Adaptations to Pregnancy
Learning Objectives
After studying this chapter, you should be able to:
• Describe the physiologic and psychological changes that occur during pregnancy.
• Compute gravidity, parity, and estimated date of delivery.
• Describe preconception, initial, and subsequent antepartum assessments.
• Discuss maternal adaptations to multifetal pregnancy.
• Develop a plan of nursing care for common problems and discomforts of pregnancy.
• Identify the process of role transition.
• Explain the maternal tasks of pregnancy.
• Describe the developmental processes of the transition to the father role.
• Describe the responses of prospective grandparents and siblings to pregnancy.
• Describe cultural influences on pregnancy and cultural assessment and negotiation.
• Describe the various types of education for childbearing families.
![]()
http://evolve.elsevier.com/McKinney/mat-ch/
From the moment of conception important changes occur in a pregnant woman’s body. These changes are necessary to support and nourish the fetus and to prepare the woman for childbirth and lactation. Changes also occur in her psychological responses to the pregnancy. Nurses must understand not only the physiologic and psychological changes but also how these changes affect the daily lives of expectant mothers.
Physiologic Responses to Pregnancy
Changes in Body Systems
Pregnancy challenges each body system to adapt to the increasing demands of the fetus.
Reproductive System
Uterus
Growth
Before conception, the uterus is a small pear-shaped organ entirely contained in the pelvic cavity. It weighs up to 70 g (2.5 oz) and has a capacity of approximately 10 mL (one third of an ounce). By full term (the end of normal pregnancy) the uterus weighs approximately 1100 to 1200 g (2.4 to 2.6 lb) and has a capacity of approximately 5000 mL (Norwitz & Lye, 2009). Uterine growth occurs as the result of hyperplasia and hypertrophy. Growth can be predicted for each trimester (one of three 13-week periods of pregnancy). During the first trimester, growth is mainly a result of hyperplasia caused by stimulation from estrogen and growth factors. During the second and third trimesters, uterine growth is caused by hyperplasia and hypertrophy as the muscle fibers stretch to accommodate the growing fetus. Fibrous tissue accumulates in the outer muscle layer of the uterus, and the amount of elastic tissue increases. These changes greatly increase the strength of the muscle wall (Cunningham, Leveno, Bloom, et al., 2010).
Muscle fibers in the myometrium increase in both length and width. By the third trimester, the uterine muscles are thin, and the fetus can be easily palpated through the abdominal wall. As the uterus expands into the abdominal cavity and rotates to the right, it displaces the intestines upward and laterally. Uterine rotation is caused by pressure from the rectosigmoid colon on the left side of the pelvis.
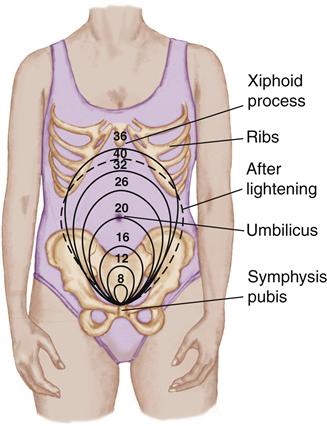
Pattern of Uterine Growth
The uterus enlarges in a predictable pattern that provides information about fetal growth and helps to confirm the estimated date of delivery (EDD), sometimes called the estimated date of birth (EDB) (Figure 13-1). By 12 weeks of gestation, the fundus (top of the uterus) can be palpated above the symphysis pubis. At 16 weeks, the fundus reaches midway between the symphysis pubis and the umbilicus. It is located at the umbilicus by 20 weeks’ gestation.
The fundus reaches its highest level at the xiphoid process at 36 weeks. Because it pushes against the diaphragm, many expectant mothers experience shortness of breath. By 40 weeks, the fetal head descends into the pelvic cavity and the uterus sinks to a lower level. This descent of the fetal head is called lightening because it reduces pressure on the diaphragm and makes breathing easier. Lightening is more pronounced in first pregnancies.
Contractility
Throughout pregnancy, the uterus undergoes irregular contractions called Braxton Hicks contractions. During the first two trimesters, contractions are infrequent and less noticeable. During the third trimester, contractions occur more frequently and may cause some discomfort. They are called false labor when they are mistaken for the onset of early labor.
