Immunology
Objectives
After completing this chapter you should be able to:
Fundamental Concepts
1. Explain the immune process.
2. Differentiate between cell-mediated immunity and humoral immunity.
3. List and match the classes of immunoglobulins (antibodies) with their locations and/or functions.
4. List the four ways to acquire adaptive immunity.
5. Discuss the principles of in vivo and in vitro immunology tests as they relate to allergy testing.
CLIA-Waived Immunology Tests
Advanced Concepts
Key Terms
agglutination clumping together of blood cells or latex beads caused by antibodies adhering to their antigens
allergen an antigen that causes an allergic reaction
antibodies immunoglobulins produced specifically to destroy foreign invaders
antigens substances that are perceived as foreign to the body and elicit an antibody response
autoimmune diseases destructive tissue diseases caused by antibody/self-antigen reactions
cell-mediated immunity T lymphocytic cell response to antigens
chromatographic pertaining to a visual color change that appears when an enzyme-linked antibody/antigen reaction takes place
complement proteins proteins that stimulate phagocytosis and inflammation and are capable of destroying bacteria
erythroblastosis fetalis a hemolytic anemia in newborns resulting from maternal–fetal blood group incompatibility
helper T cells (TH4 or CD4) antigen-activated lymphocytes that stimulate other T cells and help B cells produce their antibodies
heterophile antibody antibody that appears during an Epstein–Barr viral infection (mononucleosis) that has an unusual affinity to antigens on sheep red cells
histamine compound released by injured cells that causes the dilation of blood vessels
iFOB immunoassayed fecal occult blood
in vitro within a laboratory apparatus
in vivo within a host or living organism
memory B cells antigen-activated B lymphocytes that remember an identified antigen for future encounters
memory T cells antigen-activated T lymphocytes that remember an antigen for future encounters
mucous membrane thin sheets of tissue that line the internal cavities and canals of the body and serve as a barrier against the entry of pathogens into the body
natural killer cells special type of lymphocyte that attacks and destroys infected cells and cancer cells in a nonspecific way
normal flora nonpathogenic microorganisms that normally inhabit the skin and mucous membranes
passive immunity short-term acquired immunity created by antibodies received naturally through the placenta (or the colostrum to an infant) or artificially by injection
phagocytes cells capable of engulfing and ingesting microorganisms and cellular debris
phagocytosis process of engulfing and digesting microorganisms and cellular debris
serology branch of laboratory medicine that performs antibody/antigen testing with serum
suppressor T cells antigen-activated lymphocytes that inhibit T and B cells after a sufficient number of cells have been activated
titer a quantitative test that measures the amount of antibody that reacts with a specific antigen
wheal raised induration
 FUNDAMENTAL CONCEPTS
FUNDAMENTAL CONCEPTS
Overview of Immunology
The immune system is a remarkable defense system that protects the human body against invading pathogens, toxins, allergens, and cancer cells. When the body is under attack by any of these invaders, it has a full arsenal of defenses to destroy the invader, as well as protect itself from future attacks. A key ingredient in this defense mechanism is the body’s production of antibodies (immunoglobulins produced specifically to destroy foreign invaders). These antibodies are produced after the body detects the presence of specific antigens (substances that are perceived as foreign to the body). Once antibodies are produced, they attack the antigens, forming an antibody/antigen complex that destroys or renders the invader harmless.
Biotechnology research has made it possible to detect and measure specific antibodies and their specific antigens in blood and body fluids. Antibody/antigen testing is a rapidly expanding laboratory science called immunology. Because antibodies are usually found in serum, the laboratory department performing antibody/antigen testing may also be referred to as the serology department.
The science of immunology dates to the 1500s, when it was recorded that China had developed a technique of exposing individuals to a powder made from smallpox scabs to produce protection against the disease. The thought was that if children or young adults were exposed in a healthy state, the disease would not be as devastating; unfortunately, that did not always occur. In the late 1700s, Edward Jenner, an English country doctor, found that injecting individuals with material from cowpox provided effective protection against smallpox. This preventive process of injecting harmless or killed microorganisms into the body to induce immunity against a potential pathogen was known as vaccination or immunization.
The field of immunology has benefited from a tremendous amount of new research and subsequent knowledge over the past 100 years. In fact, the cells responsible for the body’s immune response were not discovered until the 1960s. Another recent finding is that the body may respond to self-antigens (substances within the body that induce the production of antibodies that attack an individual’s own body tissues; also called autoantigens). Antibody/self-antigen reactions cause a variety of destructive tissue diseases referred to as autoimmune diseases.
