Percutaneous Administration
Objectives
Key Terms
creams ( ) (p. 105)
) (p. 105)
lotions ( ) (p. 105)
) (p. 105)
aqueous (ey-kwee-uhs) (p. 105)
ointments ( ) (p. 105)
) (p. 105)
dressings ( ) (p. 105)
) (p. 105)
seven RIGHTS (p. 106)
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
The routes of drug administration can be classified into three categories: enteral, parenteral, and percutaneous. The term percutaneous administration refers to the application of medications to the skin or mucous membranes for absorption. The absorption of topical medications can be influenced by the drug’s concentration, how long the medication is in contact with the skin, the size of the affected area, the thickness of the skin, the hydration of the tissues, and the degree of skin disruption. Methods of percutaneous administration include the following: the topical application of ointments, creams, powders, or lotions to the skin; the instillation of solutions onto the mucous membranes of the mouth, eye, ear, nose, or vagina; and the inhalation of aerosolized liquids or gases for absorption through the lungs. The primary advantage of the percutaneous route is that the action of the drug, in general, is localized to the site of application, which reduces the incidence of systemic side effects. Unfortunately, the medications are sometimes messy and difficult to apply. In addition, they usually have a short duration of action and thus require more frequent reapplication.
Administration of Topical Medications to the Skin
Dose Forms
Creams
Creams are semisolid emulsions that contain medicinal agents for external application. The cream base is generally nongreasy, and it can be removed with water. Many over-the-counter creams are used as moisturizing agents.
Lotions
Lotions are aqueous (water-based) preparations that contain suspended materials. Lotions are commonly used as soothing agents to protect the skin and to relieve rashes and itching. Some lotions have a cleansing action, whereas others have an astringent or drawing effect. To prevent increased circulation and itching, lotions should be gently but firmly patted on the skin rather than rubbed into the skin. Shake all lotions thoroughly immediately before application, and use them sparingly to avoid waste.
Ointments
Ointments are semisolid preparations of medicinal substances in an oily base, such as lanolin or petrolatum. This type of preparation can be applied directly to the skin or mucous membrane, and it generally cannot be removed easily with water. The base helps to keep the medicinal substance in prolonged contact with the skin.
Dressings
There are several types of dressings used to treat wounds, such as dry gauze sponges, nonadherent gauze dressings (e.g., Telfa), self-adhesive transparent films that act as a second skin (e.g., OpSite), and hydrocolloid dressings (e.g., DuoDERM). Hydrogel dressings are used on partial-thickness and full-thickness wounds and on skin that has been damaged by burns. There are also exudate absorbers such as calcium alginate dressings (e.g., AlgiDERM, Kaltostat, Sorbsan) manufactured from seaweed that can be used on infected wounds.
Wound care products and wound care have become a complex science. (Refer to fundamentals of nursing, medical-surgical nursing, and geriatric nursing textbooks for discussions of the principles of wound care.) Dressing recommendations for treating pressure ulcers are available from the Agency for Health Care Research and Quality, the Public Health Service, and the U.S. Department of Health and Human Services.
Procedure Protocol
The term procedure protocol will be used as part of the medication administration technique for this text. This term includes the following nursing interventions:
1 Perform hand hygiene, and assemble appropriate equipment.
2 Use the seven RIGHTS of medication preparation and administration (see p. 100) throughout the procedure:
3 Provide privacy for the patient, and give a thorough explanation of the procedure.
In addition, a nurse should perform a premedication assessment before applying any topical preparation. See individual drug monographs for more information.
Administration of Creams, Lotions, and Ointments
Topical preparations can be used to do the following:
• Relieve localized signs and symptoms, such as itching and rash
• Provide a protective barrier
• Reduce a thickening of the skin, such as that involved with callus formation
Equipment
Sites
Skin surfaces affected by the disorder being treated.
Techniques
1 Follow the procedure protocol described previously.
4 Application: Wear gloves during the application process. Many of the agents used may be absorbed through the skin of both the patient and the person who is applying the medication.
• Lotions: Shake well until a uniform appearance of the suspension is obtained.
