Confusion and dementia
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe confusion and its causes.
• List the measures that help confused persons.
• Explain the differences between delirium, depression, and dementia.
• Describe Alzheimer’s disease (AD).
• Describe the signs, symptoms, and behaviors of AD.
• Explain the care required by persons with AD and other dementias.
• Describe the effects of AD on the family.
Key terms
cognitive function Involves memory, thinking, reasoning, ability to understand, judgment, and behavior
delirium A state of sudden, severe confusion and rapid brain changes
delusion A false belief
elopement When a person leaves the center without staff knowledge
hallucination Seeing, hearing, smelling, or feeling something that is not real
pseudodementia False (pseudo) dementia
sundowning Signs, symptoms, and behaviors of AD increase during hours of darkness
KEY ABBREVIATIONS
| AD | Alzheimer’s disease |
| ADL | Activities of daily living |
| NIA | National Institute on Aging |
| OBRA | Omnibus Budget Reconciliation Act of 1987 |
Changes in the brain and nervous system occur with aging (Box 44-1). Certain diseases affect the brain. Changes in the brain can affect cognitive function. (Cognitive relates to knowledge.) Quality of life is affected. Cognitive function involves:
Confusion
Confusion has many causes. Diseases, infections, hearing and vision loss, and medication side effects are some causes. So is brain injury. With aging, blood supply to the brain is reduced. Personality and mental changes can result. Memory and the ability to make good judgments are lost. A person may not know people, the time, or the place. Some people gradually lose the ability to perform daily activities. Behavior changes are common. The person may be angry, restless, depressed, and irritable.
Acute confusion (delirium) occurs suddenly. It is usually temporary. Causes include infection, illness, injury, medications, and surgery. Treatment is aimed at the cause.
Confusion caused by physical changes cannot be cured. Some measures help to improve function (Box 44-2). You must meet the person’s basic needs.
Dementia
Dementia is the loss of cognitive function that interferes with routine personal, social, and occupational activities. (De means from. Mentia means mind.) The person may have changes in personality, mood, or behavior. Dementia is a group of symptoms that may occur with certain diseases or conditions.
Dementia is not a normal part of aging. Most older people do not have dementia. Early warning signs include:
• Recent memory loss that affects job skills
• Problems with common tasks (for example, dressing, cooking, driving)
• Problems with language; forgetting simple words
• Getting lost in familiar places
• Misplacing things and putting things in odd places (for example, putting a watch in the oven)
• Poor or decreased judgment (for example, going outdoors in the snow without shoes)
If changes in the brain have not occurred, some dementias can be reversed. When the cause is removed, so are the signs and symptoms. Treatable causes include:
Permanent dementias result from changes in the brain. They have no cure. Function declines over time. Causes of permanent dementia are listed in Box 44-3. Alzheimer’s disease is the most common type of permanent dementia.
Pseudodementia means false (pseudo) dementia. The person has signs and symptoms of dementia. However, there are no changes in the brain. This can occur with delirium and depression. Both can be mistaken for dementia.
Delirium
Delirium is a state of sudden, severe confusion and rapid brain changes. It occurs with physical or mental illness. Usually temporary and reversible, it is common in older persons with acute or chronic illnesses. Infections, heart and lung diseases, and poor nutrition are common causes. So are hormone disorders. Hypoglycemia is also a cause (Chapter 41). Alcohol and many drugs (including prescription medications) can cause delirium. Delirium often lasts for about 1 week. However, it may take several weeks for normal mental function to return.
Delirium signals physical illness in older persons and in persons with dementia. It is an emergency. The cause must be found and treated. Signs and symptoms are listed in Box 44-4.
Depression
Depression is the most common mental health problem in older persons. It is often overlooked. Depression, aging, and some medication side effects have similar signs and symptoms. See Chapter 43 for signs and symptoms of depression in older persons.
Mild cognitive impairment
Mild cognitive impairment (MCI) is a type of memory change. The person has problems with memory, language, and other mental functions (attention, judgment, reading, writing). The person or others may notice the problems. However, the problems do not interfere with daily life. The person is at risk for Alzheimer’s disease.
Alzheimer’s disease
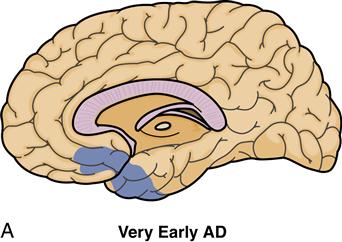
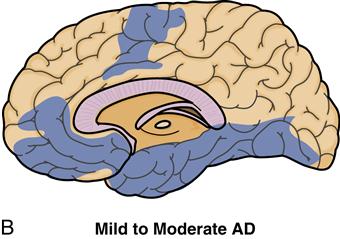
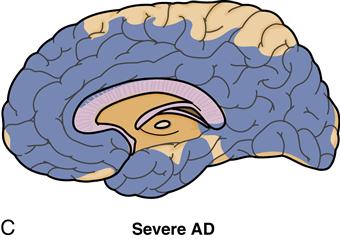
Alzheimer’s disease (AD) is a brain disease. Many nerve cells that control intellectual and social function are damaged and die (Fig. 44-2). These functions are affected:
The person has problems with work and everyday functions. Problems with family and social relationships occur. There is a steady decline in memory and mental function.
The disease is gradual in onset. It gets worse and worse over time. Persons with AD usually live 8 to 10 years after diagnosis. Some persons live as few as 3 years. Others live as long as 20 years. Some people in their 40s and 50s have AD. However, usually symptoms first appear after the age of 60. The risk increases with age. It is often diagnosed around the age of 80. Nearly half of the persons age 85 and older have AD.
The cause is unknown. A family history of AD increases a person’s risk of developing the disease. More women than men have AD. Women live longer than men.
Signs of AD
The classic sign of AD is gradual loss of short-term memory. At first, the only symptom may be forgetfulness. Box 44-5 lists the warning signs and other signs of AD. See Box 44-6 for the difference between AD and normal age-related changes.
Stages of AD
Signs and symptoms become more severe as the disease progresses. The disease ends in death. AD is often described in terms of 3 stages (Box 44-7). See Figure 44-3. The Alzheimer’s Association describes seven stages:
• No impairment. The person does not show signs of memory problems.
Behaviors and problems
AD changes how a person behaves and acts. These changes are common:
• Getting upset, worried, or angry more easily
• Believing other people are hiding things
• Catastrophic reactions (p. 663)
• Agitation and restlessness (p. 663)
• Aggression and combativeness (p. 664)
• Problems with intimacy and sexuality (p. 664)
• Repetitive behaviors (p. 664)
Health-related issues can make the problems worse. Examples include illness, infection, medications, lack of sleep, constipation, hunger, thirst, poor vision or hearing, alcohol, and caffeine. So can problems in the person’s setting. According to the National Institute on Aging (NIA), they include:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree