Drugs Used to Treat Dysrhythmias
Objectives
1 Describe the anatomic structures and conduction system of the heart.
2 Differentiate between the atrial dysrhythmias and the ventricular dysrhythmias.
6 Cite common adverse effects that may be observed with the administration of antidysrhythmic drugs.
Key Terms
conduction system ( ) (p. 386)
) (p. 386)
dysrhythmia ( ) (p. 386)
) (p. 386)
atrial flutter ( ) (p. 387)
) (p. 387)
atrial fibrillation ( ) (p. 387)
) (p. 387)
paroxysmal supraventricular tachycardia (PSVT) (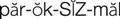
 ) (p. 387)
) (p. 387)
atrioventricular blocks ( ) (p. 387)
) (p. 387)
tinnitus (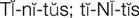 ) (p. 393)
) (p. 393)
Dysrhythmias
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
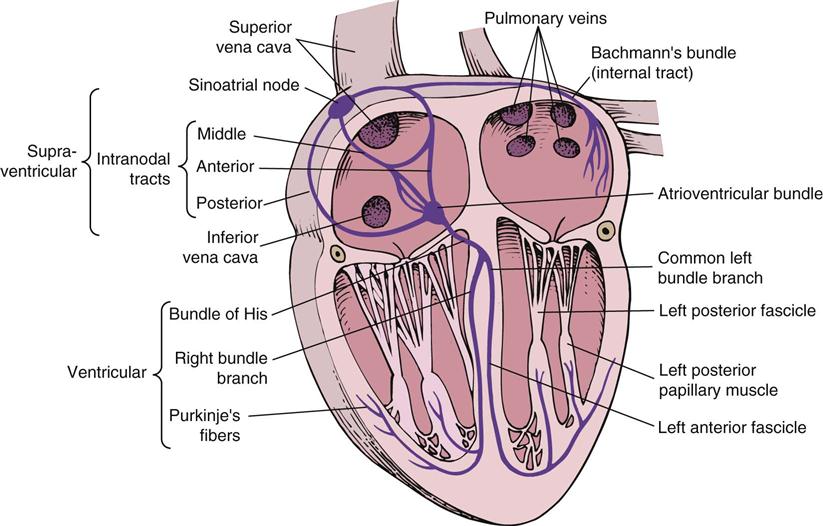
The function of the heart is to sustain life by rhythmically pumping blood to all the vital organs and the rest of the body’s tissues. The conduction system, or electrical system, of the heart is the anatomic structure that controls the sequence of muscle contractions so that an optimal volume of blood is pumped from the heart with each beat (Figure 24-1).![]() The conduction system is composed of nerve fibers that carry the electrical impulses to the cardiac muscle, causing it to contract.
The conduction system is composed of nerve fibers that carry the electrical impulses to the cardiac muscle, causing it to contract.
In the normal heart, a contraction of the heart muscle begins in the pacemaker cells of the sinoatrial (SA) node. The electrical wave passes through the conduction system in the atrial muscle and causes it to contract, forcing blood from the atrial chambers into the ventricles below. The electrical current then enters the atrioventricular (AV) node, which focuses and conducts an electrical current through the bundle of His and Purkinje fibers to the ventricular muscle tissue. The muscle contracts from the apex upward, causing blood to be pumped from the right ventricle into the pulmonary artery to the lungs and from the left ventricle into the aorta to the rest of the body.
A dysrhythmia (sometimes called an arrhythmia) occurs when there is a disturbance of the normal electrical conduction, resulting in an abnormal heart muscle contraction or heart rate. All people have an occasional irregular contraction of the heart. The danger is the frequency with which the dysrhythmia occurs because the heart muscle loses its efficiency in pumping an adequate volume of blood. Thus certain types of dysrhythmias can produce additional dysrhythmias that can stop the heart from pumping even though it continues to beat for a short time (fibrillation). A person may sense an abnormal contraction (dysrhythmia) because of a flip-flop or racing of the heart. A nurse may also suspect that a patient is having dysrhythmia because of an irregular pulse. Dysrhythmias, however, must be identified with the aid of an electrocardiogram (ECG), which provides a tracing of the electrical activity of the heart.
Dysrhythmias are caused by the firing of abnormal pacemaker cells, blockage of normal electrical pathways, or a combination of both. Normally, the rate and rhythm of electrical activity and muscle contraction are regulated by the pacemaker cells of the SA node. High emotional stress, ischemia (see Chapter 25), or heart failure (see Chapter 28) may trigger normally quiet pacemaker cells in areas of the heart other than the SA or AV nodes to fire. This sends an electrical impulse out of sequence with those from the normal pacemaker cells, causing an irregular muscular contraction, sometimes sensed as a flip-flop of the heart. The second cause of a dysrhythmia is a partial obstruction of the normal conduction pathway, causing an irregular flow of electrical impulses that results in an irregular pattern of muscle contractions. This is sometimes called a reentrant dysrhythmia. Normally, healthy heart tissue has mechanisms that protect against reentrant dysrhythmias. Various forms of heart disease cause changes in the conduction pathways that allow continuous reentrant dysrhythmias.
Dysrhythmias are most commonly classified by origin within the heart tissues. Those that develop above the bundle of His (see Figure 24-1) are called supraventricular. Examples of supraventricular dysrhythmias are atrial flutter, atrial fibrillation, premature atrial contractions(PACs), sinus tachycardia, sinus bradycardia, and paroxysmal supraventricular tachycardia (PSVT). Junctional dysrhythmias are those developing near or within the AV node. Dysrhythmias developing below the bundle of His are referred to as “ventricular dysrhythmias.” These include premature ventricular contractions (PVCs), ventricular tachycardia (VT), and ventricular fibrillation (VF). Dysrhythmias that result from obstruction of conduction pathways are described by location (e.g., supraventricular or ventricular, left or right bundle branches). Atrioventricular blocks can be subclassified by degree of block: first degree = partial block, delayed AV conduction; second degree = partial block, with occasional blocked beats; and third degree = complete block, in which the atria and ventricles function independently of each other. Another method of classification is based on heart beat rate: bradyarrhythmia (more than 60 beats/min) or tachyarrhythmia (more than 100 beats/min).
The tissues of the electrical system can be classified by conduction rate depending on whether calcium or sodium ions create the stimulus for muscle contraction. The SA and AV nodes depend on calcium ions for electrical conduction and are referred to as “slow conduction fibers.” The atrial muscle, His-Purkinje system, and ventricular muscle depend on sodium for contraction and are sometimes referred to as “fast conduction fibers.”
Treatment for Dysrhythmias
When a dysrhythmia is suspected, a patient is often admitted to a coronary care unit, where wire leads are placed in appropriate locations to provide continuous electrocardiographic monitoring (telemetry). A combination of the physical examination, patient history, and electrocardiographic pattern is used to diagnose the underlying cause of the dysrhythmia. The goal of treatment is to restore normal sinus rhythm and normal cardiac function and prevent recurrence of life-threatening dysrhythmias.
Drug Therapy for Dysrhythmias
Actions
Antidysrhythmic agents are complex agents with multiple mechanisms of action. They are classified according to their effects on the electrical conduction system of the heart (Table 24-1). Class I agents act as myocardial depressants by inhibiting sodium ion movement. The Class Ia agents prolong the duration of the electrical stimulation on cells and the refractory time between electrical impulses. Class Ib agents shorten the duration of the electrical stimulation and the time between the electrical impulses. Class Ic antidysrhythmics are the most potent myocardial depressants and slow the conduction rate through the atria and the ventricles.
Table 24-1
Classification of Antidysrhythmic Agents
| CLASS | DRUGS | EFFECT | |||
| MECHANISM | CV | RP | AM | ||
| Ia | quinidine (Quinidine) procainamide (Procanbid) disopyramide (Norpace) | Na channel blockers (intermediate-acting) | ↓ | — | ↓ |
| Ib | lidocaine (Xylocaine) mexiletine (Mexitil) | Na channel blockers (quick-acting) | ↓/↔ | ↓ | ↓ |
| Ic | flecainide (Tambocor) propafenone (Rythmol) | Na channel blockers (slow-acting) | ↓ | ↔ | ↓ |
| II | propranolol (Inderal) esmolol (Brevibloc) metoprolol (Lopressor) | Beta blockers | ↓ | — | ↓ |
| III | amiodarone (Cordarone) sotalol (Betapace) ibutilide (Corvert) dofetilide (Tikosyn) | K channel blockers | /↔ | — | ↔ |
| IV | verapamil (Calan) diltiazem (Cardizem) | Ca channel blockers | ↓ | — | ↓ |
| Miscellaneous | digoxin (Lanoxin) adenosine (Adenocard) dronedarone (Multaq) | Vagal stimulation Slows conduction | ↓ | ↓/↔ | ↓ |
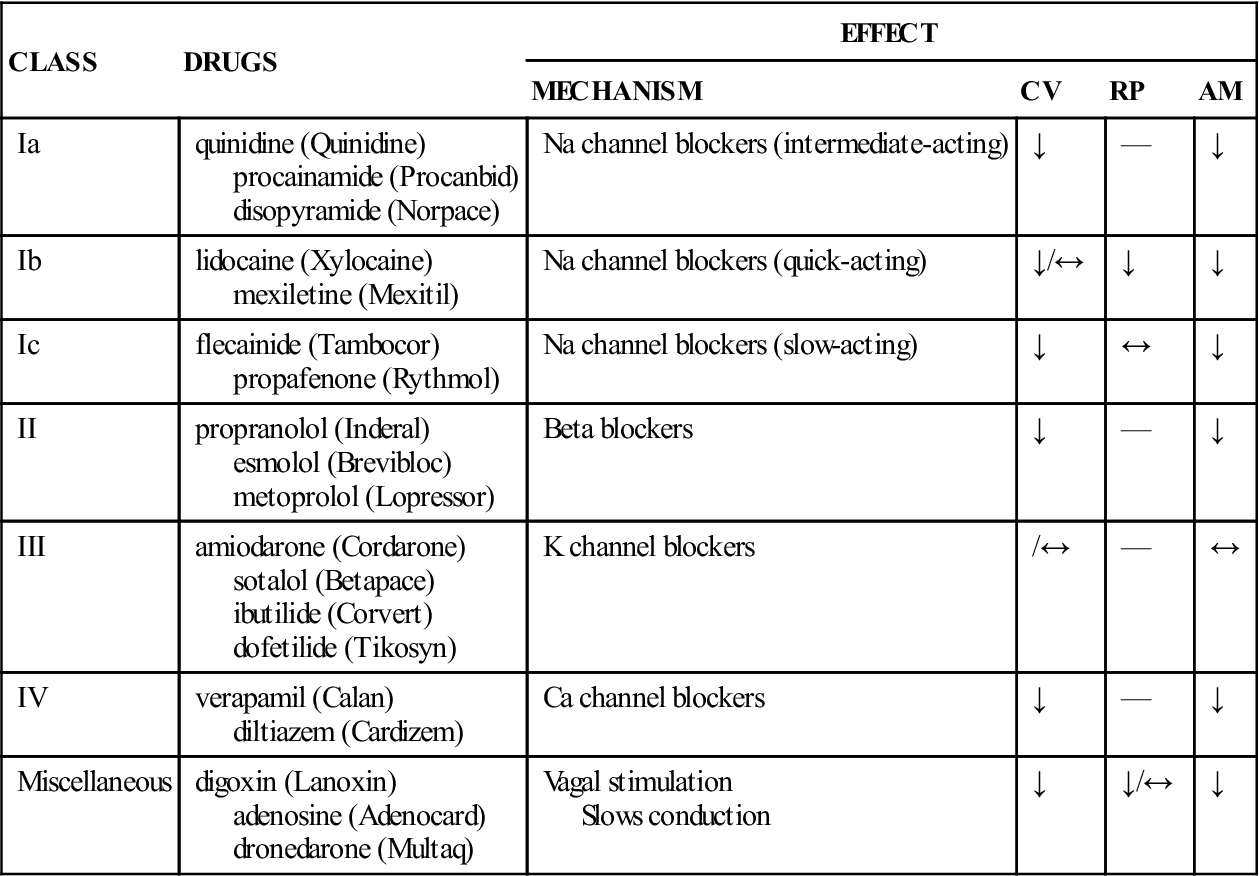
AM, automaticity; Ca, calcium; CV, conduction velocity; Na, sodium; RP, refractory period.
Class II agents are beta-adrenergic blocking agents (beta blockers). Many dysrhythmias are caused by stimulation of the beta cells of the sympathetic nervous system of the heart. Class III agents slow the rate of electrical conduction and prolong the time interval between contractions by blocking potassium channels. Class IV agents block calcium ion flow, prolonging duration of the electrical stimulation and slowing AV node conduction.
Uses
See individual drug monographs for uses of antidysrhythmic agents.
 Nursing Implications for Antidysrhythmic Agents
Nursing Implications for Antidysrhythmic Agents
The information that nurses assess relative to the cardinal signs of cardiovascular disease can provide a basis for subsequent evaluation of the patient’s response to the therapeutic modalities prescribed.
Assessment
Dysrhythmias are initially assessed by electrocardiographic monitoring. Various types of telemetry monitoring equipment are available. It is vitally important for the nurse not to rely completely on computerized systems, but rather to perform frequent patient assessments while viewing the telemetry system as an adjunct to astute nursing observations. A 24-hour ambulatory ECG (Holter monitor), electrophysiologic studies (EPS), exercise electrocardiography, and laboratory values are used to analyze and diagnose the patient’s myocardial status.
Patients are usually admitted to the coronary care unit, where specialized monitoring equipment is available for continuous surveillance of the patient. The nurses in this care unit have advanced education in cardiac physiology and the nursing care of these individuals. (See a general medical-surgical nursing text or critical care textbook for an in-depth explanation of care of the patient with a dysrhythmia.)
Medication History.
Obtain details of all medications prescribed and being taken. Tactfully find out if the prescribed medications are being taken regularly and if not, why.
History of Six Cardinal Signs of Cardiovascular Disease
Basic Mental Status.
Identify the person’s level of consciousness and clarity of thought. Both of these factors are indicators of adequate or inadequate cerebral perfusion. Subsequent regular observations for these data should be made so that apparent improvement or deterioration can be assessed. Schedule basic neurologic assessments at least once per shift.
Vital Signs.
Vital signs should be taken as often as necessary to monitor the patient’s status.
Auscultation and Percussion.
Nurses with advanced skills can perform auscultation and percussion to note changes in heart size and heart and lung sounds. (See a medical-surgical nursing text for details about performing these skills.) As appropriate to nursing skills, note changes in cardiac rhythm, heart rate, changes in heart sounds, or murmurs.
Laboratory and Diagnostic Tests.
Review laboratory tests and report abnormal results to the health care provider promptly. Such tests may include levels of serum electrolytes, especially potassium, calcium, magnesium, and sodium; arterial blood gases such as pH, PO2, PCO2, and HCO3−; coagulation studies to evaluate the blood clotting; serum enzyme levels, including aspartate aminotransferase (AST), creatine kinase (CK-MB), troponin, D-dimer, and lactic dehydrogenase (LDH); serum lipid levels (e.g., cholesterol, triglycerides); electrocardiography; chest radiography; nuclear cardiography; cardiac catheterization; EPS testing; and exercise treadmill.
Examine urinalysis reports and perform hourly monitoring of intake and output (I&O) as ordered. Report output that is less than intake or is below 30 to 50 mL per hour for the adult patient. Monitor other renal function tests such as the blood urea nitrogen (BUN) and serum creatinine. Abnormalities of these tests or insufficient hourly output may indicate inadequate renal perfusion.
Implementation
 Patient Education and Health Promotion
Patient Education and Health Promotion
Fostering Health Maintenance
Written Record.
Enlist the patient’s aid in developing and maintaining a written record of monitoring parameters (e.g., pulse rate, blood pressure, degree of dyspnea and precipitating causes, chest pain, edema) (see Patient Self-Assessment Form for Cardiovascular Agents on the Evolve Web![]() site for this text). Complete the Premedication Data column for use as a baseline to track response to drug therapy. Ensure that the patient understands how to use the form and instruct the patient to bring the completed form to follow-up visits. During follow-up visits, focus on issues that will foster adherence to the therapeutic interventions prescribed.
site for this text). Complete the Premedication Data column for use as a baseline to track response to drug therapy. Ensure that the patient understands how to use the form and instruct the patient to bring the completed form to follow-up visits. During follow-up visits, focus on issues that will foster adherence to the therapeutic interventions prescribed.
Drug Class: Class Ia Antidysrhythmic Agents
Actions
Disopyramide is a class Ia antidysrhythmic agent.
Uses
Disopyramide is used to treat life-threatening premature ventricular tachycardia and ventricular tachycardia. It may be used in digitalized and nondigitalized patients. It is a useful drug alternative to quinidine or procainamide when patients develop an intolerance to, or serious adverse effects from, these agents. It should not be used in cardiogenic shock, second- or third-degree block (without a pacemaker already in place), or Q-T prolongation.
Therapeutic Outcome
The primary therapeutic outcome expected from disopyramide therapy is conversion of dysrhythmia to normal sinus rhythm.
 Nursing Implications for Disopyramide
Nursing Implications for Disopyramide
Premedication Assessment
Availability
PO: 100- and 150-mg capsules; 100- and 150-mg controlled-release capsules.
Dosage and Administration
PO: Dosage is individualized but is usually 400 to 800 mg/day. Initial dosage is 100 mg every 6 to 8 hours. Making adjustments gradually, the recommended adult dosage schedule is 150 mg every 6 hours. If body weight is less than 110 lb (50 kg), the recommended dosage is 100 mg every 6 hours. Therapeutic blood level is 2 to 4 mg/L.
Monitoring
Common Adverse Effects
Oropharyngeal
Dry Mouth, Nose, Throat.
Suggest frequent mouth rinses or sucking on ice chips or hard candy to relieve symptoms.
Serious Adverse Effects
Cardiovascular
Myocardial Toxicity.
Hold the medication and report bradycardia or increasing signs of heart failure. Monitoring of the ECG for various types of dysrhythmias may be indicated as ordered by the physician.
Genitourinary
Urinary Hesitancy.
Tell the patient that hesitancy in starting to urinate may occur. Suggest running tap water or immersing hands in water as a means to stimulate urination. Report decreased urinary output and bladder distention. In the hospitalized patient, record input and output. Palpate the area of the symphysis pubis to assess for distention.
Gastrointestinal
Constipation With Distension and Flatus.
Report difficulties in defecation to the physician. Assess distention by measuring abdominal girth, as appropriate. Assess ability to expel flatus.
Drug Interactions
Drugs That Enhance Therapeutic and Toxic Effects.
These include procainamide, quinidine, digoxin, erythromycin, clarithromycin, fluoroquinolones (e.g., ciprofloxacin), ziprasidone, and beta blockers (e.g., propranolol, atenolol). Monitor for increases in severity of drug effects such as bradycardia and hypotension.
Drugs That Enhance Therapeutic and Toxic Effects.
Do not administer disopyramide within 48 hours before or 24 hours after administration of verapamil.
Drugs That Reduce Therapeutic Effects.
These include phenytoin, barbiturates, primidone, and rifampin. Monitor for an increase in the frequency of the patient’s dysrhythmia.
Drugs That Increase Hypotensive Effects.
These include diuretics and antihypertensive agents. Instruct the patient to rise slowly from a supine position. If symptoms become more severe, report to the health care provider.
Actions
Procainamide is an effective synthetic class Ia antidysrhythmic agent that has many cardiac effects similar to those of quinidine but generally with fewer adverse effects.
Uses
Procainamide is used to treat a wide variety of life-threatening ventricular and supraventricular dysrhythmias, atrial fibrillation, and flutter. It is usually not as effective as quinidine in atrial fibrillation. Procainamide is not recommended for the treatment of asymptomatic PVCs.
Therapeutic Outcome
The primary therapeutic outcome expected from procainamide therapy is conversion of dysrhythmia to normal sinus rhythm.
 Nursing Implications for Procainamide
Nursing Implications for Procainamide
Premedication Assessment
Obtain data relating to the six cardinal signs of cardiovascular disease and assess cardiac rhythm, vital signs, and oxygen saturation to be used as a baseline for subsequent evaluation of response to therapy.
Availability
IV: 100 mg/mL in 10-mL vials and 500 mg/mL in 2-mL vials. (High-alert medication).
Dosage and Administration
Adult: IV: 50 mg/kg/day in four to eight divided doses (every 3 to 6 hours) or by continuous infusion of 2 to 6 mg/min to maintain control of the dysrhythmia.
Patients should have monitoring of the ECG and blood pressure when receiving IV doses of procainamide. If dysrhythmia recurs, suppress the dysrhythmia with bolus therapy, as above, and increase the rate of infusion.
Serum levels of procainamide are determined to measure the amount of procainamide and N-acetyl procainamide (an active metabolite) in the bloodstream. It is important to be consistent in the time of drawing the blood and administering the dose if more than one serum level is to be determined in the same patient. Therapeutic blood levels are 4 to 8 mg/L.
Monitoring
Common Adverse Effects
Neurologic
Drowsiness, Sedation, Dizziness.
Tell patients that they may experience these symptoms early in therapy as the dosage is being adjusted. Instruct patients to use caution in operating power equipment or driving.
Cardiovascular
Hypotension.
Hypotension may be observed while therapy is being initiated, particularly by the IV route. Hypotension is usually transient and can be avoided by rising slowly from supine and sitting positions. However, should the systolic blood pressure fall 15 mm Hg or more, hold the medication and notify the prescriber.
Serious Adverse Effects
Immunologic
Fever, Chills, Joint and Muscle Pain, Skin Eruptions.
Tell patients to report the development of these symptoms. Monitor laboratory reports for leukocyte counts and the antinuclear antibody (ANA) titer.
Drug Interactions
Drugs That Enhance Therapeutic and Toxic Effects.
These include digoxin, cimetidine, ranitidine, quinidine, trimethoprim, amiodarone, fluoroquinolones (e.g. ciprofloxacin), ziprasidone, and beta-adrenergic blocking agents (e.g., nadolol, propranolol). Monitor for an increase in severity of adverse effects such as bradycardia and hypotension.
Neuromuscular Blockade, Respiratory Depression.
Procainamide may potentiate the neuromuscular blockade induced by these agents. These agents include surgical muscle relaxants (e.g., tubocurarine, succinylcholine) and aminoglycoside antibiotics (e.g., tobramycin, gentamicin, amikacin). Monitor the patient’s respiratory rate and depth. Observe for signs of cyanosis and additional dysrhythmia.
Patients who are on respirators may require additional time to be weaned off ventilatory assistance.
Hypotension With Diuretics and Antihypertensive Agents.
Instruct patients to rise slowly from a supine position. If symptoms begin to recur more frequently, report to the physician.
Actions
Quinidine, originally obtained from cinchona bark, has been used as an antidysrhythmic agent for several decades. It is classified as a class Ia antidysrhythmic agent, working on the muscle of the heart and stabilizing the rate of conduction of impulses. It slows the heart and changes a rapid irregular pulse to a slow regular pulse.
Uses
Quinidine is used most often to suppress atrial fibrillation, atrial flutter, PSVT and ventricular tachycardia, and life-threatening PVCs. Use with extreme caution in patients with digitalis intoxication or heart block.
Therapeutic Outcome
The primary therapeutic outcome expected from quinidine therapy is conversion of dysrhythmia to normal sinus rhythm.
 Nursing Implications for Quinidine
Nursing Implications for Quinidine
Premedication Assessment
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 )
) )
) )
) )
)