Patient Teaching
1 If appropriate, teach the patient to apply the medication and dressings.
3 When dressings are ordered, suggest the purchase of gauze and other necessary supplies.
4 Stress gentleness and moderation with regard to the amount of medication to be applied.
5 Emphasize that the patient must avoid touching or scratching the affected area.
Documentation
Provide the RIGHT DOCUMENTATION of the medication administered and the patient’s response to drug therapy.
Patch Testing For Allergens
Objectives
Key Terms
Patch testing is a method that is used to identify a patient’s sensitivity to contact materials (e.g., soaps, pollens, dyes). The suspected allergens (antigens) are placed in direct contact with the skin surface and covered with nonsensitizing, nonabsorbent tape. Unless pronounced irritation appears, the patch is usually left in place for 48 hours and then removed. The site is left open to air for 15 minutes and then “read.” A positive reaction is noted by the presence of redness and swelling, called a wheal, which indicates an allergy to the specific allergen. It may be necessary to read the areas after 3 days and again after 7 days to detect delayed reactions.
Intradermal tests may also be used to determine allergenicity to specific antigens. See Chapter 11 for more information about the intradermal administration of allergens.
Perform premedication assessments. See individual drug monographs.
Equipment
Sites
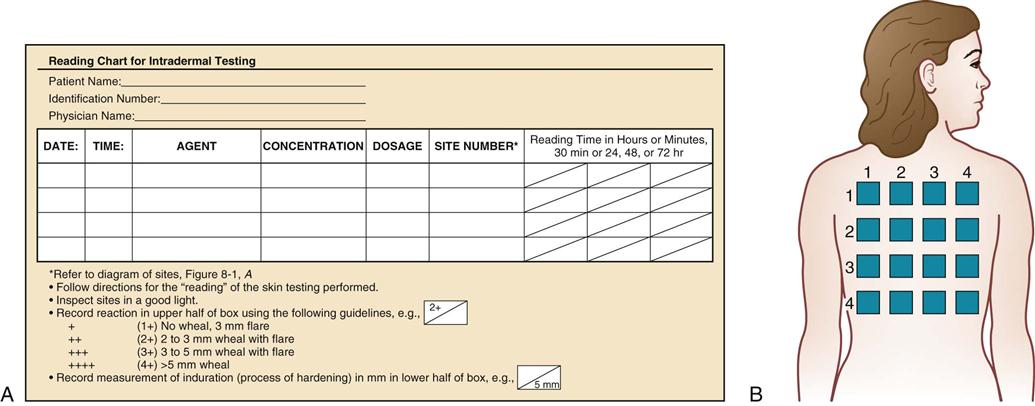
The back, arms, or thighs are commonly used. (DO NOT use the face or areas that are susceptible to friction from clothing.) Selected areas are spaced 2 to 3 inches apart. The type of allergen applied and the site of application are documented on the patient’s chart (Figure 8-1). Hair is clipped from sites to ensure that the allergen is kept in close contact with the skin surface, thereby preventing a false-negative reaction.
Technique
CAUTION: DO NOT begin any type of allergy testing unless emergency equipment is available in the immediate area in case of an anaphylactic response. Personnel should be familiar with the procedure to follow if an emergency does arise.
2 Follow the procedure protocol described on p. 106.
5 Prepare the designated solutions with the use of aseptic technique.
7 The following methods may be used:
• After application, follow institutional policy for covering the test site.
| + (1+) | No wheal, 3-mm flare |
| ++ (2+) | 2- to 3-mm wheal with flare |
| +++ (3+) | 3- to 5-mm wheal with flare |
| ++++ (4+) | >5-mm wheal |
Patient Teaching
Documentation
Provide the RIGHT DOCUMENTATION of the allergen testing sites and the patient’s responses to the allergens that were applied.
Administration of Nitroglycerin Ointment
Objectives
Dose Form
Nitroglycerin ointment (Nitro-Bid) provides relief of anginal pain for several hours longer than sublingual preparations. When properly applied, nitroglycerin ointment is particularly effective against nocturnal attacks of anginal pain. Specific instructions for nitroglycerin ointment are reviewed in this text, because it is the only ointment that is currently available for which dosage is critical to the success of use (see Chapter 25).
Perform premedication assessments. See individual drug monographs.
Equipment
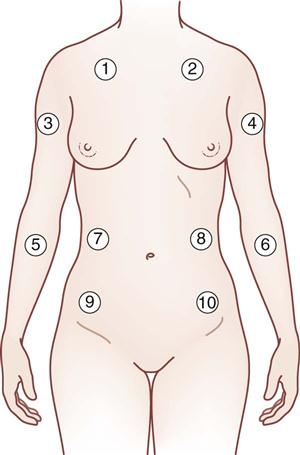
Sites
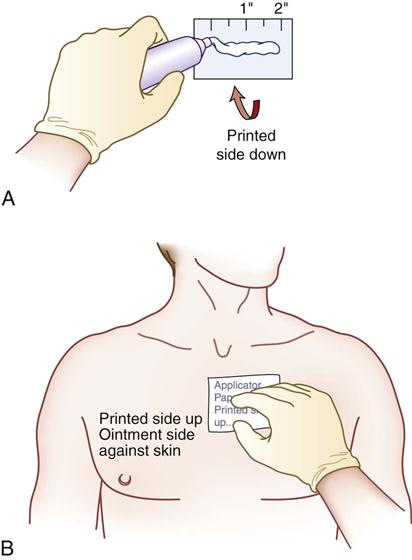
Any area without hair may be used. Most people prefer the chest, flank, or upper arm area (Figure 8-2). DO NOT shave an area to apply the ointment; shaving may cause skin irritation.
Techniques
1 Follow the procedure protocol described on p. 106.
4 Lay the dose-measuring applicator paper with the print side DOWN on the site (Figure 8-3, A). The ointment will smear the print.
5 Squeeze a ribbon of ointment of the proper length onto the applicator paper.
6 Place the measuring applicator on the skin surface at the site chosen on the rotation schedule, ointment side DOWN. Spread in a thin, uniform layer under the applicator. DO NOT RUB IN. Leave the paper in place. NOTE: Use of the applicator paper allows you to measure the prescribed dose and prevents absorption through the fingertips as you apply the medication (see Figure 8-3, B).
8 Remove gloves and dispose of them in accordance with institutional policy.
Patient Teaching
1 Help the patient learn how to apply the ointment.
5 When terminating the use of this topical ointment, the dosage and frequency of application should be gradually reduced over a 4- to 6-week period. Tell the patient to contact the health care provider if adjustment is thought to be necessary. Encourage the patient not to discontinue the medication abruptly (see Chapter 25).
Documentation
Provide the RIGHT DOCUMENTATION of the medication administration and the patient’s responses to drug therapy.
Administration of Transdermal Drug Delivery Systems
Objective
Key Term
Dose Form
The transdermal patch provides for the controlled release of a prescribed medication (e.g., nitroglycerin, clonidine, estrogen, nicotine, scopolamine, fentanyl) through a semipermeable membrane for several hours to 3 weeks when applied to intact skin. The dose released depends on the surface area of the disk in contact with the skin surface and the individual drug. See specific monographs for the onset and duration of action of drugs that make use of this delivery system.
Perform premedication assessments. See individual drug monographs.
Equipment
Sites
Any area without hair may be used. Most people prefer the chest, flank, or upper arm area. Develop a rotation schedule for use (see Figure 8-2 for an example of a nitroglycerin rotation schedule). See manufacturer’s recommendations for location and frequency of application of patches other than nitroglycerin.
Techniques
1 Follow the procedure protocol described on p. 106.
5 Apply the small adhesive topical disk. Figure 8-4 illustrates nitroglycerin being applied to one of the sites recommended by the rotation schedule. The frequency of application depends on the specific medication being applied via the transdermal disk and the duration of action of the prescribed medication. Nitroglycerin is applied once daily, whereas fentanyl is reapplied every 3 days; clonidine and Ortho Evra are reapplied once every 7 days. Hormone replacement therapies may be applied every 4 to 7 days.
6 Remove gloves and dispose of them in accordance with institutional policy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 ) (
) ( ) (
) (