Uterine Blood Flow
As the uterus increases in size, blood flow rises dramatically. In early pregnancy, when the uterus and placenta are relatively small, most of the blood flow is directed to the myometrium and endometrium. During late pregnancy, blood flow to the uterus and placenta reaches 1200 mL/min (Koos, Kahn, & Equils, 2010). Adequate perfusion of the placental intervillous spaces is essential for the delivery of substances needed for fetal growth and the removal of metabolic wastes.
Cervix
The most obvious cervical changes occur in color and consistency. Estrogen causes hyperemia (congestion with blood) of the cervix, resulting in the characteristic bluish purple color that extends to include the vagina and labia. This discoloration, referred to as Chadwick’s sign, is one of the earliest signs of pregnancy.
Collagen fibers in the connective tissue of the cervix decrease, causing the cervix to soften. Before pregnancy, the cervix has a consistency similar to that of the tip of the nose. After conception, the cervix feels more like the lips or earlobe. The cervical softening is referred to as Goodell’s sign.
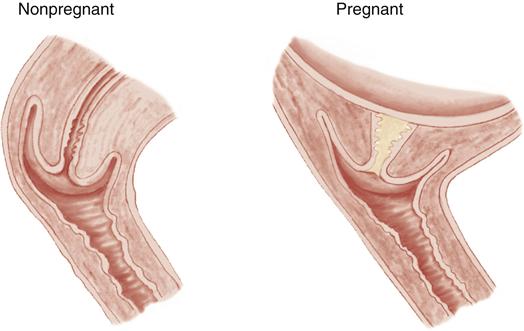
The cervical glands proliferate during pregnancy, and the endocervical tissue resembles a honeycomb that fills with mucus. The mucus plugs the cervical canal and blocks the ascent of bacteria from the vagina into the uterus during pregnancy (Figure 13-2). One of the earliest signs of labor may be “bloody show,” which consists of the mucous plug plus a small amount of blood. This bleeding occurs from disruption of the cervical capillaries as the mucous plug is dislodged when the cervix begins to thin and dilate.
Vagina and Vulva
Increased vascularity of the vagina causes the vaginal walls, as well as the cervix, to appear a bluish purple in color. Loosening of the abundant connective tissue allows the vagina to distend during childbirth. The vaginal mucosa thickens, and vaginal rugae (folds) become very prominent.
Vaginal cells contain increasing amounts of glycogen, which causes rapid sloughing and increased vaginal discharge. The pH of the vaginal discharge is acidic because of the increased production of lactic acid that results from the action of Lactobacillus acidophilus on glycogen in the vaginal epithelium (Cunningham et al., 2010). The acidic condition helps to prevent growth of harmful bacteria found in the vagina. However, the glycogen-rich environment favors the growth of Candida albicans, so that persistent yeast infections (candidiasis) are common during pregnancy.
Increased vascularity, edema, and connective tissue changes make the tissues of the vulva and perineum more pliable. Pelvic congestion during pregnancy can lead to heightened sexual interest and increased orgasmic experiences.
Ovaries
After conception, the major function of the ovaries is to secrete progesterone from the corpus luteum for the first 6 to 7 weeks of pregnancy. Progesterone is called the hormone of pregnancy because adequate progesterone must be available from the earliest stages if the pregnancy is to be maintained. The corpus luteum secretes progesterone until the placenta is developed. Once developed, the placenta produces progesterone throughout pregnancy.
Ovulation ceases during pregnancy because the circulating levels of estrogen and progesterone are high, inhibiting the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) necessary for ovulation.
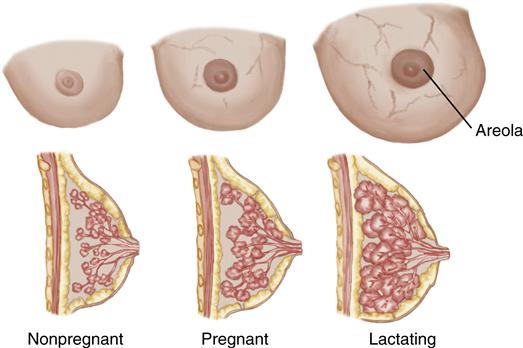
Breasts
During pregnancy the breasts change in size and appearance (Figure 13-3). Estrogen stimulates the growth of mammary ductal tissue, and progesterone promotes the growth of lobes, lobules, and alveoli. The breasts become highly vascular, and a delicate network of veins is often visible. If the increase in breast size is extensive, lineal tears in the connective tissue (striae gravidarum or “stretch marks”) may develop.
Characteristic changes in the nipples and areolae occur during pregnancy. The nipples increase in size and become darker and more erect, and the areolae become larger and more pigmented. Women with very light complexions exhibit less change in pigmentation than those with darker skin tones. Sebaceous glands, called tubercles of Montgomery, become more prominent during pregnancy and secrete a substance that lubricates the nipples. In addition, a thick, yellowish fluid (colostrum) is present beginning at 12 to 16 weeks of pregnancy and can readily be expressed from the breasts by the third trimester (Janke, 2008). Secretion of milk is suppressed during pregnancy by high levels of estrogen and progesterone.
Cardiovascular System
Heart
Heart Size and Position
Cardiac changes are relatively minor and reverse soon after childbirth. The muscles of the heart (myocardium) enlarge slightly because of an increased workload during pregnancy. The heart is pushed upward and toward the left as the uterus elevates the diaphragm during the third trimester. As a result of the change in position, the locations for auscultating heart sounds may be shifted upward and laterally in late pregnancy.
Heart Sounds
During pregnancy some heart sounds may be so altered that they would be considered abnormal in a nonpregnant state. The changes are first heard between 12 and 20 weeks and regress during the first week after childbirth. The most common variations in heart sounds include splitting of the first heart sound and a third heart sound. A systolic murmur is found in 95% of pregnant women. The murmur may persist beyond the 4th week for approximately 20% of postpartum women (Monga, 2009).
Blood Volume
Total Volume
Total blood volume is a combination of plasma and other components, such as red blood cells (RBCs, erythrocytes), white blood cells (WBCs, leukocytes), and platelets (thrombocytes). Total blood volume increases by as much as 45% (Jones, 2009).
Plasma Volume
Plasma volume increases progressively from 6 to 8 weeks of gestation until approximately 32 weeks. This is an increase of 40% to 60% (1200 to 1600 mL) above nonpregnant values. Increases are greater in multifetal pregnancies. The increase may be related to vasodilation from nitric oxide, and estrogen and progesterone stimulation of the renin-angiotensin-aldosterone system, which stimulates sodium and water retention (Blackburn, 2013).
The increased volume is needed to: (1) transport nutrients and oxygen to the placenta, where they become available for the growing fetus; and (2) meet the demands of the expanded maternal tissue in the uterus and breasts. The greater volume also provides a reserve to protect the pregnant woman from the adverse effects of the blood loss that occurs during childbirth.
Red Blood Cell Mass
RBC mass increases by 250 to 450 mL, approximately 20% to 30% above prepregnancy values (Blackburn, 2013). The increase in plasma volume is more pronounced and occurs earlier than the increase in RBC volume. The resulting dilution of RBC mass causes a decline in maternal hemoglobin and hematocrit. This condition is frequently called physiologic anemia or pseudoanemia of pregnancy because it reflects the dilution of RBCs in an expanded plasma volume rather than an actual decline in the number of RBCs. Therefore, it does not indicate true anemia.
Frequent laboratory examinations may be needed to distinguish physiologic anemia from true anemia. Generally, iron deficiency anemia occurs when the hemoglobin is less than 11 g/dL or the hematocrit is less than 33% in the first or third trimesters, or the hemoglobin is less than 10.5 g/dL or the hematocrit is less than 32% in the second trimester (Centers for Disease Control and Prevention [CDC], 1998; Cunningham et al., 2010). Iron supplementation is often prescribed for pregnant women by the second trimester to prevent anemia.
Dilution of RBCs by plasma may also have a protective function. By decreasing blood viscosity, dilution may counter the tendency to form clots (thrombi) that can obstruct blood vessels and cause serious complications (see Chapter 28). Hemodilution may also increase intervillous perfusion (Monga, 2009).
Cardiac Output
The expanded blood volume of pregnancy causes an increase in cardiac output—the amount of blood ejected from the heart each minute. It is based on stroke volume (the amount of blood pumped from the heart with each contraction) and heart rate (the number of times the heart beats each minute). Cardiac output rises up to 50% with half of the rise occurring in the first 8 weeks of gestation (Beckmann, Ling, Barzansky, et al., 2010). The increase in cardiac output is caused primarily by a gain in stroke volume, but the heart rate also rises about 15 to 20 beats per minute (bpm) (Bond, 2011). Cardiac output is most efficient when the woman is lying in the lateral position and least efficient in the supine position.
