | 3.7% |
| Prevention Percent | 1854.7 12.1 | 1514.3 10.1 | 1717.7 11.0 | 203.3 | 13.4% |
| Domestic Law Enforcement Percent | 3869.4 25.3 | 3843.5 25.6 | 3917.3 25.2 | 73.8 | 1.9% |
| Interdiction Percent | 3910.2 25.6 | 3640.1 24.2 | 3727.0 24.0 | 86.9 | 2.4% |
| International Percent | 2082.2 13.6 | 2288.0 15.2 | 2308.1 14.8 | 20.1 | 0.9% |
| Total | $15,278.40 | $15,031.50 | $15,552.50 | $521.10 | 3.5% |
| Supply/Demand Demand Reduction Percent | 5416.6 35.5 | 5259.9 35.0 | 5600.2 36.0 | 340.3 | 6.5% |
| Supply Reduction Percent | 9861.8 64.5 | 9771.6 65.0 | 9952.4 64.0 | 180.8 | 1.9% |
| Total | $15,278.40 | $15,031.50 | $15,552.50 | $521.10 | 3.5% |
A 3-year study by the National Center on Addiction and Substance Abuse (CASA) closely examined the 2005 federal, state, and local government budgets to measure the financial impact of ATOD problems on their health, social service, criminal justice, education, mental health, developmentally disabled, and other programs. The CASA study found that the government spent at least $467.7 billion ($238.2 billion, federal; $135.8 billion, state; and $93.8 billion, local) in 2005 on substance abuse and addiction, which amounted to 10.7% of the entire $4.4 trillion budgets. Of every dollar the federal and state governments spent on substance abuse and addiction, 95.6 cents was used to deal with the ATOD problems, while only 1.9 cents went to prevention and treatment, 0.4% to research, 1.4% to taxation or regulation, and 0.7% to interdiction. Almost half of this spending cannot be disaggregated by specific substance. However, of the $248 billion in ATOD-related spending, 92.3% was linked to alcohol and tobacco (National Center on Addiction and Substance Abuse, 2009).
Attitudes and Myths
Attitudes are developed through cultural learning and personal experiences. Attitudes toward ATOD problems are influenced by the way society inappropriately categorizes drugs as either “good” or “bad.” In the United States, good drugs are typically over-the-counter (OTC) or those prescribed by a health care provider as medicine, yet this makes them no less problematic or addictive. Bad drugs are the illegal drugs, and persons who use these drugs are considered criminals regardless of whether the drug has caused any problems.
Americans rely heavily on prescription and OTC drugs to relieve (or mask) anxiety, tension, fatigue, and physical or emotional pain. Rather than learning non-medicinal methods of coping, many people rely on the “quick fix” and take pills to deal with their problems or negative feelings.
Addicts are often viewed as immoral, weak-willed, or irresponsible persons who should try harder to help themselves. Although alcoholism was recognized as a disease by the American Medical Association in 1954, and drug addiction was recognized as a disease some years later, much of the public and many health care professionals have failed to change their attitudes and accept alcoholics and addicts as ill persons in need of health care.
Nurses must examine their attitudes toward ATOD use, abuse, and addiction before working with this health problem. To be therapeutic, the nurse must develop a trusting, non-judgmental relationship with the client. Systematic assessment for ATOD problems is based on awareness that there may be problems with both legal and illegal drugs. If the nurse’s attitude toward a client with a drug abuse problem is negative or punitive, the issue may never be directly addressed or the client may be avoided. If the client senses the negative attitude of the health care provider, either by words or from tone of voice, communication may cease and information may be withheld. To develop a therapeutic attitude, the nurse must realize that any drug can be abused, that anyone may develop drug dependence, and that drug addiction can be successfully treated.
Myths develop over years, and if myths are not questioned, many attitudes may be formed solely on the basis of fiction rather than fact. Some common myths are as follows:
• “An alcoholic is a skid row bum”—but less than 5% of persons with addictions fit this description.
Paradigm Shift
We can hope to see a major shift in how the United States conceptualizes ATOD problems. The old criminal justice model is based on stereotypes, misinformation, and punishment, and it uses war tactics to fight the drug users, addicts, and suppliers. Campaigns have been launched using the slogans “zero tolerance” for drug users, “just say no” to drugs, and striving for a “drug-free America”—all of which vilify the drug user or drug addict. Gil Kerlikowske, the drug czar in the Obama administration, has said that he wants to move away from the “war on drugs” approach and that the Obama administration is likely to deal with drugs as a matter of public health rather than criminal justice alone, with the role of treatment growing relative to incarceration (Fields, 2009). Also, on the international level, experts are suggesting that national drug policies need to be more comprehensive rather than focusing on law enforcement strategies (Box 37-1).
The harm reduction model is a public health approach to ATOD problems initially used in Great Britain, The Netherlands, Germany, Switzerland, and Australia, and interest in it is spreading throughout Europe and in Canada. This new public health model recognizes the following:
• Addiction is a health problem.
• Any psychoactive drug can be abused.
• Accurate information can help people make responsible decisions about drug use.
This approach accepts the reality that psychoactive drug use is endemic, and it focuses on pragmatic interventions, especially education, to reduce the adverse consequences of drug abuse and get treatment for addicts. The United States has already taken a harm reduction approach with tobacco and alcohol. Educational campaigns are used to inform the public about the health risks of tobacco use. Warnings have appeared on tobacco product labels since 1967 as a result of the surgeon general’s 1966 report on the dangers of smoking. In 1971 a ban on television and radio cigarette advertising was imposed. Cigarette smoking has decreased since that time. Smoking is on the decline among eighth and twelfth graders. According to the 2007 report from Monitoring the Future drug survey data among secondary school students, 4% of eighth graders smoked in 2006, down from 5.5% in 2001. For twelfth graders in 2006, 12% smoked compared with 19% in 2001 (Johnston, O’Malley, and Bachman, 2007). Education is continuing to address the dangers of alcohol abuse and to establish guidelines for safe alcohol use.
Nurses need to seek the underlying roots of various health problems and plan action that is realistic, non-judgmental, holistic, and positive. A harm reduction model for ATOD problems facilitates such an approach.
Definitions
The terms drug use and drug abuse have virtually lost their usefulness because the public and government have narrowed the term drug to include only illegal drugs rather than including prescription, OTC, and legal recreational drugs. The current phrase alcohol, tobacco, and other drugs (ATODs) is a reminder that the leading drug problems involve alcohol and tobacco. The term substance broadens the scope to include alcohol, tobacco, legal drugs, and even foods. Substance abuse is the use of any substance that threatens a person’s health or impairs social or economic functioning. This definition is more objective and universal than the government’s definition of drug abuse, which is the use of a drug without a prescription or any use of an illegal drug. Although any drug or food can be abused, this chapter focuses on psychoactive drugs—drugs that affect mood, perception, and thought.
Drug dependence and drug addiction are often used interchangeably, but they are not synonymous. Drug dependence is a state of neuroadaptation (a physiological change in the central nervous system [CNS]) caused by the chronic, regular administration of a drug; in drug dependence, continued use of the drug becomes necessary to prevent withdrawal symptoms. For example, when a person is given an opiate such as morphine on a regular basis for pain management, the morphine needs to be gradually tapered rather than abruptly stopped to prevent symptoms of withdrawal.
Drug addiction is a pattern of abuse characterized by an overwhelming preoccupation with the use (compulsive use) of a drug, securing its supply, and a high tendency to relapse if the drug is removed. Frequently, addicts are physically dependent on a drug, but there also appears to be an added psychological component that causes the intense cravings and subsequent relapse. In general, anyone can develop drug dependence as a result of regular administration of drugs that alter the CNS; however, only 7% to 15% of the drug-using population will develop a drug addiction. The process of becoming addicted is complex and related to several factors, including the addictive properties of the substance, family and peer influences, personality, age of first use, cultural and social factors, existing psychiatric disorders, and genetics.
Alcoholism is addiction to the drug called alcohol. Alcoholism and drug addiction are recognized as illnesses under a biopsychosocial model. Simply stated, the disease concept of addiction and alcoholism identifies them as chronic and progressive diseases in which a person’s use of a drug or drugs continues despite problems it causes in any area of life—physical, emotional, social, economic, or spiritual.
Psychoactive Drugs
Although any drug can be abused, ATOD abuse and addiction problems generally involve the psychoactive drugs. These drugs, which can alter emotions, are used for enjoyment in social and recreational settings and for personal use to self-medicate physical or emotional discomfort. Psychoactive drugs are divided into categories according to their effect on the CNS and the general feelings or experiences the drugs may induce. The Internet or a pharmacology text can provide detailed information on these drug categories (e.g., depressants, stimulants [Box 37-2], hallucinogens, inhalants [Box 37-3] and marijuana), and a drug chart of commonly abused drugs is provided in the Evolve site for this book. This chapter focuses on alcohol, tobacco, and marijuana since alcohol and tobacco cause the greatest harm and marijuana is the most commonly used illicit drug. (Resource Tool 37.B on the Evolve website lists useful web resources with more information on handling substance abuse and addiction.)
Alcohol
Alcohol (ethyl alcohol or ethanol) is the oldest and most widely used psychoactive drug in the world. In 2006 a national survey found that young people between the ages of 12 and 20 are more likely to use alcohol than use tobacco or illicit drugs, including marijuana. Youth tend to drink less often than adults, but they consume more alcohol per occasion. On average, youth report consuming five drinks per occasion, and they increasingly binge drink. Alcohol abuse contributes to illness in each of the top three causes of death in the United States: heart disease, cancer, and stroke. In 2008, an estimated 22.2 million persons (8.9% of the population aged 12 or older) were classified with substance dependence or abuse in the past year based on criteria specified in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). Of these, 3.1 million were classified with dependence on or abuse of both alcohol and illicit drugs, 3.9 million were dependent on or abused illicit drugs but not alcohol, and 15.2 million were dependent on or abused alcohol but not illicit drugs (SAMHSA, 2009a).
Alcohol abuse costs billions of dollars in lost productivity, property damage, medical expenses from alcohol-related illnesses and accidents, family disruptions, alcohol-related violence, and neglect and abuse of children.
Chronic alcohol abuse leads to profound metabolic and physiological effects on all organ systems. Gastrointestinal (GI) disturbances include inflammation of the GI tract, malabsorption, ulcers, liver problems, and cancers. Cardiovascular disturbances include cardiac dysrhythmias, cardiomyopathy, hypertension, atherosclerosis, and blood dyscrasias. CNS problems include depression, sleep disturbances, memory loss, organic brain syndrome, Wernicke-Korsakoff syndrome, and alcohol withdrawal syndrome. Neuromuscular problems include myopathy and peripheral neuropathy. Males may experience testicular atrophy, sterility, impotence, or gynecomastia, and females who consume alcohol during pregnancy may reproduce neonates with fetal alcohol syndrome (FAS) or fetal alcohol effects (FAE). Some of the metabolic disturbances include hypokalemia, hypomagnesemia, and ketoacidosis. Also, endocrine disturbances may result in pancreatitis or diabetes (Merck Manual, 2008).
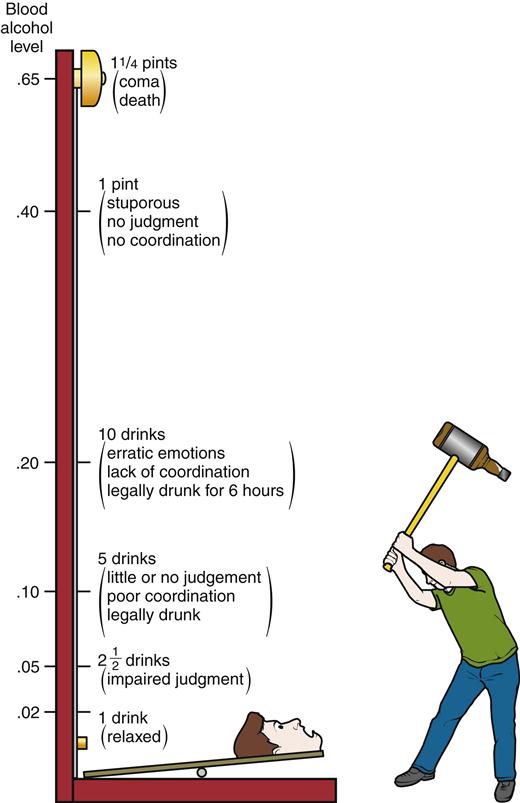
The concentration of alcohol in the blood is determined by the concentration of alcohol in the drink, the rate of drinking, the rate of absorption (slower in the presence of food), the rate of metabolism, and a person’s weight and sex. The amount of alcohol the liver can metabolize per hour is equal to about ¾ oz of whiskey, 4 oz of wine, or 12 oz of beer. Figure 37-1 shows the effects on the CNS as the blood alcohol concentration (BAC) increases. However, with chronic consumption, tolerance will develop, and a person can reach a high BAC with minimal CNS effects.
Alcohol use in moderation may provide health benefits by providing mild relaxation and lowering the serum cholesterol level. Controlled drinking organizations such as Moderation Management (http://www.moderation.org) provide guidelines for persons who want to have alcohol in their lives. See Box 37-4 for safe limits of alcohol consumption and Table 37-2 for standard drink equivalents.
TABLE 37-2
| A standard drink in the United States is any drink that contains about 14 g of pure alcohol (about 0.6 fluid oz or 1.2 tbsp). The U.S. standard drink equivalents shown here are approximate, since different brands and types of beverages vary in their actual alcohol content. | ||||||
| 12 oz of beer or cooler | 8-9 oz of malt liquor 8.5 oz shown in a 12-oz glass that, if full, would hold about 1.5 standard drinks of malt liquor | 5 oz of table wine | 3-4 oz of fortified wine (such as sherry or port) 3.5 oz shown | 2-3 oz of cordial, liqueur, or aperitif 2.5 oz shown | 1.5 oz of brandy (a single jigger) | 1.5 oz of spirits (a single jigger of 80-proof gin, vodka, whiskey, etc.) Shown straight and in a highball glass with ice to show level before adding mixer* |
12 oz  | 8.5 oz  | 5 oz  | 3.5 oz  | 2.5 oz  | 1.5 oz  | 1.5 oz  |
| Many people do not know what counts as a standard drink and so they do not realize how many standard drinks are in the containers in which these drinks are often sold. Some examples: | |
| • 12 oz = 1 | • 22 oz = 2 |
| • 16 oz = 1.3 | • 40 oz = 3.3 |
| • 12 oz = 1.5 | • 22 oz = 2.5 |
| • 16 oz = 2 | • 40 oz = 4.5 |
| • a standard 750 mL (25 oz) bottle = 5 | |
| • a mixed drink = 1 or more* | • a fifth (25 oz) = 17 |
| • a pint (16 oz) = 11 | • 1.75 L (59 oz) = 39 |
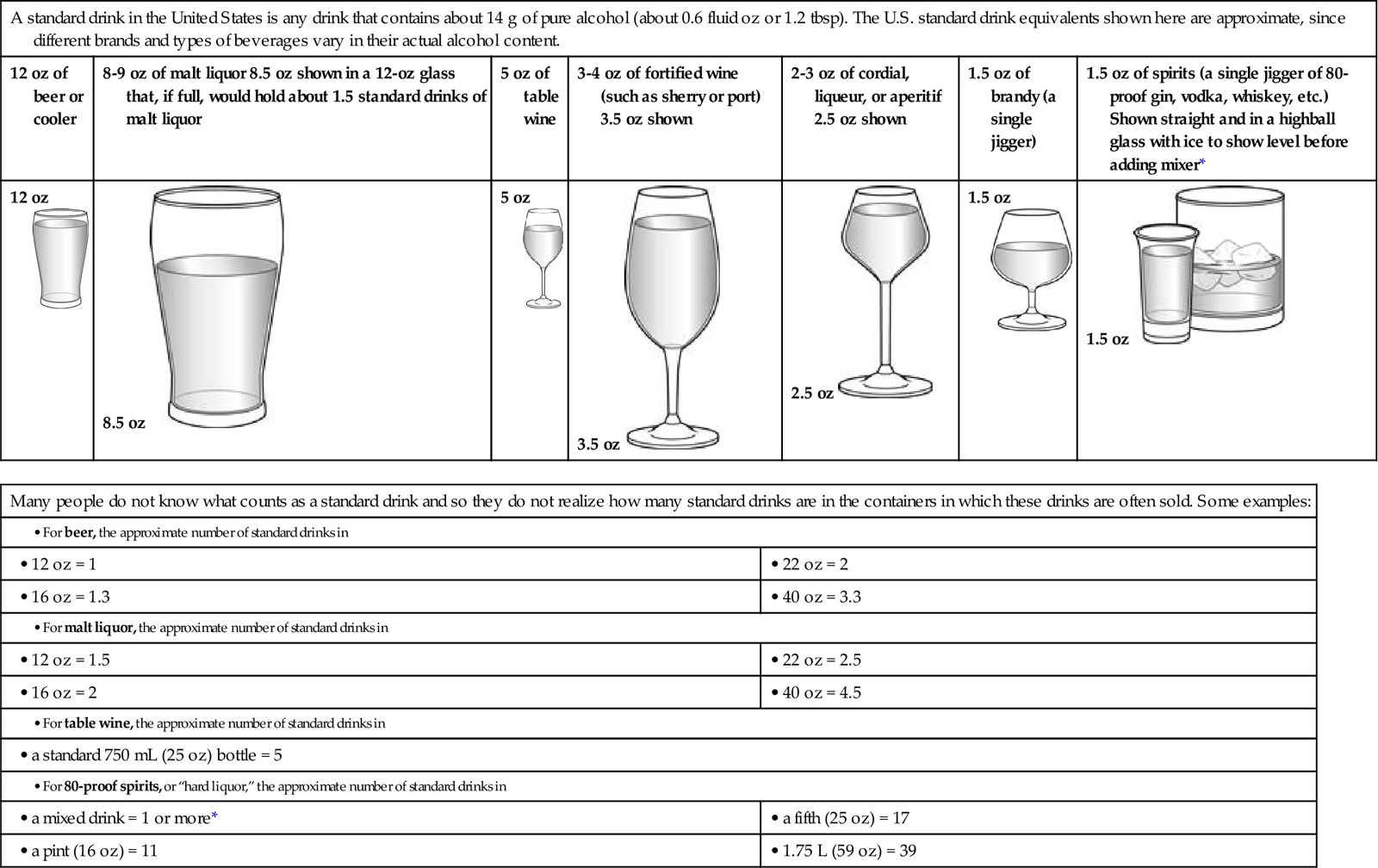
*Note: It can be difficult to estimate the number of standard drinks in a single mixed drink made with hard liquor. Depending on factors such as the type of spirits and the recipe, a mixed drink can contain from one to three or more standard drinks.
Tobacco
Smoking is the foremost preventable cause of death and disease in the United States, with one in five deaths attributed to cigarettes. For every person who dies from tobacco use, another 20 will suffer from at least one serious tobacco-related illness (CDC, 2010). Table 37-3 highlights cigarette smoking–related mortality in the United States. The Centers for Disease Control and Prevention (CDC) estimates an average of 443,000 deaths per year are caused by complications of cigarette smoking (CDC, 2008a). In 2008, an estimated 70.9 million Americans aged 12 or older were current (past month) users of a tobacco product. This represents 28.4% of the population in that age range. In addition, 59.8 million persons (23% of the population) were current cigarette smokers; 13.1 million (5.3%) smoked cigars; 8.7 million (3.5%) used smokeless tobacco; and 1.9 million (0.8%) smoked tobacco in pipes (SAMHSA, 2009a). Young adults ages 18 to 25 reported the highest rate of current tobacco use at 44.8% (NIDA, 2009b).
TABLE 37-3
CIGARETTE SMOKING–RELATED MORTALITY
| DISEASE | MEN | WOMEN | OVERALL |
| Cancers | |||
| Lung | 78,680 | 46,842 | 125,522 |
| Other | 25,792 | 9,534 | 35,326 |
| Subtotal | 104,472 | 56,376 | 160,848 |
| Cardiovascular Diseases | |||
| Heart disease | 63,878 | 37,181 | 101,059 |
| Stroke | 7,896 | 8,026 | 15,922 |
| Other | 7,415 | 4,151 | 11,566 |
| Subtotal | 79,139 | 49,358 | 128,497 |
| Respiratory Diseases | |||
| Pneumonia/influenza | 6,042 | 4,381 | 10,423 |
| Bronchitis/emphysema | 7,536 | 6,391 | 13,927 |
| Chronic airway obstruction | 40,217 | 38,771 | 78,988 |
| Subtotal | 53,795 | 49,543 | 103,338 |
| Total | 237,406 | 155,277 | 392,683 |
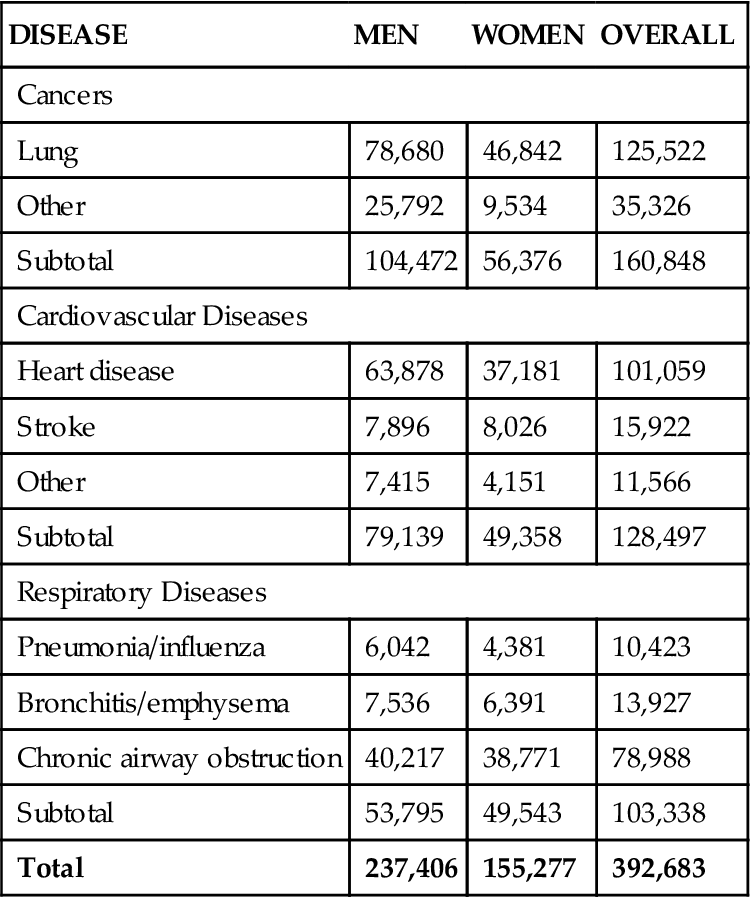
Modified from Centers for Disease Control and Prevention: Smoking-Attributable Mortality, Years of Potential Life Lost, and Productivity Losses—United States, 2000-2004. Available at http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/tobacco_related_mortality/index.htm. Accessed July 9, 2010.
The economic toll from tobacco use in the United States is enormous. Between 2000 and 2004, cigarette smoking was responsible for approximately $193 billion in annual health-related losses, with $96 billion in direct medical costs and $97 billion in lost productivity (CDC, 2008a).
Nicotine, the active ingredient in the tobacco plant, is a particularly toxic drug. To protect itself, the body quickly develops tolerance to the nicotine. If a person smokes regularly, tolerance to nicotine develops within hours, compared with days for heroin or months for alcohol. Pipes and cigars are less hazardous than cigarettes because the harsher smoke discourages deep inhalation. However, pipes and cigars increase the risk of cancer of the lips, mouth, and throat.
Smoke can be inhaled directly by the smoker (mainstream smoke), or it can enter the atmosphere from the lighted end of the cigarette and be inhaled by others in the vicinity (sidestream smoke). Sidestream or second-hand smoke contains higher concentrations of toxic and carcinogenic compounds than mainstream smoke. An estimated 3000 annual lung cancer deaths and over 1 million illnesses in children are attributed to sidestream smoke (Barry, 2007). Sidestream smoke is only about 20% less dangerous than actually smoking, and most of the toxic effects occur within the first 5 minutes of exposure (Barnoya and Glanz, 2005). Smoking bans are being adopted to reduce the discomfort and health hazards among non-smokers.
Nicotine is also used as chewing tobacco or snuff. Marketed as “smokeless tobacco,” a wad is put in the mouth and the nicotine is absorbed sublingually. Higher doses of nicotine are delivered in the smokeless forms because the nicotine is not destroyed by heat. Nevertheless, this form is less addictive because nicotine enters the bloodstream less directly. Smokeless tobacco users are 20% more likely to die of heart disease than non-users (Henley et al, 2005), and they are at a higher risk for cancer of the mouth, pharynx, esophagus, stomach, and pancreas (Boffetta et al, 2005).



