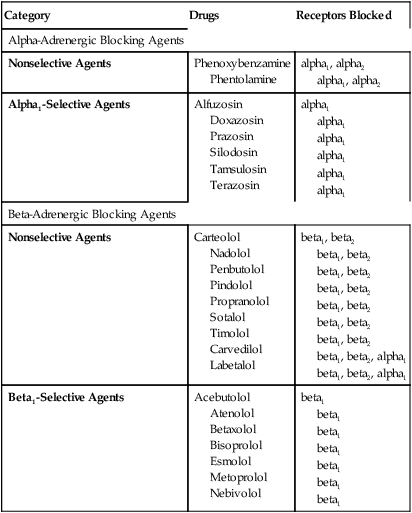
CHAPTER 18 Unlike many adrenergic agonists, which act at alpha- and beta-adrenergic receptors, most adrenergic antagonists are more selective. As a result, the adrenergic antagonists can be neatly divided into two major groups: (1) alpha-adrenergic blocking agents (drugs that produce selective blockade of alpha-adrenergic receptors); and (2) beta-adrenergic blocking agents (drugs that produce selective blockade of beta receptors).* Members of these two groups are listed in Table 18–1. TABLE 18–1 Receptor Specificity of Adrenergic Antagonists Remember that it is much easier to understand responses to the adrenergic drugs if you first understand the responses to activation of adrenergic receptors. Accordingly, if you have not yet mastered (memorized) Table 13–3, you should do so now (or at least be prepared to consult the table as we proceed). Hypertension (high blood pressure) can be treated with a variety of drugs, including the alpha-adrenergic antagonists. Alpha antagonists lower blood pressure by blocking alpha1 receptors on arterioles and veins, causing vasodilation. Dilation of arterioles reduces arterial pressure directly. Dilation of veins lowers arterial pressure by an indirect process: In response to venous dilation, return of blood to the heart decreases, thereby decreasing cardiac output, which in turn reduces arterial pressure. The role of alpha-adrenergic blockers in essential hypertension is discussed further in Chapter 47 (Drugs for Hypertension). BPH results from proliferation of cells in the prostate gland. Symptoms include dysuria, increased frequency of daytime urination, nocturia, urinary hesitance and intermittence, urinary urgency, a sensation of incomplete voiding, and a reduction in the size and force of the urinary stream. All of these symptoms can be improved with drugs that block alpha1 receptors. Benefits derive from reduced contraction of smooth muscle in the prostatic capsule and the bladder neck (trigone and sphincter). BPH is discussed at length in Chapter 66. As indicated in Table 18–1, the alpha-adrenergic blocking agents can be subdivided into two major groups. One group, represented by prazosin, contains drugs that produce selective alpha1 blockade. The second group, represented by phentolamine, consists of nonselective alpha blockers, which block alpha1 and alpha2 receptors. Angina pectoris (paroxysmal pain in the region of the heart) occurs when oxygen supply (blood flow) to the heart is insufficient to meet cardiac oxygen demand. Anginal attacks can be precipitated by exertion, intense emotion, and other factors. Beta-adrenergic blockers are a mainstay of antianginal therapy. By blocking beta1 receptors in the heart, these drugs decrease cardiac work. This brings oxygen demand back into balance with oxygen supply, and thereby prevents pain. Angina pectoris and its treatment are the subject of Chapter 51.
Adrenergic antagonists

Category
Drugs
Receptors Blocked
Alpha-Adrenergic Blocking Agents
Nonselective Agents
Phenoxybenzamine
Phentolamine
alpha1, alpha2
alpha1, alpha2
Alpha1-Selective Agents
Alfuzosin
Doxazosin
Prazosin
Silodosin
Tamsulosin
Terazosin
alpha1
alpha1
alpha1
alpha1
alpha1
alpha1
Beta-Adrenergic Blocking Agents
Nonselective Agents
Carteolol
Nadolol
Penbutolol
Pindolol
Propranolol
Sotalol
Timolol
Carvedilol
Labetalol
beta1, beta2
beta1, beta2
beta1, beta2
beta1, beta2
beta1, beta2
beta1, beta2
beta1, beta2
beta1, beta2, alpha1
beta1, beta2, alpha1
Beta1-Selective Agents
Acebutolol
Atenolol
Betaxolol
Bisoprolol
Esmolol
Metoprolol
Nebivolol
beta1
beta1
beta1
beta1
beta1
beta1
beta1
Alpha-adrenergic antagonists
Therapeutic and adverse responses to alpha blockade
Therapeutic applications of alpha blockade
Essential hypertension.
Benign prostatic hyperplasia.
Adverse effects of alpha blockade
Adverse effects of alpha1 blockade
Properties of individual alpha blockers
Beta-adrenergic antagonists
Therapeutic and adverse responses to beta blockade
Therapeutic applications of beta blockade
Angina pectoris.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Adrenergic antagonists
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access