Systemic Vascular Resistance
Systemic vascular resistance diminishes during pregnancy. This change is likely the result of (1) vasodilation caused by the effects of progesterone and prostaglandins; (2) the addition of the uteroplacental unit, which provides low resistance and a greater area for circulation; (3) fetal, maternal, and placental heat production, which causes vasodilation; (4) decreased vascular sensitivity to angiotensin II; and (5) endothelial prostacyclin and endothelial-derived relaxant factors such as nitric oxide (Blackburn, 2013).
Blood Pressure
As a result of decreased systemic vascular resistance, blood pressure (BP) changes little during pregnancy despite the increase in blood volume.
Effect of Position on Blood Pressure
Arterial blood pressure is affected by the woman’s position during pregnancy. With the woman in the sitting or standing position, the systolic pressure remains largely unchanged and diastolic pressure decreases (by about 10 mm Hg) by 24 weeks and then returns to prepregnancy levels by term. When the woman is lying in the left lateral position, systolic pressure decreases 5 to 10 mm Hg, and diastolic BP decreases 10 to 15 mm Hg (Monga, 2009).
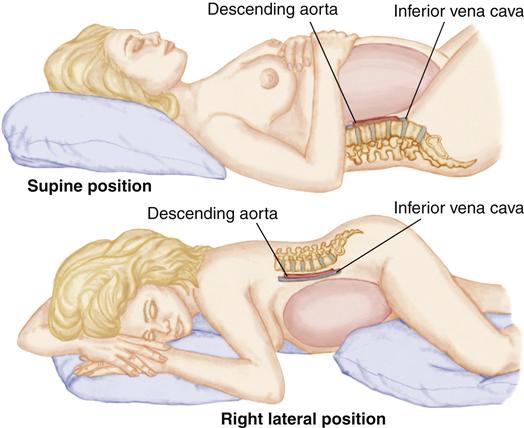
Supine Hypotension
When the pregnant woman is in the supine position, particularly during the second half of pregnancy, the weight of the gravid (pregnant) uterus partially occludes the vena cava and the aorta (Figure 13-4). The occlusion may impede return of blood from the lower extremities and reduce cardiac return, cardiac output, and blood pressure. Collateral circulation developed in pregnancy generally allows blood flow from the legs and pelvis to return to the heart when the woman is in a supine position (Blackburn, 2013). However, some women develop supine hypotensive syndrome.
Symptoms include faintness, lightheadedness, dizziness, nausea, and agitation. Some may experience syncope, a brief lapse in consciousness. Blood flow through the placenta also decreases if the woman remains in the supine position for a prolonged period, which could cause fetal hypoxia.
Turning to a lateral recumbent position alleviates the pressure on the blood vessels and quickly corrects supine hypotension. Women should be advised to rest in a side-lying position to prevent supine hypotension. If they must lie in a supine position for any reason, a wedge or pillow under either hip is effective in decreasing supine hypotension.
Blood Flow
Five major changes in blood flow occur during pregnancy (Koos et al., 2010):
Blood Components
Although iron absorption and iron-binding power are increased during pregnancy, sufficient iron is not always supplied by diet. Iron supplementation is needed to promote hemoglobin synthesis and ensure that erythrocyte production is sufficient to prevent iron deficiency anemia (see Chapter 26). During pregnancy, erythrocyte production increases by 30% if the mother takes iron supplements and by 18% without supplementation (Gordon, 2007).
Leukocytes increase during pregnancy, ranging from 5000 to 12,000 cells/mm3 to as high as 15,000 cells/mm3 (Blackburn, 2013). Leukocytes increase further during labor and the early postpartum period, reaching 25,000 to 30,000 cells/mm3 (Cunningham et al., 2010).
Pregnancy is a hypercoagulable state where the mother’s blood clots more readily. This is because of an increase in factors that favor coagulation and a decrease in factors that inhibit coagulation. Fibrinogen (factor I) increases 50% and factors VII, VIII, IX, and X also rise (Beckmann et al., 2010). Fibrinolytic activity (to break down clots) decreases during pregnancy. Platelets may decrease slightly but remain within normal range (Blackburn, 2013). These changes offer some protection from hemorrhage during childbirth, but also increase the risk of thrombus formation. The risk is a particular concern if the woman must stand or sit for prolonged periods, causing stasis of blood in the veins of the legs. (See Table 13-1 for additional changes in blood components.)