The Immune Process
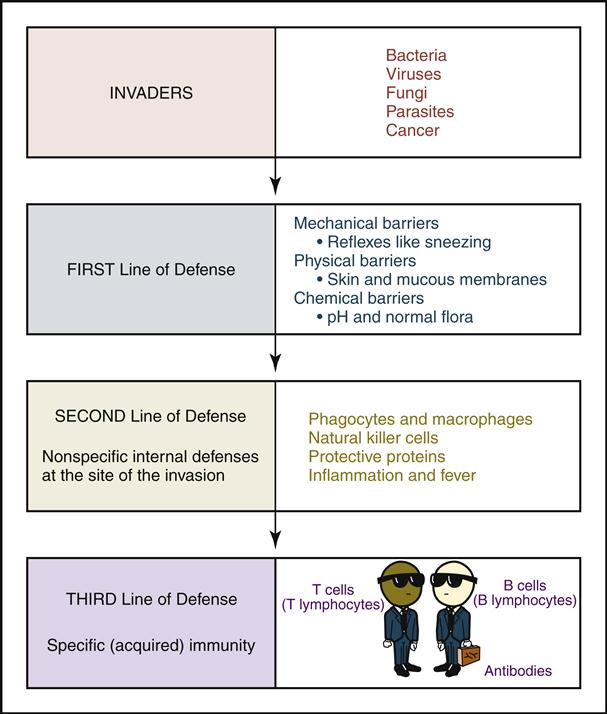
The overall immune process that occurs as the body protects itself against foreign invaders can be viewed as three lines (or battlefields) of defensive mechanisms. Fig. 7-1 is a simplified picture of these lines of defense. The foreign invaders are portrayed at the top of the flowchart. Their goal is to enter the body and cause destruction. The first two lines of defense are considered “nonspecific immunity”—nonspecific because they fight all invaders in the same way. The third line of defense, at the bottom of the illustration, is referred to as “specific immunity” because it intelligently identifies each invader on the basis of its specific antigens. The B cells are then able to produce a specific antibody capable of destroying the invader.
First Line of Defense: Natural Barriers
The first line of defense stops invaders from entering or growing on the body. The skin and mucous membrane (thin sheets of tissue lining the internal cavities and canals) serve as anatomical barriers that prevent the entry of pathogens into the body. They also secrete chemicals that discourage the growth of pathogenic bacteria. These secretions maintain a skin pH of 5.6, which allows the growth of normal flora (nonpathogenic microorganisms that normally inhabit the skin and mucous membranes) while inhibiting the growth of pathogens. In the respiratory tract the mucous membranes contain mucus, which entraps foreign organisms. Coughing and sneezing help move foreign organisms out of the body.
Second Line of Defense: Nonspecific Internal Response
The second line of defense is the internal nonspecific response to all invaders that have passed the natural barriers and entered the body. When invaders break through the barriers, the body quickly responds by sending phagocytes (cells capable of engulfing and ingesting pathogens and cellular debris) to the site of invasion. White blood cells, neutrophils, and monocytes (which become macrophages in the tissue) engulf and ingest the invaders by the process of phagocytosis.
Natural killer cells are a special type of lymphocyte sent to the scene of invasion to attack and destroy the body’s infected cells and cancer cells in a nonspecific way. Protective proteins such as interferons and complement proteins also play an important role at the site of invasion. Interferons are proteins secreted by infected cells to prevent the further replication and spread of the infection into neighboring cells. Complement proteins are proteins that further stimulate phagocytosis and inflammation (reaction of the body to tissue injury or invasion by an infectious agent) and are capable of destroying bacteria. Complement proteins swarm over a bacterium and punch holes in its membrane, causing it to fill with fluid and explode.
At the same time that these defenders are doing their jobs to destroy the invader, the injured tissues are initiating a nonspecific inflammatory response. The clinical signs of inflammation are heat, redness, swelling, and pain. Inflammation begins when histamine is released by the injured cells, causing the dilation of blood vessels. The increased blood flow to the affected areas results in redness and heat. Fluids in the plasma leak into the tissue because of the increased permeability of the vessels, causing the swelling and pain.
The second line of defense is generally seen within the first 12 hours of an infection. For example, the first signs and symptoms of influenza start with swollen glands, sore throat, chills, and fever. These symptoms are the result of an active nonspecific battle against the invaders consisting of the phagocytes, natural killer cells, protective proteins, and the subsequent inflammatory response.
Third Line of Defense: Adaptive or Acquired Immunity
The third line of defense goes into action when the first two lines have failed to bring the invasion under control. It is the “intelligent” identification of the invader based on its antigenic properties. The T cells and B cells work together to produce the specific antibodies that will destroy the invader or render it harmless once and for all. This adaptive process takes 6 to 10 days to accomplish. The T and B cells are also capable of developing immunological memory so that a second encounter with the same organism will induce a heightened immune reaction.
Both these intelligent lymphocytes provide different immunological functions, as described in the following sections.
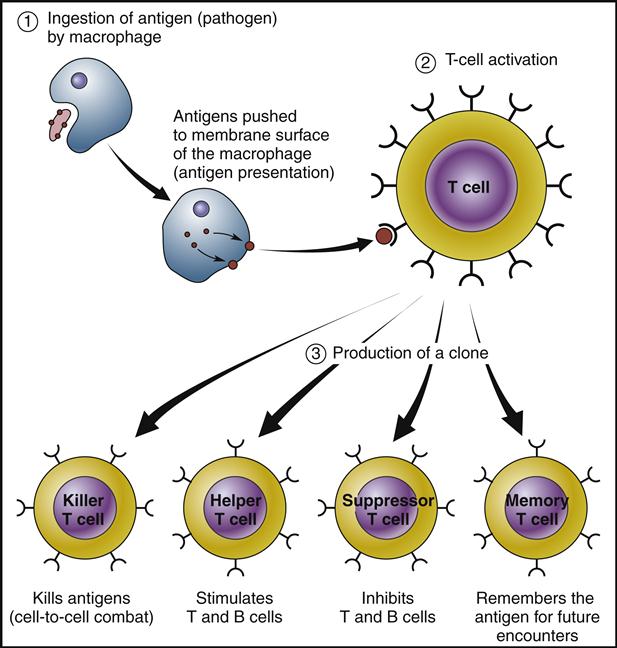
Cell-Mediated Immunity
T cells, small lymphocytes associated with the thymus gland, are involved in cell-mediated immunity. They become involved at the site of the invasion, where they become activated after they receive an antigen presentation from the macrophages (Fig. 7-2).
Once activated, T cells rapidly duplicate themselves into clones that differentiate into the following four subgroups:
Of the lymphocytes circulating in the blood, 70% to 80% are T cells.
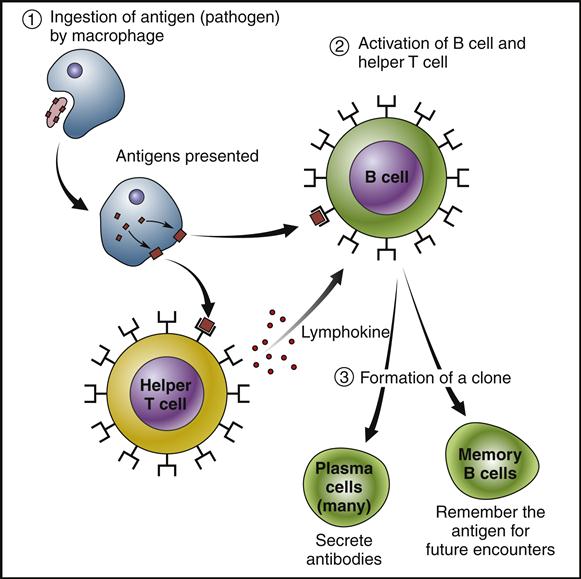
Humoral Immunity (Antibody-Mediated Immunity)
B cells are involved in humoral immunity. Humoral immunity begins with the interaction of a B cell with a specific antigen and the lymphokine (chemicals) from the T helper cell (Fig. 7-3). Once it is activated, it rapidly duplicates into a clone and differentiates into the following two subgroups:
Classes of Antibodies (Immunoglobulins)
Biomedical researchers have found that antibodies are part of the globulin group of proteins that circulate in the blood. Because of their globulin properties, antibodies are referred to as immunoglobulins (Igs). The researchers have classified immunoglobulins into the following groups, based on their shapes, locations, and functions:
• IgE are the immunoglobulins involved in acute allergic reactions.
• IgM are the primary responders in the first encounter with an invading antigen.
• IgG respond to the antigens and allergens in subsequent invading or allergic encounters.
• IgA protect mucous membranes from bacterial and viral infections.
• IgD are involved in lymphocyte activation and suppression.
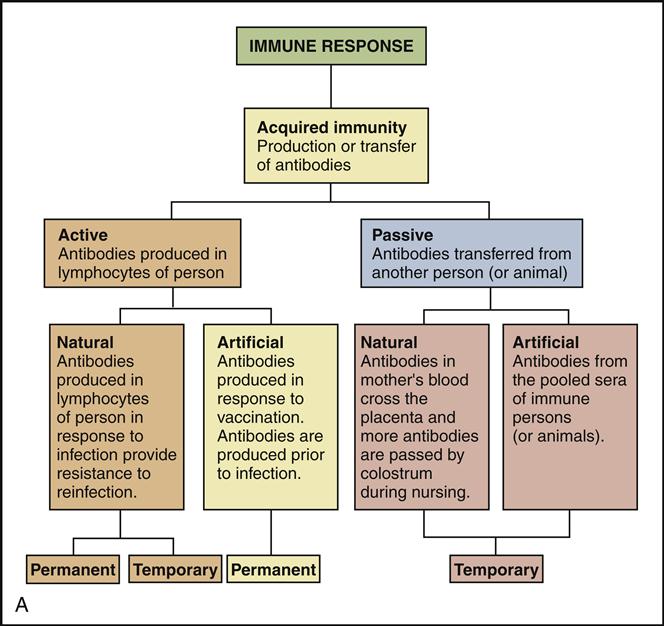
Ways to Acquire Specific Immunity
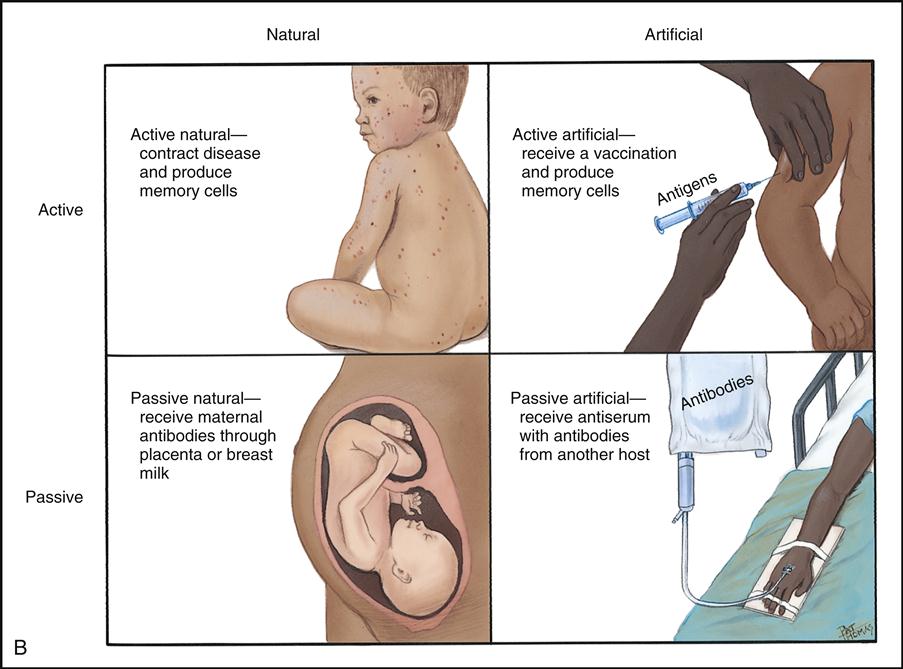
Once a specific antibody is present in the blood, the individual is said to be immune to its particular disease, pathogen, or antigen. There are four ways to acquire specific immunity: (1) active immunity acquired naturally, (2) active immunity acquired artificially, (3) passive immunity acquired naturally, and (4) passive immunity acquired artificially (Fig. 7-4).
Active immunity is long-term protection against future infections that results from the production of antibodies that were formed naturally during an infection or artificially by vaccination. In both cases the antibody is remembered in the memory B cells, making the individual immune to future encounters with the pathogen.
Passive immunity is short-term protection against infections created by antibodies received naturally through the placenta (or the colostrum to an infant) or artificially by the injection of antiserum or gamma globulins. Passive immunity is only temporary.
Two Types of Allergy Testing
In Vivo Testing
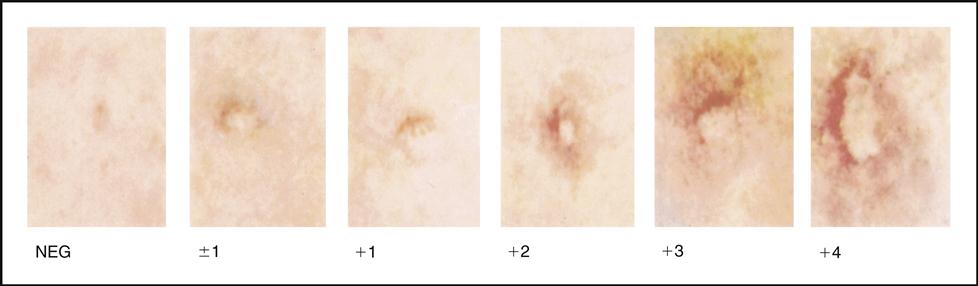
The body is capable of overreacting to antigens by producing too many antibodies (immunoglobulins), resulting in allergic or autoimmune conditions such as asthma, hives, breathing difficulties, and gastrointestinal inflammation. Allergy tests have been performed to visualize the specific reaction between an allergen (an antigen that causes an allergic reaction) and its specific antibody. Tests are done in vivo (within a host or living organism) by injecting or pricking an antigen into the skin and seeing whether a wheal (raised induration) forms in response to the antibody/antigen reaction. Fig. 7-5 shows a negative reaction and various positive reactions to skin tests. Tuberculosis screening tests and allergy skin tests are examples of in vivo immunology tests.
In Vitro Testing
Laboratory immunology tests (also referred to as serology tests) are now being performed in vitro (within the laboratory test tube) outside of the body. It is now available to test the antigen/antibody reaction using only the serum from a tube of blood. Through this testing method, a multiwell plate is coated with various food proteins and/or inhalants that are possible allergens capable of causing allergic reactions. The patient’s serum is then added to each well. If the patient’s serum contains IgE or IgG antibodies to any of the specific food or inhalant proteins, a binding reaction occurs. The degree of antibody–antigen binding depends on the concentration of antibodies present in the patient’s serum. The reaction is then detected through a color change and assessed spectrophotometrically. The wells showing a strong reaction and high level of IgG immunoglobulins will indicate an allergic response to the items in the wells. A typical serological food panel test will indicate possible allergies in the following food groups: dairy, meat/fowl, fruits, fish/crustacea/mollusk, grains, vegetables, spices, herbs.
 CLIA-WAIVED IMMUNOLOGY TESTS
CLIA-WAIVED IMMUNOLOGY TESTS
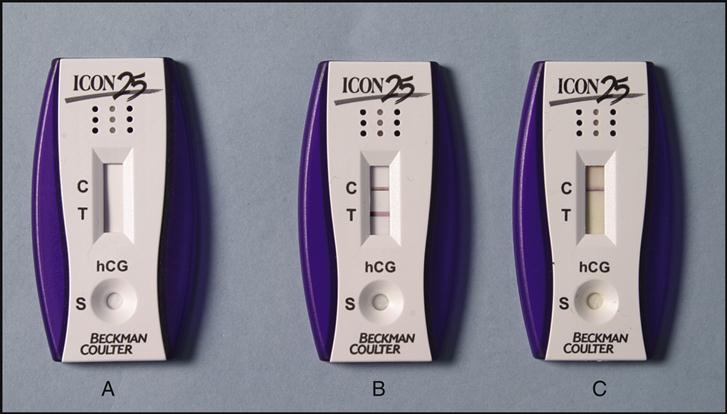
CLIA-Waived Enzyme-Linked Immunoassays
Manufacturers produce a variety of immunology testing devices. In most of these rapid screening tests, a liquid specimen is absorbed and travels across a testing area that enzymatically changes color if an antibody/antigen reaction takes place. The tests typically include an internal control that must also change color to prove the testing device is working. The control area is usually located just beyond the test area to make sure the solution has traveled all the way through the test area. This method is often referred to as a lateral flow immunochromatographic assay. Fig. 7-6 shows the before and after reactions of a positive and negative urine pregnancy test.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree