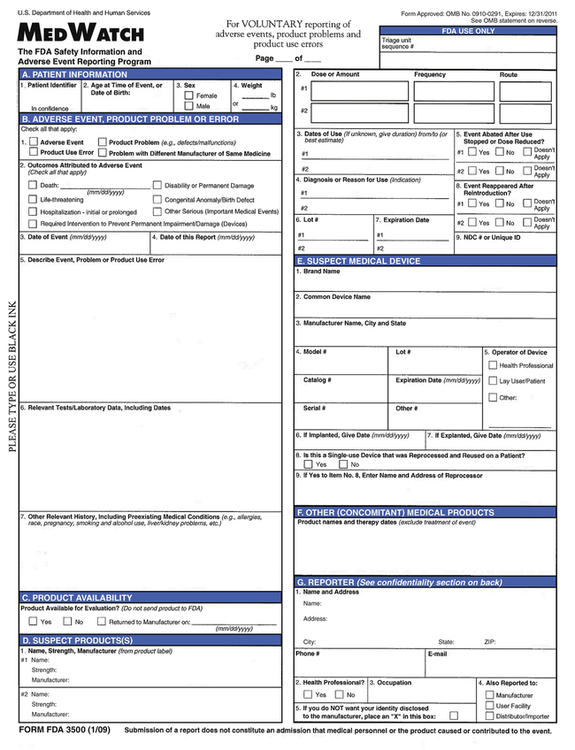
CHAPTER 7 Fortunately, liver failure from using known hepatotoxic drugs is rare, with an incidence of less than 1 in 50,000. (Drugs that cause liver failure more often than this are removed from the market—unless they are indicated for a life-threatening illness.) More than 50 drugs are known to be hepatotoxic. Some of these are listed in Table 7–1. TABLE 7–1 Statins and Other Lipid-Lowering Drugs Atorvastatin [Lipitor] Oral Antidiabetic Drugs Acarbose [Precose] Antiseizure Drugs Carbamazepine [Tegretol] Antifungal Drugs Itraconazole [Sporanox] Drugs for Tuberculosis Isoniazid Immunosuppressants Azathioprine [Imuran] Antiretroviral Drugs Nevirapine [Viramune] Other Drugs Acetaminophen [Tylenol, others], but only when combined with alcohol, or when taken in excessive dosage The term QT interval drugs—or simply QT drugs—refers to the ability of some medications to prolong the QT interval on the electrocardiogram, thereby creating a risk of serious dysrhythmias. As discussed in Chapter 49 (Antidysrhythmic Drugs), the QT interval is a measure of the time required for the ventricles to repolarize after each contraction. When the QT interval is prolonged, patients can develop a dysrhythmia known as torsades de pointes, which can progress to potentially fatal ventricular fibrillation. How long must the QT interval be to be considered long? More than 470 msec for postpubertal males, or more than 480 msec for postpubertal females. More than 100 drugs are known to cause QT prolongation, torsades de pointes, or both. As shown in Table 7–2, QT drugs are found in many drug families. Seven QT drugs—including astemizole [Hismanal], terfenadine [Seldane], and fenfluramine [Pondimin]—have been withdrawn because of deaths linked to their use, and use of another QT drug—cisapride [Propulsid]—is now restricted. To reduce the risks from QT drugs, the Food and Drug Administration (FDA) now requires that all new drugs be tested for the ability to cause QT prolongation. TABLE 7–2 Drugs That Prolong the QT Interval, Induce Torsades de Pointes, or Both Cardiovascular: Antidysrhythmics Amiodarone [Cordarone] Cardiovascular: ACE Inhibitors/CCBs Bepridil [Vascor] Cardiovascular: Others Dobutamine [Dobutrex] Antibiotics Azithromycin [Zithromax] Antifungal Drugs Antidepressants Amitriptyline [Elavil] Antipsychotics Chlorpromazine [Thorazine] Antiemetics/Antinausea Drugs Dolasetron [Anzemet] Bronchodilators Albuterol [Proventil, Ventolin] Anticancer Drugs Arsenic trioxide [Trisenox] Drugs for ADHD Amphetamine/dextroamphetamine [Adderall] Nasal Decongestants Phenylephrine [Neo-Synephrine, Sudafed PE] Other Drugs Alfuzosin [Uroxatral] When QT drugs are used, care is needed to minimize the risk of dysrhythmias. These agents should be used with caution in patients predisposed to dysrhythmias. Among these are the elderly and patients with bradycardia, heart failure, congenital QT prolongation, and low levels of potassium or magnesium. Women are also at risk. Why? Because their normal QT interval is longer than the QT interval in men. Concurrent use of two or more QT drugs should be avoided, as should the concurrent use of a QT drug with another drug that can raise its blood level (eg, by inhibiting its metabolism). Obviously, excessive dosing should be avoided. Additional information on QT drugs, including a current list of these agents, is available online at www.QTdrugs.org. • Did symptoms appear shortly after the drug was first used? • Did symptoms abate when the drug was discontinued? • Did symptoms reappear when the drug was reinstituted? • Is the illness itself sufficient to explain the event? • Are other drugs in the regimen sufficient to explain the event? As we discussed in Chapter 3, preclinical and clinical trials of new drugs cannot detect all of the ADRs that a drug may be able to cause. In fact, about 50% of all new drugs have serious ADRs that are not revealed during Phase II and Phase III trials. If you suspect a drug of causing a previously unknown adverse effect, you should report the effect to MEDWATCH, the FDA Medical Products Reporting Program. You can file your report online at www.fda.gov/medwatch. The form used for reporting is shown in Figure 7–1. Because voluntary reporting by healthcare professionals is an important mechanism for bringing ADRs to light, you should report all suspected ADRs, even if absolute proof of the drug’s complicity has not been established.
Adverse drug reactions and medication errors
Adverse drug reactions
Organ-specific toxicity
Hepatotoxic drugs

Fenofibrate [Tricor]
Fluvastatin [Lescol]
Gemfibrozil [Lopid]
Lovastatin [Mevacor]
Niacin [Niaspan, others]
Pravastatin [Pravachol]
Simvastatin [Zocor]
Pioglitazone [Actos]
Rosiglitazone [Avandia]
Felbamate [Felbatol]
Valproic acid [Depakene, others]
Ketoconazole [Nizoral]
Terbinafine [Lamisil]
Pyrazinamide
Rifampin [Rifadin]
Methotrexate [Rheumatrex]
Ritonavir [Norvir]
Amiodarone [Cordarone]
Diclofenac [Voltaren]
Duloxetine [Cymbalta]
Halothane [Fluothane]
Leflunomide [Arava]
Methyldopa [Aldomet]
Nefazodone
Nitrofurantoin [Macrodantin]
Tacrine [Cognex]
Tamoxifen [Nolvadex]
Zileuton [Zyflo]
QT interval drugs

Disopyramide [Norpace]
Dofetilide [Tikosyn]
Flecainide [Tambocor]
Ibutilide [Corvert]
Mexiletine [Mexitil]
Procainamide [Procan, Pronestyl]
Quinidine
Sotalol [Betapace]
Isradipine [DynaCirc]
Moexipril
Nicardipine [Cardene]
Dopamine
Norepinephrine [Levophed]
Ranolazine [Ranexa]
Clarithromycin [Biaxin]
Erythromycin
Gatifloxacin [Tequin]
Gemifloxacin [Factive]
Levofloxacin [Levaquin]
Moxifloxacin [Avelox]
Ofloxacin [Floxin]
Sparfloxacin [Zagam]
Telithromycin [Ketek]
Fluconazole [Diflucan]
Itraconazole [Sporanox]
Ketoconazole [Nizoral]
Voriconazole [Vfend]
Citalopram [Celexa]
Desipramine [Norpramin]
Doxepin [Sinequan]
Fluoxetine [Prozac]
Imipramine [Tofranil]
Protriptyline [Pamelor, Aventyl]
Sertraline [Zoloft]
Trimipramine [Surmontil]
Venlafaxine [Effexor]
Clozapine [Clozaril]
Haloperidol [Haldol]
Mesoridazine [Serentil]
Pimozide [Orap]
Quetiapine [Seroquel]
Risperidone [Risperdal]
Thioridazine [Mellaril]
Ziprasidone [Geodon]
Domperidone [Motilium]
Droperidol [Inapsine]
Granisetron [Kytril]
Ondansetron [Zofran]
Ephedrine
Epinephrine [Bronkaid, Primatene]
Isoproterenol [Isuprel]
Levalbuterol [Xopenex]
Metaproterenol [Alupent]
Salmeterol [Serevent]
Terbutaline
Sunitinib [Sutent]
Tamoxifen [Nolvadex]
Atomoxetine [Strattera]
Dexmethylphenidate [Focalin]
Dextroamphetamine [Dexedrine]
Methylphenidate [Ritalin, Concerta]
Pseudoephedrine [Sudafed]
Amantadine [Symmetrel]
Chloroquine [Aralen]
Cisapride [Propulsid]*
Cocaine
Felbamate [Felbatol]
Foscarnet [Foscavir]
Fosphenytoin [Cerebyx]
Galantamine [Razadyne]
Halofantrine [Halfan]
Indapamide [Lozol]
Lithium [Lithobid, Eskalith]
Methadone [Dolophine]
Midodrine [ProAmatine]
Octreotide [Sandostatin]
Pentamidine [Pentam, Nebupent]
Phentermine [Fastin]
Ritodrine [Yutopar]
Salmeterol [Serevent]
Solifenacin [Vesicare]
Tacrolimus [Prograf]
Tizanidine [Zanaflex]
Tolterodine [Detrol]
Vardenafil [Levitra]
Identifying adverse drug reactions
Adverse reactions to new drugs
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Adverse drug reactions and medication errors
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access