TABLE 13-1
LABORATORY VALUES IN NONPREGNANT AND PREGNANT WOMEN
| VALUE | NONPREGNANT | PREGNANT |
| Red blood cell count | 4.2-5.4 million/mm3 | 3.8-4.4 million/mm3; Decreases slightly because of hemodilution |
| Hemoglobin | 12-16 g/dL | At least 11 g/dL during 1st and 3rd trimesters and at least 10.5 g/dL during 2nd trimester |
| Hematocrit, packed cell volume | 37%-47% | At least 33% during 1st and 3rd trimesters and at least 32% during 2nd trimester |
| White blood cell | 5000-10,000 /mm3 | 5000-15,000 /mm3 |
| Platelets | 150,000-400,000/mm3 | Slight decrease but within normal range |
| Prothrombin time | 11-12.5 sec | Slight decrease |
| Activated partial thromboplastin | 30-40 sec | Slight decrease |
| D-dimer | Negative | Negative |
| Glucose, blood | ||
| Fasting | 70-110 mg/dL | 95 mg/dL or lower |
| Postprandial | <140 mg/dL | <140 mg/dL |
| Creatinine | 0.65 ± 0.14 mg/dL | 0.46 ± 0.13 mg/dL |
| Creatinine clearance, urine | 85-120 mL/min | 110-150 mL/min |
| Fibrinogen | 200-400 mg/dL | 300-600 g/dL |
Data from Blackburn, S. T. (2013). Maternal, fetal, and neonatal physiology: A clinical perspective (4th ed.). St. Louis: Saunders; Blackburn, S. T. (2008). Physiologic changes of pregnancy. In K. R. Simpson & P. A. Creehan (Eds.), AWHONN perinatal nursing (3rd ed., pp. 59-77). Philadelphia: Lippincott Williams & Wilkins; Cunningham, F. G., Leveno, K. J., Bloom, S. L., et al. (2010). Williams obstetrics (23rd ed.). New York: McGraw-Hill; Pagana, K. D., & Pagana, T. J. (2009). Mosby’s diagnostic and laboratory test reference (9th ed.). St. Louis: Mosby.
Respiratory System
Oxygen Consumption
Oxygen consumption increases by approximately 20% in pregnancy. Half the oxygen is used by the uterus, fetus, and placenta. The rest is consumed by the breast tissue, and increased cardiac, renal, and respiratory maternal demands (Beckmann et al., 2010). To compensate for the increased need for oxygen, the woman hyperventilates slightly by breathing more deeply, although her respiratory rate remains unchanged. This hyperventilation promotes the transfer of carbon dioxide from fetal to maternal circulation (Monga, 2009).
Hyperventilation also causes a tidal volume (the volume of gas moved into or out of the respiratory tract with each breath) increase of 30% to 40% causing an increase in the respiratory minute volume (the volume of air inspired or expired in 1 minute) (Beckmann et al., 2010). As a result of the elevated minute volume, the partial pressure of carbon dioxide (PCO2) is lowered. Renal excretion of bicarbonate from the kidneys compensates for the resulting respiratory alkalosis.
Hormonal Factors
Progesterone
Progesterone and prostaglandins play a role in decreasing airway resistance by relaxing smooth muscle in the respiratory tract. Progesterone is also believed to raise the sensitivity of the respiratory center (medulla oblongata) to carbon dioxide, thus stimulating the increase in minute ventilation. These two factors are responsible for the heightened awareness of the need to breathe experienced by many pregnant women.
Estrogen
Estrogen causes increased vascularity of the mucous membranes of the upper respiratory tract. As the capillaries become engorged, edema and hyperemia develop within the nose, pharynx, larynx, and trachea. This congestion may result in nasal and sinus stuffiness, epistaxis (nosebleed), and deepening of the voice. Increased vascularity also causes edema of the eardrum and eustachian tubes, which may result in a sense of fullness in the ears or earaches.
Physical Changes
Although the enlarging uterus lifts the diaphragm by approximately 4 cm (1.6 inches) by the third trimester, movement of the diaphragm is slightly increased. The total lung capacity is decreased 5% because of the elevated diaphragm (Callahan & Caughey, 2009). The ribs flare, the substernal angle widens, and the thoracic circumference increases by 5 to 7 cm (2 to 3 inches) (Bond, 2011). These changes result from relaxation of the ligaments around the ribs (Blackburn, 2013). Breathing becomes more thoracic than abdominal, adding to the dyspnea many women experience.
Gastrointestinal System
Mouth
Elevated levels of estrogen cause hyperemia of the tissues of the mouth and gums, which may lead to gingivitis and bleeding gums. Some women develop severe vascular hypertrophy of the gums, which appear reddened and swollen and bleed easily. The condition regresses spontaneously after childbirth.
Some women experience ptyalism (excessive salivation) that is unpleasant and embarrassing. The cause of ptyalism appears to be stimulation of the salivary glands by the ingestion of starch (Cunningham et al., 2010). Decreased swallowing during nausea and vomiting may also may play a part (Bond, 2011). Small, frequent meals, gum chewing, and oral lozenges offer limited relief.
Some women believe pregnancy adversely affects tooth mineralization, but the teeth do not lose minerals to the fetus. However, existing periodontal disease may be exacerbated during pregnancy and dental care is important.
Esophagus
The lower esophageal sphincter tone decreases during pregnancy, primarily because of the effect of progesterone on the smooth muscles. The relaxation of the esophageal sphincter and upward displacement of the stomach allow reflux of acidic stomach contents into the esophagus and produces heartburn (pyrosis).
Stomach
Elevated levels of progesterone relax all smooth muscle, decreasing gastrointestinal tone and motility. The effect on gastric emptying time is unclear with some studies showing a decrease and others showing no change during pregnancy (Beckmann et al., 2010; Cunningham et al., 2010).
Large and Small Intestine
Emptying time of the intestines is increased allowing more time for nutrient absorption. Calcium, amino acids, iron, glucose, sodium, and chloride are better absorbed during pregnancy, but absorption of some of the B vitamins is reduced (Blackburn, 2013). Decreased motility in the large intestine allows time for more water to be absorbed leading to constipation. Hemorrhoids may be caused or exacerbated by constipation if the expectant mother must strain to have bowel movements.
Liver and Gallbladder
Progesterone causes functional changes of the liver and gallbladder. The gallbladder becomes hypotonic and emptying time is prolonged, resulting in thicker bile and predisposing to the development of gallstones. Reduced gallbladder tone also leads to a tendency to retain bile salts, which can cause itching (pruritus) (Cunningham, et al., 2010).
During the last trimester the liver is pushed upward and backward by the enlarging uterus. Serum alkaline phosphatase rises to two to four times that of nonpregnant women and levels of serum albumin and total protein fall (Williamson & Mackillop, 2009).
Urinary System
Bladder
The woman experiences frequency of urination throughout pregnancy. Although uterine expansion within the pelvis is one cause of these urinary changes, frequency begins before the uterus is big enough to exert pressure on the bladder. Hormonal influences, the increased blood volume, and changes in glomerular filtration rate (GFR) may play a significant role in urinary frequency (Blackburn, 2013). Many women experience stress or urge incontinence that begins at any time during pregnancy and continues until after delivery. Nocturia is also common.
The bladder, like all smooth muscle, relaxes in response to increasing levels of progesterone. Bladder mucosa becomes congested with blood, and the bladder walls become hypertrophied as a result of stimulation from estrogen. Decreased drainage of blood from the base of the bladder makes the tissues edematous and susceptible to trauma and infection during childbirth. The base of the bladder is pushed forward and upward near the end of pregnancy by pressure from the uterus.
Kidneys and Ureters
Changes in Size and Shape
During pregnancy, the kidneys change in both size and shape because of dilation of the renal pelves, calyces, and ureters above the pelvic brim. The dilation is caused by (1) the effect of progesterone, which causes the ureters to become elongated and more distensible; and (2) compression of the ureters between the enlarging uterus and the bony pelvic brim. The flow of urine through the ureters is partially obstructed, particularly on the right side, causing the ureters and renal pelvis to dilate. The resulting stasis of urine allows additional time for bacteria to multiply and increases the risk of urinary tract infection during pregnancy.
Functional Changes
Renal blood flow increases by 50% to 80% by the middle of pregnancy, then decreases as the pregnancy progresses to term (Blackburn, 2013). The rise is the result of increases in plasma volume and cardiac output. The GFR, the rate at which water and dissolved substances are filtered in the glomerulus, increases by 50% beginning in the second trimester (Cunningham et al., 2010; Prasad, 2007). This increase is the result of the rise in renal blood flow and of decreased colloid osmotic pressure caused by a reduction in the concentration of plasma proteins.
The increases in renal plasma flow and GFR are necessary for excretion of additional metabolic waste from the mother and fetus, but they also affect the excretion of glucose, amino acids, electrolytes, and water-soluble vitamins. As the GFR increases, the filtered load of these substances exceeds the ability of the renal tubules to reabsorb them, and they spill into the urine (Blackburn, 2008). Therefore glycosuria is common during pregnancy. Bacteria thrive in urine that is rich in nutrients, increasing the risk of urinary tract infections during pregnancy.
Mild proteinuria is common and does not necessarily mean there is abnormal kidney function or preeclampsia (Blackburn, 2013). Urinary protein is monitored throughout pregnancy to identify increases that would indicate a problem. Tests of renal function may be misleading during pregnancy. As a result of increased GFR, blood urea nitrogen and serum creatinine normally decline (Blackburn, 2013).
Integumentary System
Skin
Circulation to the skin increases during pregnancy and encourages activity of the sweat and sebaceous glands. Pregnant women feel warmer and perspire more, particularly during the last trimester. Accelerated activity of the sebaceous glands fosters the development of acne. Additional changes include hyperpigmentation and vascular changes in the skin.
Hyperpigmentation
Increased pigmentation from elevated estrogen, progesterone, and melanocyte-stimulating hormone may begin as early as the 8th week. Women with dark hair or skin exhibit more hyperpigmentation than women with very light hair and skin.
Areas of pigmentation include brownish patches, called melasma, chloasma, or the mask of pregnancy, over the forehead, cheeks, and nose. Melasma may also occur in women taking oral contraceptives. It increases with exposure to sunlight, but use of sunscreen may reduce the severity.
The linea alba (the line that marks the longitudinal division of the midline of the abdomen) darkens to become the linea nigra (Figure 13-5). The nipples, areolae, and preexisting moles (nevi) become darker as pregnancy progresses. Hyperpigmentation usually disappears after childbirth, when the levels of estrogen and progesterone decline, although melasma may persist in some women.
Cutaneous Vascular Changes
Blood vessels dilate and proliferate during pregnancy, an effect of estrogen. Changes in surface blood vessels are obvious during pregnancy, especially in women with fair skin. These include spider angiomas that appear as tiny red elevations that branch in all directions. Redness of the palms or soles of the feet, known as palmar erythema, also occurs in many white women and in some African-American women. Vascular changes may be emotionally distressing for the expectant mother, but they are clinically insignificant and usually disappear shortly after childbirth.
Connective Tissue
Striae gravidarum or “stretch marks” appear as slightly depressed pink to purple streaks on the abdomen, breasts, and buttocks. Striae fade to white or silvery lines but do not disappear after childbirth. Laser therapy is sometimes used after childbirth to reduce or eliminate severe striae. Many women believe that striae can be prevented by massage with oil, cocoa butter, or vitamin E, but no topical treatment has been found effective (Rapini, 2009). Lotions and antipruritic creams may be effective in controlling the itching that often occurs.
Hair
Because fewer follicles are in the resting phase, hair grows more rapidly and less hair falls out during pregnancy. After childbirth, hair follicles return to normal activity. Many women become concerned about the rate of hair loss that begins 2 to 4 months postpartum. They need reassurance that more follicles have returned to the normal resting phase and that excessive hair loss will not continue. Hair growth returns to normal 6 to 12 months after delivery (Beckmann et al., 2010).
Musculoskeletal System
Calcium Storage
During pregnancy, fetal demands for calcium increase, especially in the third trimester. Absorption of calcium from the intestine is increased from the first trimester, and calcium is stored to meet the later needs of the fetus (Blackburn, 2013). The amount of calcium transferred to the fetus is small in comparison with maternal stores, and there is no loss of maternal bone density to supply fetal needs.
Postural Changes
Musculoskeletal changes are progressive. They begin in the second trimester, when the hormones estrogen and progesterone initiate increased mobility of the pelvic ligaments. This facilitates passage of the fetus through the pelvis at the time of birth. At 28 to 30 weeks, the pelvic symphysis separates. Relaxation of the pelvic joints creates pelvic instability, and the woman may assume a wide stance and the waddling gait of pregnancy to compensate for a changing center of gravity.
During the third trimester, as the uterus increases in size, the expectant mother leans backward to maintain her balance. This posture creates a progressive lordosis, or curvature of the lower spine, and may lead to backache. Obesity or previous back problems increases the problem.
