Urinary and reproductive disorders
Objectives
• Define the key terms and key abbreviations listed in this chapter.
• Describe urinary tract infections and the care required.
• Describe prostate enlargement and the care required.
• Describe urinary diversions and the care required.
• Describe renal calculi and the care required.
• Describe acute and chronic kidney failure and the care required.
• Describe sexually transmitted diseases and the care required.
Key terms
dialysis The process of removing waste products from the blood
dysuria Difficult or painful (dys) urination (uria)
hematuria Blood (hemat) in the urine (uria)
oliguria Scant (olig) urine (uria)
pyuria Pus (py) in the urine (uria)
urinary diversion A new pathway for urine to exit the body
urostomy A surgically created opening (stomy) between a ureter (uro) and the abdomen
KEY ABBREVIATIONS
| AIDS | Acquired immunodeficiency syndrome |
| BPH | Benign prostatic hyperplasia |
| HIV | Human immunodeficiency virus |
| mL | Milliliter |
| STD | Sexually transmitted disease |
| UTI | Urinary tract infection |
Understanding urinary and reproductive disorders gives meaning to the required care. Refer to Chapter 9 while you study this chapter.
Urinary system disorders
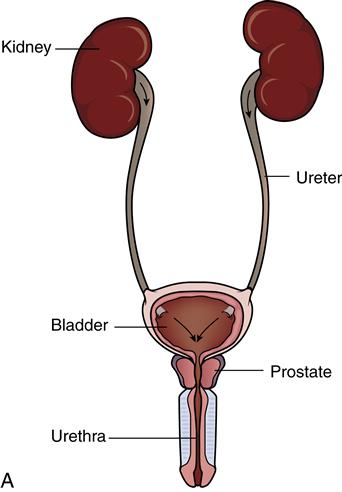
The kidneys, ureters, bladder, and urethra are the major urinary system structures. Disorders can occur in these structures. Men can develop prostate problems.
Urinary tract infections
Urinary tract infections (UTIs) are common. Infection in one area can progress through the entire system. Microbes can enter the system through the urethra. Catheterization, urological exams, intercourse, poor perineal hygiene, immobility, and poor fluid intake are common causes. UTI is a common healthcare-associated infection (Chapter 15).
Women are at high risk. Microbes can easily enter the short female urethra. Prostate gland secretions help protect men from UTIs. However, an enlarged prostate increases the risk of UTI.
Older persons are at high risk for UTIs. Incomplete bladder emptying, perineal soiling from fecal incontinence, poor fluid intake, and poor nutrition increase the risk of UTI in older men and women.
Cystitis
Cystitis is a bladder (cyst) infection (itis) caused by bacteria. These signs and symptoms are common:
• Oliguria—scant (olig) urine (uria)
• Urgency
• Dysuria—difficult or painful (dys) urination (uria)
• Pain or burning on urination
• Hematuria—blood (hemat) in the urine (uria)
• Pyuria—pus (py) in the urine (uria)
• Fever
Antibiotics are ordered. Fluids are encouraged—usually 2000 mL (milliliters) per day. If untreated, cystitis can lead to pyelonephritis.
Pyelonephritis
Pyelonephritis is inflammation (itis) of the kidney (nephr) pelvis (pyelo). Infection is the most common cause. Cloudy urine may contain pus, mucus, and blood. Chills, fever, back pain, and nausea and vomiting occur. So do the signs and symptoms of cystitis. Treatment involves antibiotics and fluids.
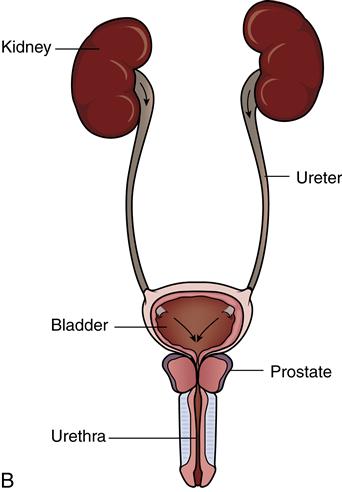
Prostate enlargement
The prostate is a gland in men. It lies in front of the rectum and just below the bladder (Chapter 9). The prostate also surrounds the urethra. In young men, the prostate is about the size of a walnut. The prostate grows larger (enlarges) as the man grows older. This is called benign prostatic hyperplasia (BPH). See Figure 42-1. (Benign means non-malignant. Hyper means excessive. Plasia means formation or development.) Benign prostatic hypertrophy is another name for enlarged prostate. (Trophy means growth.)
Most men age 60 and older have some symptoms of BPH. The enlarged prostate presses against the urethra, obstructing urine flow. Bladder function is gradually lost. These problems are common:
• Frequent voidings of small amounts of urine
• Urgency and leaking or dribbling of urine
• Urinary retention (The man cannot void. Urine remains in the bladder.)
Treatment depends on the extent of the problem. For mild BPH, medications can shrink the prostate or stop its growth. Some microwave and laser treatments destroy excess prostate tissue.
Transurethral resection of the prostate (TURP) is a common surgical procedure. The doctor inserts a lighted scope through the penis. The scope has a wire loop. The loop is used to cut tissue and seal blood vessels. The removed tissue is flushed out of the bladder. A special catheter is inserted and left in place for a few days. Flushing fluid enters the bladder through the catheter. Urine and the flushing fluid flow out of the bladder through the same catheter. Some bleeding and blood clots are normal. After surgery, the person’s care plan may include the following:
• No straining or sudden movements
• Drinking at least 8 cups of water daily to flush the bladder
• No straining to have a bowel movement
• A balanced diet to prevent constipation
Urinary diversions
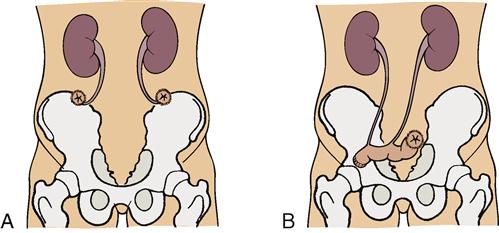
Sometimes the urinary bladder is surgically removed. Cancer and bladder injuries are common reasons. When the bladder is removed, urine must still leave the body. A new pathway—urinary diversion—is needed for urine to exit the body.
Often an ostomy is involved. A urostomy is a surgically created opening (stomy) between a ureter (uro) and the abdomen (Fig. 42-2). The nurse provides care after surgery. You may care for persons with long-standing urostomies. The person assists with care as able.
A pouch is applied over the stoma (Fig. 42-3). Urine drains through the stoma into the pouch. Pouches are changed every 5 to 7 days. A pouch is replaced anytime it leaks. Skin irritation, breakdown, and infection can occur if urine leaks onto the skin.
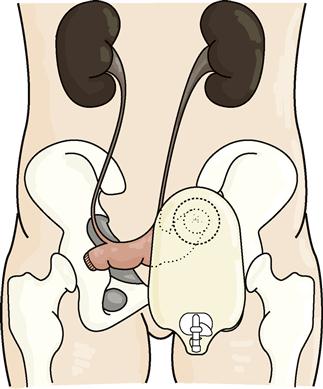
Urine drains constantly into the pouch. Empty pouches every 3 to 4 hours. Or empty them when they are becoming ⅓ (one-third) full. Pouches become heavy as they fill with urine. A heavy pouch can loosen the seal between the pouch and the skin. Urine can leak onto the skin.
The person needs good skin care. You must help prevent skin breakdown. Observe the skin for changes around the stoma. Report changes to the nurse. See “The Person With an Ostomy” in Chapter 23.
See Promoting Safety and Comfort: Urinary Diversions.