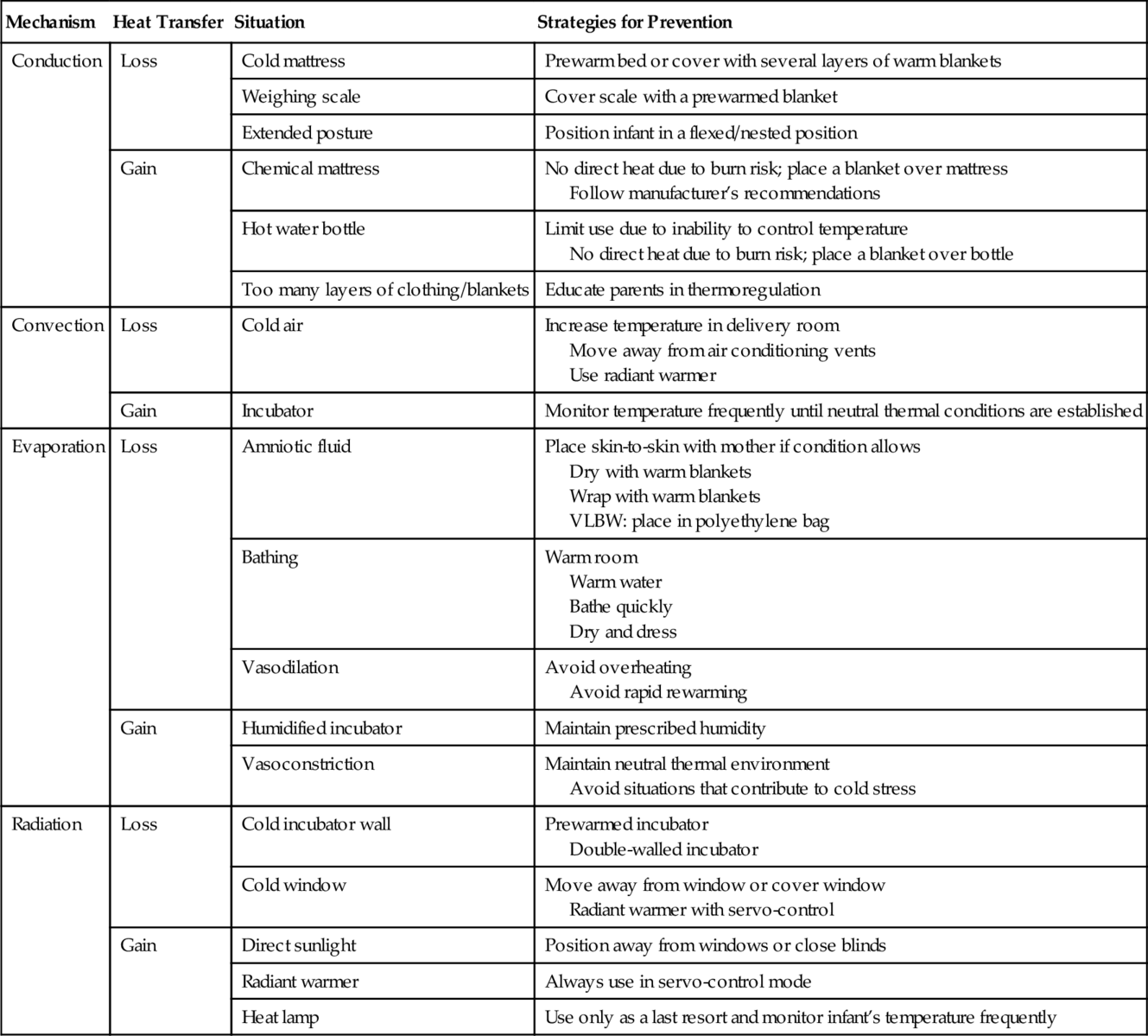
CHAPTER 6 M. Colleen Brand; Holly A. Boyd 1. Discuss the importance of thermoregulation in the care of newborn infants. 2. Compare mechanisms of heat transfer involved in newborn thermoregulation. 3. Identify newborns at increased risk for thermal instability. 4. Recognize symptoms of hypothermia and hyperthermia in neonates. 5. Describe the physiologic processes involved in thermoregulation. 6. Apply strategies for managing the thermal environment. Neonates are the most vulnerable population in regard to temperature control. The smallest and most premature are unable to protect themselves against fluctuations in environmental temperature. Nurses are the first line of defense for this population. It is important that nurses understand the physiology and management of thermoregulation and use their skill and expertise to provide the best environment for these at-risk patients. A. The importance of thermoregulation. b. In the early 1900s, premature babies were displayed at world fairs and expositions in these devices to show small babies previously believed to have very little chance of survival now thriving in this new warmer environment. c. In the 1950s, Silverman demonstrated that hypothermia increased morbidity and mortality (Silverman et al., 1958). More recent studies confirm this finding (Costeloe et al., 2000; Laptook et al., 2007). d. The World Health Organization (WHO) recognizes thermoregulation of the newborn as a major threat to the health of newborns throughout the world (WHO, 1997). e. The term “golden hour” has been used recently in reference to strategies implemented in the delivery room to improve the outcome of neonates. A major focus during the “golden hour” is prevention of heat loss (Bissinger and Annibale, 2010). B. Mechanisms of heat transfer. 1. Heat transfer infers the transfer of heat from warm to cool. There are four mechanisms of heat transfer that affect neonates: conduction, convection, radiation, and evaporation. Table 6-1 lists mechanisms of heat transfer and activities that are associated with heat loss and heat gain as well as strategies to prevent both loss and gain. a. Conduction is the transfer of heat via direct contact. (2) Heat is gained when the neonate comes in contact with a warmer surface such as a chemical warming mattress or warm blankets. (3) The rate of heat transfer varies with the temperature gradient and the amount of skin in contact with the surface. Heat is transferred more readily from the skin to a metal object than from the skin to a cloth surface. b. Convection is heat transfer due to air currents or drafts. (1) Incubators transfer heat to infants through the circulation of warm air (convective heat gain). (2) Heat loss will occur when an infant is exposed to cool air, such as air conditioning, or is placed into an incubator that has not been prewarmed. (3) Heat transfer increases with the temperature gradient between skin and air, with increased airflow, and with increased skin exposure. c. Radiation is the transfer of heat from a warm object to a cooler object that is not in direct contact through infrared energy transfer. Think of standing near a sunny window in summer (heat gain) or a frosty window in winter (heat loss). (1) Radiant warmers provide this type of heat. (2) Heat transfer is affected by the temperature gradient and the distance and angle between the heat source and the skin surface. Radiant heat transfer is not affected by the ambient air temperature or circulating air. (3) If the walls of an incubator are cold, an infant may lose heat and be cold-stressed despite warm air circulating through the incubator (Blackburn, 2013). d. Evaporation is heat transfer due to water vaporizing from the skin or respiratory tract into the drier surrounding air and, in the case of premature infants with thin permeable skin, through transepidermal water loss (TEWL). e. In the delivery room, evaporation of amniotic fluid accounts for 25% of neonatal heat loss (Dahm and James, 1972). f. High total body water, immature skin, and relatively large body surface area result in increased evaporative losses in premature infants. This is even more significant in very low birth weight (VLBW) and especially in extremely low birth weight (ELBW) infants. C. Thermal instability. b. Infants at risk for hypothermia include premature and late preterm infants and infants who have intrauterine growth restriction, are critically ill, are sedated, or have neurologic problems. Infants with open skin defects that place them at risk for increased water loss, such as neural tube or abdominal wall defects, are also at increased risk (American Academy of Pediatrics [AAP] and American College of Obstetricians and Gynecologists [ACOG], 2007; Blackburn, 2013) (Box 6-1). c. Symptoms of hypothermia include apnea, bradycardia, decreased cardiac output, poor oral feeding, feeding intolerance, hypoglycemia, hypotension, hypoxia, irritability, lethargy, weak cry, metabolic acidosis, peripheral vasoconstriction, pulmonary vasoconstriction, and respiratory distress (Box 6-2). d. Poor weight gain may be a symptom of chronic hypothermia due to increased caloric use to attempt to maintain a normal temperature. e. In severe cases of hypothermia, coagulation defects and death may result (Blackburn, 2013). Although shivering is rare, it may be seen in term infants after prolonged cold stress (Bissinger and Annibale, 2010). 2. Hyperthermia. b. Infants at risk for hyperthermia include those with hypermetabolism, including sepsis, cardiac problems, and drug withdrawal, those with dehydration, and infants with central nervous system (CNS) injury or malformation (see Box 6-1). c. Symptoms of hyperthermia include apnea, CNS depression, hypernatremia from dehydration, irritability, lethargy, weak cry, poor oral feeding, seizures, tachycardia, and vasodilation (Brown and Landers, 2011) (see Box 6-2). d. Severe hyperthermia may be associated with seizures and death. 3. Monitoring temperature (Smith et al., 2013). b. It is important to measure the neonate’s temperature accurately in order to assure the temperature is within the normal range and to document the temperature in the medical record to provide data for following temperature trends. c. Axillary temperatures are commonly used in the nursery as they are easy to obtain, are minimally invasive, and correlate well with core temperature. (1) Normal axillary ranges are 36.5° to 37.5°C (97.7° to 99.5°F) for the term neonate and 36.3° to 36.9°C (97.3° to 98.6°F) for the preterm neonate (Brown and Landers, 2011). (2) Electronic or digital thermometers should be used according to the manufacturer’s specifications. d. Rectal temperatures should not be used due to the risk of intestinal perforation and because the core temperature may not decrease until the neonate has totally decompensated. e. Esophageal temperature monitoring may be used to monitor core temperature during therapeutic cooling for HIE or during surgery. f. Continuous skin monitoring is done when servo-controlled equipment is in use. The thermistor should be securely attached to an exposed area of skin with an insulated cover. (a) Desired skin temperatures range from 36° to 37.5°C (96.8° to 99.5°F) (Bissinger and Annibale, 2010; Brown and Landers, 2011; Gomella, 2009; Malin and Baumgart, 1987). (2) Abdominal temperatures greater than 36.5° C are associated with lower oxygen consumption in radiant warmers (Malin and Baumgart, 1987). (3) A study on temperature and heart rate suggests a target of 36.8° to 36.9° C might be more optimal during transition in ELBW infants (Knobel et al., 2010). (4) If both central (abdominal) and peripheral temperatures are monitored, the expected difference is 0.5° to 1° C (Turnbull and Petty, 2013). A difference of 2° C or greater has been associated with cold stress resulting in peripheral vasoconstriction in infants beyond the first day of life (Horns, 2002; Knobel et al., 2009; Lyon et al., 1997; Mok et al., 1991). g. Ear thermometers are fast and easy to use but may be too large for premature infants. If the probe is not placed correctly, the surface temperature may be measured rather than an approximation of core temperature. h. Infrared thermometers, also called temporal artery thermometers, measure the surface temperature without touching the infant by capturing heat radiated from the skin surface. More study is needed before these thermometers are used routinely in neonatal units. 1. The intrauterine temperature may be 0.8° C (1.3° F) greater than the maternal oral temperature (Banerjee et al., 2004). 2. Maternal temperature increases as labor progresses and may increase by an average of 1° C during labor due to physical activity and stimulation of the thermoregulatory center in the hypothalamus (Blackburn, 2013). 3. Epidural anesthesia may also increase the maternal temperature. Temperatures as high as 37.5° to 38°C (99.5° to 100.4° F) have been reported. 4. Neonatal symptoms associated with increased maternal temperature in noninfected women include lower Apgar scores, hypotonia, hypoxia, and an increased need for resuscitation and oxygen at birth (Kattwinkel, 2011). B. Once the infant is delivered, a number of physiologic conditions affect thermal stability, including the physical characteristics of the neonate, metabolic processes, and physical activity. a. Thermal receptors in the skin affect the infant’s response to cold stimuli (Blackburn, 2013). (1) The most prominent and sensitive skin receptors are in the trigeminal area of the face. (2) Stimulation of thermal receptors leads to vasoconstriction as a measure to conserve heat. (3) ELBW infants are unable to respond to hypothermia with vasoconstriction during the first 12 hours after birth (Knobel et al., 2009). b. Neonates have a relatively large surface area–to–body mass ratio, which has an impact on thermoregulation. (1) In term neonates, the surface area–to–body mass ratio is three times greater than that of an adult (Blackburn, 2013). (2) In the preterm infant, the surface area–to–body mass ratio is five to six times greater than that of an adult. The surface area–to–body mass ratio in preterm infants increases as the gestation decreases. c. Premature infants have very thin skin, allowing greater loss of water and heat than seen in term neonates. Thin permeable skin allows water to evaporate from the skin surface. (1) Heat is lost by evaporation. This is known as TEWL (Sedin and Agren, 2006). (2) At 25 weeks of gestation, premature infants can lose 15 times more water through their skin than term neonates. This water loss is inversely proportional to gestational age until about 33 weeks of gestation, when TEWL is similar to that of a term infant (Agren et al., 2006; Sedin and Agren, 2006). d. Posture can affect body temperature by decreasing or increasing surface area for heat loss. (2) Preterm infants lack the muscle tone to maintain a flexed position and rely on caregivers to position them appropriately. e. Thermoregulation in neonates is affected by the type and amount of accumulated fat, which in turn is affected by both gestational age and birth weight. (2) BAT, also known as brown fat, generates more energy than any other tissue in the body and is very important in thermoregulation. (a) Heat production through the metabolism of BAT is regulated by uncoupling protein-1, norepinephrine, and triiodothyronine (Bissinger and Annibale, 2010; Blackburn, 2013). (b) BAT is metabolized during nonshivering thermogenesis (NST) to produce heat. (c) A heavy concentration of blood vessels gives BAT its characteristic brown color and serves to conduct heat into the circulation. (d) Metabolism of BAT involves the breakdown of triglycerides into glycerol and fatty acids and is dependent on the availability of oxygen, glucose, and ATP. If these elements are not available, as is the case during hypoxia, acidosis, and hypoglycemia, heat production will suffer (Cypess and Kahn, 2010). (e) BAT is found around the kidneys and adrenal glands, at the nape of the neck, between the scapulas, in the mediastinum, and around the trachea, heart, lungs, liver, and abdominal aorta. (f) The amount of available BAT is dependent on gestational age (Blackburn, 2013). i. It begins to appear at 25 to 26 weeks, so only a minimal amount is available in VLBW infants. ii. Infants less than 32 weeks of gestation do not have enough BAT to produce significant amounts of heat by NST (Knobel and Holditch-Davis, 2007). iii. BAT increases significantly during the third trimester. iv. BAT continues to increase in the early weeks after birth and is thought to play a role in thermoregulation until a child is approximately 2 years of age. 2. Metabolic processes generate energy by metabolism of fat, including BAT (above), glucose, and protein (Blackburn, 2013). a. NST is the major method of heat production in the neonate. b. NST is triggered when skin temperature decreases to less than 35° to 36° C (95° to 96.8° F). c. NST relies on the availability of BAT and therefore is limited in ELBW infants. d. All metabolically active tissues can generate heat. The organs that generate the greatest amount of energy are the brain, heart, and liver. e. An increase in metabolic rate can produce heat but also leads to an increase in oxygen consumption. This may be a problem in critically ill neonates with borderline oxygenation. f. Term neonates can increase their metabolic rate by 200% to 300% through a combination of metabolic and physical responses (Blackburn, 2013). g. VLBW infants may only be able to increase their metabolic rate by 25%, while ELBW infants may not be able to respond at all. h. Critically ill neonates may not have the reserves of oxygen, glucose, or energy to mount an increase in metabolic rate and adapt to an unstable thermal environment. i. Hypothermia may lead to respiratory distress, hypoglycemia, and the production of lactic acid (see Box 6-2). 3. Physical activity can generate heat, but only late preterm and term infants have enough muscle tone to produce heat by this method and this may only be effective for a short time. b. Neonates receiving sedation, paralytics, or other medications leading to decreased activity or muscle tone may have a blunted response to environmental temperatures outside the normal range. c. Shivering is an involuntary method of heat production that is rarely seen in the neonatal population. The neonate only shivers after prolonged cold stress that leads to decreased spinal cord temperature (Blackburn, 2013). 1. Delivery room management (Bissinger & Annibale, 2010). a. The primary challenge in thermal management of newborns is the prevention of hypothermia because the neonate is expected to transition from a warm, moist environment to a much colder, drier environment. Late preterm and preterm infants are at an increased risk of hypothermia, especially those who are less than 28 weeks of gestation at birth and/or weigh 1500 g or less at birth. A number of strategies have been described to maintain temperature at birth, including warming the room, drying the infant, providing skin-to-skin contact with the mother, utilization of heat loss barriers, use of external heat sources, and use of polyethylene plastic wrap or bag for neonates less than 29 weeks of gestation (Kattwinkel, 2011; McCall et al., 2010). (a) A newborn’s temperature may fall rapidly. The infant’s temperature may drop 0.2° C to 1° C per minute due to evaporative losses from amniotic fluid, convective losses to cooler room air, and radiation to cooler structures in the room such as walls (Blackburn, 2013). (b) The gradient between the ambient room temperature in the delivery room and the infant’s skin temperature promotes heat loss. The delivery room should be maintained above 25° to 26° C (77° to 78.8° F), or at least 26° to 27° C (78° to 80° F) for infants less than 29 weeks of gestation, to minimize convective heat loss (AAP & ACOG, 2012; Hammarlund et al., 1980; Kattwinkel, 2011; Knobel et al., 2005). (2) Dry the infant immediately and remove wet linen (unless using a polyethylene bag) to minimize evaporative heat loss (Bissinger & Annibale, 2010). (a) Use prewarmed absorbent towels to dry the infant gently, taking care not to damage the skin. (b) Use warm blankets and prewarm any surfaces that come in contact with the infant’s skin during stabilization, routine delivery care, and weighing of the infant to minimize conductive heat loss. (3) Avoid drafts to minimize convective heat loss. (4) Skin-to-skin holding. (a) If condition of the infant allows, drying and placing the infant against the mother’s bare skin, then covering with a warm blanket, allows heat from the mother to maintain the infant’s temperature (McCall et al., 2010). (b) Skin-to skin holding can be used in the neonatal intensive care unit as well, even in VLBW infants. The conduction of heat from mother (or father) to the infant is high enough to compensate for increased heat loss through evaporation and convection while the infant is out of the humidified incubator (Karlsson et al., 2012). (5) Barriers to heat loss (Bissinger & Annibale, 2010; McCall et al., 2010). (a) Polyethylene bags or wraps should be used in infants less than 29 weeks of gestation to prevent evaporative heat loss and allow visualization, stabilization, and heat gain through radiation from the radiant warmer. The infant is placed in the wrap immediately and wrapped from the neck to the feet. Only the head is dried. Maintain the wrap until the infant’s temperature is stable in a humidified environment for 1 hour (AAP and ACOG, 2012; Knobel et al., 2005; Trevisanuto et al., 2010; Vohra et al., 2004). (b) Use a polyethylene or insulated cap (not stockinette) after drying the baby’s head to prevent evaporative heat loss (Trevisanuto et al., 2010). (c) Open skin defects (gastroschisis, myelomeningocele) present a major challenge to thermoregulation as the open defect presents a permeable surface for rapid fluid losses and increased evaporative heat loss. Cover the defect with sterile saline-soaked gauze and a sterile waterproof barrier to reduce evaporative losses. (See Chapter 29.) (6) External heat sources. (a) A radiant warmer or prewarmed incubator should be used in the delivery room to maintain the infant’s temperature during routine care and stabilization. Radiant warmers should always be used with a servo-control to prevent overheating (AAP and ACOG, 2012). (b) Chemical mattresses, also called transwarmers, may be used to improve thermal control in VLBW infants. These may be used in the delivery room or during transport and should be removed once the infant is warm and in a stable thermal environment. Because heat is provided by conduction, a blanket should be placed under the neonate to prevent skin burns (AAP and ACOG, 2007, 2012; Brown and Landers, 2011; McCall et al., 2010). (c) Avoid overheating if perinatal asphyxia is suspected. In some cases providing hypothermia strategies to preserve brain function may be appropriate. (See Chapter 34.) (d) Use a prewarmed transport incubator to transfer neonates to the nursery. A transport incubator uses batteries and continues to provide heat during transfer. The incubator usually has equipment built in or attached for monitoring, suctioning, and providing respiratory support and intravenous infusions. 2. Nursery (AAP and ACOG, 2012). a. The temperature in the nursery should be maintained at 22° to 27° C (72° to 78° F) (Bissinger and Annibale, 2010). b. Humidity in the nursery should be maintained at 30% to 60% (Blackfan and Yaglou, 1933). 3. Equipment. b. Incubators. (1) Incubators warm infants using convective heat. (a) Incubator covers can be used to decrease radiant heat loss from incubator walls (Fig. 6-1).
Thermoregulation
INTRODUCTION
PHYSIOLOGY OF THERMOREGULATION
MANAGEMENT OF THE THERMAL ENVIRONMENT


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


6: Thermoregulation
FIGURE 6-1 ■ Incubator with cover. (Courtesy Allen S. Kramer, Texas Children’s Hospital, Houston, Tex.)