Abdominal Wall
During the third trimester, the abdominal muscles may become so stretched that the rectus abdominis muscles separate (diastasis recti). The extent of the separation varies from slight, which is clinically insignificant, to severe, when a large portion of the uterine wall is covered only by peritoneum, fascia, and skin (see Figure 20-4).
Endocrine System
Pituitary Gland
During pregnancy, prolactin from the anterior pituitary increases to prepare the breasts to produce milk. FSH and LH are suppressed because they are not needed to stimulate ovulation during pregnancy. The posterior pituitary produces oxytocin, which stimulates the milk-ejection reflex after childbirth. Oxytocin also stimulates contractions of the uterus, but during pregnancy, this action is inhibited by progesterone, which relaxes smooth muscle fibers of the uterus. After childbirth, progesterone levels decline when the placenta is removed, and oxytocin keeps the uterus contracted, preventing excessive bleeding at the placental site.
Thyroid Gland
Hyperplasia and increased vascularity cause the thyroid gland to enlarge during pregnancy. Early in the first trimester, a rise in total serum thyroxine (T4) and thyroxine-binding globulin occurs. The level of serum free (unbound) T4 rises in early pregnancy and then returns to normal. Maternal thyroid hormones are important in the development of the fetal brain. The basal metabolic rate (BMR) increases up to 25% primarily because of the fetal metabolic activity (Cunningham et al., 2010).
Parathyroid Glands
Parathyroid hormone, important for calcium homeostasis, decreases during the first trimester but then increases steadily throughout pregnancy (Cunningham et al., 2010). Calcium for transfer to the fetus is adequate.
Pancreas
During pregnancy, alterations in maternal blood glucose and fluctuations in insulin production occur. Glucose levels are 10% to 20% lower than before pregnancy, and hypoglycemia may develop between meals and at night as the fetus draws glucose from the mother (Blackburn, 2013).
During the second half of pregnancy, maternal tissue sensitivity to insulin begins to decline because of the effects of human chorionic somatomammotropin, prolactin, progesterone, estrogen, and cortisol. The mother uses fat stores to meet her energy needs. The higher blood glucose level makes more glucose available for fetal energy needs and stimulates the pancreas of a healthy woman to produce additional insulin. Inadequate insulin production results in gestational diabetes (see Chapter 26).
Adrenal Glands
During pregnancy, significant changes occur in two adrenal hormones: cortisol and aldosterone. Free (unbound) cortisol, the metabolically active form, is elevated. Cortisol regulates carbohydrate and protein metabolism. It stimulates gluconeogenesis (formation of glucose from noncarbohydrate sources such as amino or fatty acids) whenever the supply of glucose is inadequate to meet the mother’s needs for energy.
Aldosterone regulates the absorption of sodium from the distal tubules of the kidneys. It increases during pregnancy to overcome the salt-wasting effects of progesterone to maintain the necessary level of sodium in the greatly expanded blood volume and to meet the needs of the fetus. Aldosterone is closely related to water metabolism.
Changes Caused by Placental Hormones
Human Chorionic Gonadotropin
In early pregnancy, human chorionic gonadotropin (hCG) is produced by the trophoblastic cells that surround the developing embryo. The rapid increase of this hormone stimulates the corpus luteum to produce progesterone and estrogen until the placenta is sufficiently developed to assume that function at about 10 to 12 weeks after conception (Blackburn, 2008). It also causes a positive pregnancy test result.
Estrogen
In early pregnancy, estrogen is produced by the corpus luteum. It is produced primarily by the placenta for the remainder of pregnancy. Estrogen has numerous functions during pregnancy: (1) It stimulates uterine growth and increases blood supply to uterine vessels; (2) it aids in developing the ductal system in the breasts in preparation for lactation; and (3) it is associated with hyperpigmentation, vascular changes in the skin, increased activity of the salivary glands, and hyperemia of the gums and nasal mucous membranes.
Progesterone
Progesterone is produced first by the corpus luteum and then by the fully developed placenta. The major functions include:
• Maintaining the endometrial layer for implantation of the fertilized ovum
• Preventing spontaneous abortion by relaxing the smooth muscles of the uterus
• Preventing tissue rejection of the fetus
• Stimulating the development of the lobes and lobules in the breast in preparation for lactation
• Increasing respiratory sensitivity to carbon dioxide, stimulating ventilation
• Suppressing the immunologic response, preventing rejection of the fetus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree